Arthrodesis of the Knee
Christopher P. Beauchamp
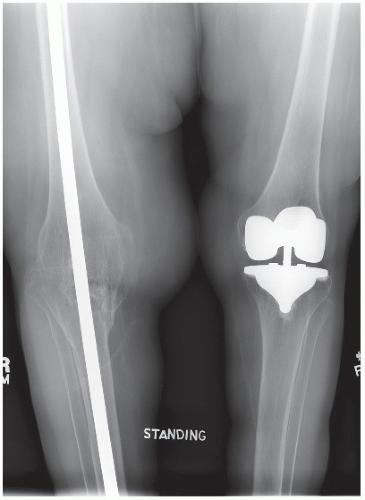
With the availability of modern reconstructive techniques that can achieve a mobile knee reconstruction, knee arthrodesis is now seldom chosen as a primary reconstructive solution. In fact, intra-articular extension of a tumor, necessitating an extra-articular resection, was once considered to be reconstructable only with an arthrodesis. Today, extra-articular resections can sometimes be reconstructed with a mobile knee provided extensor continuity can be maintained. When a fusion is desirable, there are many different ways to successfully achieve it. The techniques described in this chapter all have advantages and disadvantages, There is no single method that is superior to all others. Surgical experience with similar procedures, such as intramedullary nail fixation, may influence the choice of fixation. Plate fixation because of severe obesity may be a preferable choice in certain patients. The following will describe a variety of techniques to achieve a successful arthrodesis.
INDICATIONS
The most common indication today is for salvage of a failed arthroplasty.
Patients who are young, overweight, and have high physical demands can be considered for primary arthrodesis.
An arthrodesis is sometimes chosen for young patients with benign or low-grade malignant neoplasm.
Patients with a quadriceps paralysis and arthritis or a neuropathic joint are also considered candidates for knee fusion
CONTRAINDICATIONS
Acute untreated infections are a contraindication to arthrodesis using plates or rods.
Fusion of the ipsilateral hip or contralateral knee also makes knee arthrodesis an unattractive treatment choice.
PREOPERATIVE PREPARATION
Preoperative planning includes the following:
Radiographic measurement of limb lengths. The ideal final limb length should aim for a discrepancy of 1 to 2 cm. This prevents the foot from brushing against the floor during swing phase.
Plain radiographs with markers or a CT scan are used to determine the canal/IM rod diameter if nail diameter is a potential issue.
CT and MRI are used to calculate the plane of resection for tumors.
Surgical approach is determined by previous incisions or biopsy site. It is generally longitudinal, anterior, medial, or lateral.
Soft tissue coverage is often an issue especially with salvage of an infected prosthesis. Local flaps usually cover most defects about the knee; free tissue transfer is seldom needed.
Infected reconstructions are best treated in two stages. The first stage debriding the joint and removing the prosthesis and inserting an antibiotic spacer. The second stage being the definitive arthrodesis. The assumption being the infection is eradicated after the first stage, and the history of infection does not influence the reconstruction method.
TECHNIQUE
There are a number of reconstructive techniques to achieve a knee fusion. Each method has advantages and disadvantages. There is no single best method and it is helpful to be familiar with all methods of reconstruction. Fortunately, the principles are similar to other orthopedics procedures and this form of reconstructions should be within the capabilities of most orthopedic surgeons.
There are three main techniques including intramedullary fixation with a rod device, external fixation, and internal fixation with plates.
The factors that go into the decision making regarding the particular method include
Age, weight, activity level, infection presence/risk, bone quality, and patient compliance.
The remaining bone stock also is a factor. Arthrodesis for arthritis or failed total knee arthroplasty usually has enough bone in the femur and tibia to permit bone contact at the fusion site. Defects created following tumor resection are most commonly reconstructed with a segmental allograft. In the past autografts, ipsilateral fibula and hemicortical grafts were used to span the defect.
Intramedullary Fixation
There are a number of different devices available for this technique. Resection arthrodesis of the knee for defects secondary to tumor resection has been well described by Enneking and others over the years. Initially, a Kunschner nail or a Sampson nail was used; these were custom made and could be modified in the operating room. Today, most IM nail providers have a long version (Fig. 19.1). These are usually inserted in an antegrade manner. The Sampson rod was extensively used for resection arthrodesis of the knee. It was inserted in a retrograde manner using a perforator adapter that is attached to the proximal end of the rod, and the greater trochanter was penetrated by this beveled tip. The rod was driven proximally through a small incision to allow for the reduction of the knee, and the rod was then driven down the shaft of the tibia. The proximal portion of the rod was curved and the tibial portion was straight. The rod was fluted providing some rotational stability.
There are a number of modular rods. The Neff nail is designed to permit the insertion of a long intramedullary nail through a single knee incision (Fig. 19.2). The rod consists of a femoral and a tibial component so that size differences between the two bones could be accommodated. The two devices are attached to each other via a Morse taper. The device itself could not provide any compression and removal of the implant if necessary is difficult without taking down the fusion. The Wichita nail is also a two piece design with differing diameters in the femur and tibia. The two connect together and a compression nut allows for compression across the arthrodesis site. The femoral and tibial stems are locked allowing compression to be applied (Fig. 19.3).