Triple Arthrodesis
Keywords
• Triple arthrodesis • Traumatic arthritis • Degenerative joint disease • Tarsal coalitions
Indications
Edwin W. Ryerson first described triple arthrodesis in 1923 as a fusion of the talocalcaneal, talonavicular, and calcaneal cuboid joints.1 The goal was to create a well-aligned, plantigrade, and stable foot for patients with deformity or progressive neurologic and arthritic conditions. This procedure should be reserved for instances when all conservative measures have been tried and failed, and a more limited surgical procedure will not afford appropriate pain relief and reduction of the deformity. In cases of a flexible deformity, consideration should first be given to those procedures that are joint sparing, such as tendon transfers or osteotomies.
The following is a list of indications for triple arthrodesis:
Contraindications
Advanced age and diabetes mellitus are not direct contraindications for triple arthrodesis, although it has implications for the postoperative care regimen.3 Proper control of blood sugar is necessary to allow an optimal postoperative course.
Physiology and pathomechanics
Preoperative valgus mechanical alignment and preoperative varus tibial alignment have an effect on the ultimate position of the foot after triple arthrodesis. Even if the tibial malalignment is not corrected, foot malalignment can be avoided, because the foot has been placed in a plantigrade position with respect to the preexisting proximal lower alignment. This concept comes into play when a patient is to undergo later correction of deformity at the knee joint, because the foot has already been placed in a plantigrade position relative to the original deformity of the tibial mechanical axis. Therefore, in cases such as this, the patient may require revision for correct alignment of the hindfoot.3
Radiographic evaluation
All patients should have weight-bearing radiographs of their feet and ankles: anteroposterior foot, lateral foot, and anteroposterior ankle views. Oblique foot and a mortise view may be taken as well to facilitate preoperative evaluation. Talar head uncovering is seen on anteroposterior view in patients with planovalgus deformity (Fig. 2). These patients also display divergence of the talocalcaneal angle on both the anteroposterior and lateral views. Conversely, these angles tend to be parallel or converge in patients with cavus foot type. The anteroposterior view of the ankle can be used to evaluate any degenerative joint disease, talar tilt, or to visualize calcaneal fibular impingement that is seen with flatfoot deformity.5
Surgical technique
Preferably a tourniquet is placed around the upper calf region. Generous soft roll underpadding is placed around the undersurface of the tourniquet, particularly surrounding the course of the peroneal nerve as it wraps around the fibular head to impart adequate protection. This technique allows for the use of lower cuff pressures, typically around 250 mm Hg, compared with higher thigh tourniquets. Standard lower extremity surgical prep and draping may be used. The toes and forefoot may be covered using a surgical glove or iodine adhesive plastic to prevent contamination from debris from the toenails. Appropriate preoperative antibiotic therapy is advocated.3
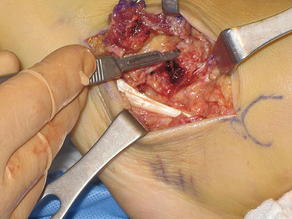
Lateral dissection is typically initiated first. The peroneal tendons should be identified running along the lateral inferior aspect of the calcaneus and calcaneal cuboid articulation and retracted inferiorly. Next, the extensor digitorum brevis muscle belly is identified. The deep fascial, capsular, and periosteal tissues overlying the subtalar and calcaneal cuboid joint are opened simultaneously as 1 layer through and inverted-L–shaped flap. The flap is then reflected distally. There may be a large venous plexus along the distal extent of the extensor digitorum brevis muscle belly, so care should be taken to achieve proper hemostasis to prevent possible postoperative complications. The sinus tarsi may now be visualized (Fig. 3). The contents of the sinus tarsi are evacuated by using a hand rongeur or by placing a #15 blade along the osseous constraints of the talus and calcaneus and carefully moving the blade in a circular fashion. Care should be taken that all intertarsal ligaments are removed to allow the calcaneus to be reduced from its valgus position. Visualization of the posterior facet of the subtalar joint can now be made through the void in the sinus tarsi. A lamina spreader is then placed within the subtalar joint to allow wider exposure (Fig. 4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree