40. Antibacterial therapy
principles
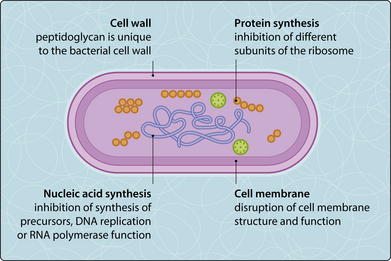
Antibacterial drugs may be classified by their spectrum of antibacterial activity (Ch. 41) or their target site of action (Fig. 3.40.1 and Table 3.40.1).
Table 3.40.1 CLASSES OF ANTIBACTERIAL DRUG
| Target site and class | Examples | Comments/adverse reactions |
|---|---|---|
| Cell wall (β-lactams) | ||
| Penicillins (β-lactams) | Benzylpenicillin, ampicillin | Generally safe but allergic reactions |
| Cephalosporins (β-lactams) | Cephalexin, cefuroxime, ceftazidime | Broad-spectrum: overusage promotes resistance |
| Carbapenems (β-lactams) | Imipenem, meropenem | Reserved for resistant pathogens |
| Glycopeptides | Vancomycin, teicoplanin | Vancomycin may be nephro/oto-toxic, assay required |
| Protein synthesis | ||
| Aminoglycosides | Gentamicin, amikacin | Potential nephro- and oto-toxicity; assay required |
| Tetracyclines | Tetracycline, doxycycline | Stain teeth and bone |
| Chloramphenicol | Chloramphenicol | Potential marrow toxicity |
| Macrolides | Erythromycin | Often used in penicillin-allergic patients |
| Lincosamides | Clindamycin | Associated with pseudomembranous colitis |
| Fusidic acidOxazolidinones | Fusidic acidLinezolid | May cause jaundiceMay cause myelosuppression |
| Nucleic acid synthesis | ||
| Sulphonamides | Sulfamethoxazole | Rarely used because of toxic reactions |
| Trimethoprim | Trimethoprim | Mainly used in treatment of UTI |
| Quinolones | Nalidixic acid, ciprofloxacin | Early quinolones have limited Gram-positive activity |
| Rifamycins | Rifampicin | Stains tears/urine, may cause jaundice |
| NitroimidazolesNitrofurans | MetronidazoleNitrofurantoin | Antabuse effect with alcoholUrinary activity only |
| Cell membrane function | ||
| Polymyxins | Colistin | Used for bowel decontamination or by inhalation |
| Cyclic lipopeptide | Daptomycin | May cause rhabdomyolysis |
| Ethambutol | Visual changes |
UTI, urinary tract infection.
Agents that inhibit bacterial growth are termed bacteriostatic, whereas those that kill bacteria are termed bactericidal. For many agents, bactericidal activity is species dependent and generally not essential except in some immunosuppressed individuals and in endocarditis. However classification by pharmacodynamic properties, such as concentration- or time-dependent killing, is coming into use for dosage decisions (Ch. 41).
Antimicrobial resistance
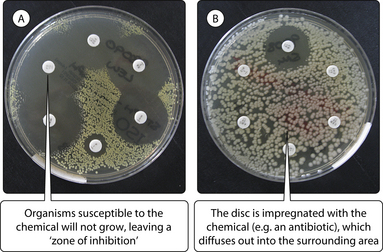
A bacterium is considered resistant to a certain agent when bacterial growth cannot be inhibited by achievable serum concentrations of the agent. The minimal inhibitory concentration (MIC) is the antibiotic concentration required to suppress visible growth. In diagnostic microbiology laboratories, the disc diffusion method is used to determine resistance, whereby a certain diameter for the inhibition zone corresponds to the MIC (Fig. 3.40.2). Some bacteria show inherent or innate resistance to certain antibiotics (e.g. Pseudomonas aeruginosa is always resistant to benzylpenicillin). Other bacteria have acquired resistance as a result of genetic change. Resistance may result from chromosomal mutation or transformation (Fig. 3.40.3). Spontaneous mutation of the chromosome may change protein synthesis to create bacteria that have a selective advantage and will, therefore, outgrow the susceptible population. Certain species such as Streptococcus viridans, Neisseria and Haemophilus spp. can pick up genes from dead bacteria and transform their corresponding gene with the newly acquired DNA sequence, resulting, for example, in penicillin-resistant pneumococci.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree