Anteromedial Tibial Tubercle Transfer
John P. Fulkerson
INDICATIONS/CONTRAINDICATIONS
The best candidate for anteromedial tibial tubercle transfer (2,5,6) (Fig. 3-1) is a patient with lateral patellar tilt (and/or subluxation) associated with grade III or IV articular degeneration localized on the lateral and/or distal medial patellar facets following the failure of nonsurgical therapy. If there is no articular degeneration or pain, there is no need to anteriorize the tibial tubercle, and a straight medial transfer of the tibial tubercle as described by Trillat (11) and reviewed by Carney, Mologne, Muldoon, and Cox (1) is more appropriate for correcting subluxation. However, some patients have distal and/or lateral patella articular softening (grade I) or cartilage breakdown (grade II-IV).
In such patients, the surgeon may wish to anteriorize the extensor mechanism to some extent at the time of realignment. An oblique osteotomy will transfer load off an area of articular degeneration, particularly when damage is noted on the distal aspect of the patella (anteriorization “tips” up the distal patella, thereby unloading it). Anteromedial tibial tubercle transfer is appropriate whenever the surgeon wishes to shift contact stress on the patella from the lateral and distal aspects of the patella to the more proximal and medial patellar articular cartilage. Most important is to recognize that tibial tubercle anteriorization at the time of medialization gives the added benefit of removing articulation with the distal patella, which is often a fragmented or softened source of pain.
Before considering anteromedial tibial tubercle transfer, alternative nonsurgical treatment methods must fail. In particular, a well-structured program of rehabilitation should be tried involving mobilization of a lateralized and tight extensor mechanism supplemented by patellar bracing (9). I use the TruPull braces (DJOrtho, Vista, CA). A tight extensor mechanism and hamstrings should be mobilized through stretching and strengthening. Prone quadriceps stretching has been very helpful and is easy for patients to do at home. Lower extremity core stability including hip stabilization exercises is important in these patients. Nonsteroidal anti-inflammatory medication is often helpful for symptomatic treatment during the period of nonsurgical therapy.
Failed lateral release is another potential indication for anteromedial tibial tubercle transfer. If a patient is left with residual articular pain or symptomatic lateral malalignment of the patella following lateral release, anteromedial tibial tubercle transfer may be helpful.
Contraindications to anteromedial tibial tubercle transfer include:
Diffuse patella articular breakdown. Particularly if the cartilage loss involves the proximal medial patella (dashboard or crush injury), patients are less likely to benefit from anteromedial tibial tubercle transfer.
Tilt alone and no significant subluxation or lateral facet collapse. Such patients may benefit from simple lateral retinacular release; therefore anteromedial tibial tubercle transfer is not recommended as a first procedure.
Reflex sympathetic dystrophy and chronic pain syndrome.
Patients with a bleeding tendency or history of deep venous thrombosis are less desirable candidates for this type of surgery.
Poor healing capacity, diabetes, gross obesity, and smoking are relative contraindications for tibial tubercle transfer.
PREOPERATIVE PLANNING
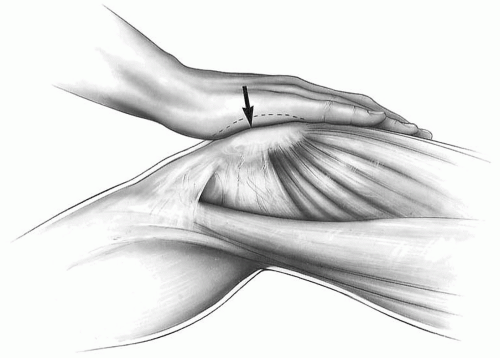
Clinical examination is important in preoperative planning for anteromedial tibial tubercle transfer. The examination should include compression of the patella while flexing and extending the knee to see if articular pain can be elicited (Fig. 3-2). The examining surgeon should also rule out other nonarticular causes of pain such as neuroma, isolated retinacular pain, patellar tendonitis, referred pain, plica, meniscus derangement, synovitis, and osteochondritis dissecans. The physical examination should be done with the patient in both standing and supine positions. The examiner should look for evidence of lateralization of the extensor mechanism and tilt. Passive patellar tilt and tightness of the lateral retinaculum should be noted (2). Pain on compression of the patella with flexion and extension of the knee is likely to have an articular source. If this is associated with lateralization and lateral tilt of the patella, the patient may be a candidate for anteromedial tibial tubercle transfer, particularly if the compression pain is prominent in early knee flexion, indicating a distal patella articular lesion that will be completely unloaded on anteriorization of the tibial tubercle. It is important to be certain that pain is not due to a retinacular neuroma, painful scar, or intra-articular cause that might be corrected by a smaller surgical procedure or injection.
Standard anteroposterior and lateral radiographs should be taken on all surgical candidates and supplemented with an axial (tangential) view. A standard axial (10) view (knee flexed 45 degrees and x-ray beam 30 degrees from the horizontal plane) provides a good idea of patella orientation in the trochlea and is our view of choice. If a specific malalignment pattern is identifiable on the axial radiograph, no further radiographic evaluation is necessary. On the other hand, some patients with significant malalignment of the extensor mechanism will demonstrate a normal axial radiograph yet have significant lateral subluxation and/or tilt on computed tomography (CT) of the patellofemoral joint.
A true lateral radiograph of the knee (posterior condyles superimposed) at 0 and 30 degrees knee flexion will help greatly in understanding trochlea morphology from top to bottom.
CT of the patellofemoral joint should be done with normal standing alignment of the patient reproduced in the scanner gantry. Midpatellar transverse tomographic images should be made with the
CT cut directed to include the posterior condyles of the femur (Fig. 3-3). These tomographic slices should be taken with the knees flexed 15, 30, and 45 degrees (5). The patella is significantly tilted if the patellar tilt angle (the angle created by lines drawn along the lateral facet of the patella and the posterior femoral condyles) is less than 12 degrees on the tomographic image with the knee flexed 15 degrees. The patella should be centered in the trochlea on the tomographic image in which the knee is flexed at 15 degrees. (In other words, the congruence angle [10] should be 0 or slightly negative). Furthermore, CT provides an ideal opportunity to understand the relationship of the tibial tubercle to the central trochlea (TT-TG index as described by Goutallier [7]). As the TT-TG index rises, TT transfer becomes increasingly desirable, particularly when it exceeds 20 mm.
CT cut directed to include the posterior condyles of the femur (Fig. 3-3). These tomographic slices should be taken with the knees flexed 15, 30, and 45 degrees (5). The patella is significantly tilted if the patellar tilt angle (the angle created by lines drawn along the lateral facet of the patella and the posterior femoral condyles) is less than 12 degrees on the tomographic image with the knee flexed 15 degrees. The patella should be centered in the trochlea on the tomographic image in which the knee is flexed at 15 degrees. (In other words, the congruence angle [10] should be 0 or slightly negative). Furthermore, CT provides an ideal opportunity to understand the relationship of the tibial tubercle to the central trochlea (TT-TG index as described by Goutallier [7]). As the TT-TG index rises, TT transfer becomes increasingly desirable, particularly when it exceeds 20 mm.
Following full clinical evaluation and radiographic study, the surgeon will know whether the patella is malaligned and will have some idea of the degree of articular degeneration, particularly as demonstrated by pain and crepitation on flexion/extension of the knee while compressing the patella. If appropriate nonsurgical treatment has failed, the patient may be a candidate for anteromedial tibial tubercle transfer, given significant malalignment (tilt and/or subluxation) and evidence of pain coming from the patellar articular surface (particularly if articular degeneration is distal and/or lateral).
SURGERY
The patient is positioned supine on the operating room table, and the anesthesiologist may apply a percutaneous nerve stimulator over the femoral nerve at the groin level. A tourniquet is applied on the proximal thigh and the patient is prepped from the tourniquet level down to and including the toes. Impermeable drapes are used.
Technique
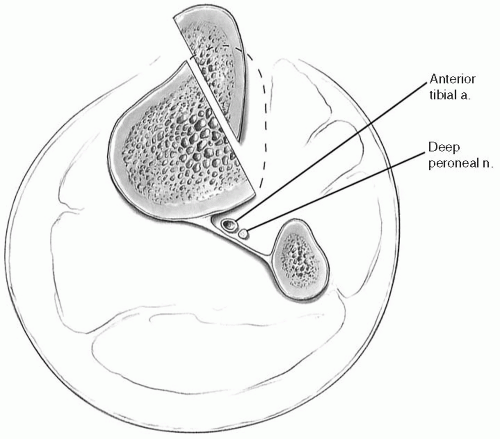
An arthroscopy is routine at the outset of anteromedial tibial tubercle transfer. A superomedial portal, two finger-breadths above the medial proximal pole of the patella, allows an excellent view of the patellar articular surfaces (Fig. 3-4), but standard arthroscopic evaluation using medial and lateral infrapatellar portals is often sufficient. By distending the knee to 60 mm Hg pressure, the surgeon can determine the extent of articular damage as well as the extent and location of articular breakdown. Reducing the fluid inflow pressure gives an idea of the extent of patellar subluxation and/or tilt with flexion and extension of the knee. The femoral nerve may be stimulated (to brief tetany) with the knee in progressive flexion to help determine the dynamic alignment/malalignment. The arthroscopy is completed through an infrapatellarportal to evaluate the rest of the knee and to confirm the patellar findings noted if a proximal approach was used.
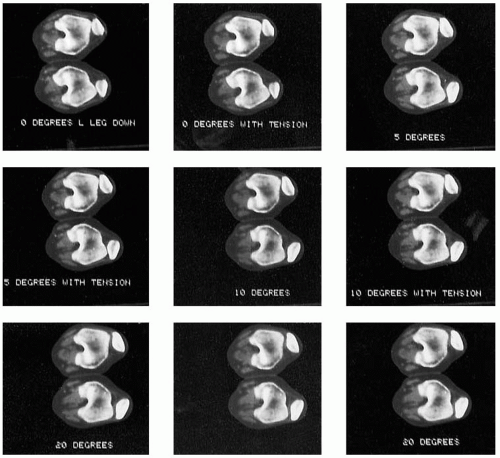 FIGURE 3-3 Computed tomographic imaging of the patellofemoral joint should include precise midpatellar transverse cuts directed through the posterior femoral condyles. |
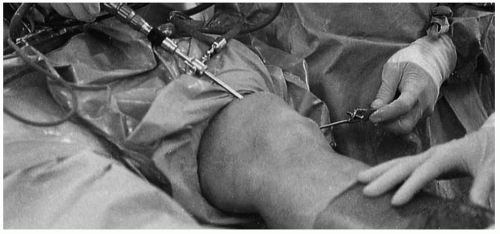 FIGURE 3-4 Arthroscopy of the patellofemoral joint using the superomedial approach gives an excellent view of the entire patellar articular surface as well as the medial and lateral recesses. |
The surgeon must first characterize and document (by print or video) the nature and location of any articular lesion. A precise description of all articular lesions and their location should be dictated later in the operation report.
Loose flaps of articular cartilage or fibrillated cartilage can be removed most easily at the time of arthroscopy. Abrasion or resection of exposed sclerotic bone can also be done at the time of arthroscopy or with the knee open at the time of anteromedial tibial tubercle transfer. Drilling of the patella is best accomplished after lateral release. Debridement of inflamed synovium, preferably using cautery, and removal of loose bodies are best accomplished arthroscopically.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree