Anterior Thoracolumbar Extensile Approach
Robert A. McGuire Jr.
INDICATIONS/CONTRAINDICATIONS
The extensile approach is used to gain access to the lower thoracic spine and lumbar spine simultaneously. This approach allows spinal access for anterior soft tissue release and correction of deformities with instrumentation in the anterior position alone (5). It is also used for treatment of thoracolumbar fractures, either acute or chronic. In many patients with chronic fractures, kyphosis is often present as a result of the fracture. The extensile approach allows excellent visualization of the anterior column of the spine in a circumferential manner. This allows surgical release of the anterior soft tissue-deforming structures (such as the annulus and the anterior longitudinal ligament), vertebrectomy, and correction of the deformity. Correction of the kyphosis, reconstruction of the vertebra with placement of a graft, and anterior stabilization can be easily accomplished through this approach.
PREOPERATIVE PREPARATION
The approach can be made from either the right or the left side. The goals of the surgical procedure and the side of major pathology often dictate which side is used. If an anterior release is all that is
necessary; it is most often worthwhile to work on the convex portion of the curve. It is often very difficult to work in the concave side and achieve an adequate and complete soft tissue release. For fracture decompression, reduction, and stabilization, both the right and the left sides can be used according to the surgeon’s preference. Because the arterial vessels lie most often on the left side of the spine, it is often easier to approach from the left in order to mobilize the vessels and minimize risk to the inferior vena cava. It is worthwhile to determine whether there are any preexisting problems related to the pulmonary cavity, such as fibrosis from old respiratory diseases or previous abdominal procedures, that could make the approach more difficult. This extensile approach allows exposure from the distal thoracic spine all the way to the sacrum if needed.
necessary; it is most often worthwhile to work on the convex portion of the curve. It is often very difficult to work in the concave side and achieve an adequate and complete soft tissue release. For fracture decompression, reduction, and stabilization, both the right and the left sides can be used according to the surgeon’s preference. Because the arterial vessels lie most often on the left side of the spine, it is often easier to approach from the left in order to mobilize the vessels and minimize risk to the inferior vena cava. It is worthwhile to determine whether there are any preexisting problems related to the pulmonary cavity, such as fibrosis from old respiratory diseases or previous abdominal procedures, that could make the approach more difficult. This extensile approach allows exposure from the distal thoracic spine all the way to the sacrum if needed.
Technique
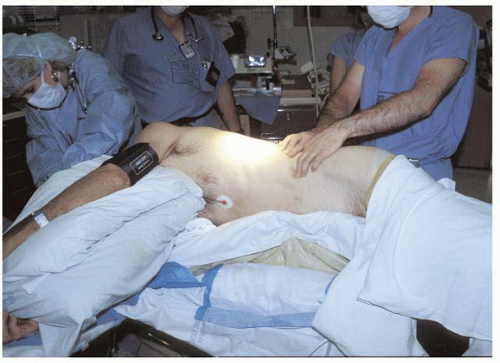
Positioning of the patient is critical when this approach is used. Planning should be discussed with the anesthesia team because the use of a double-lumen endotracheal tube can be extremely helpful in minimizing problems with the lung. The use of the double-lumen endotracheal tube allows the lung to be deflated, which assists in visualization of the surgical field and still allows the patient to be adequately ventilated. This is most helpful for procedures at T9 and above. When the patient is positioned, great care must be undertaken to adequately pad all of the bony prominences around the knees, hips, and ankles (Fig. 13-1). An axillary roll should also be placed to minimize injury to the brachial plexus. The use of a vacuum-formed beanbag stabilizer provides individualized support and stability on the operating table and allows intraoperative radiographs to be taken (Fig. 13-2). Stability can also be augmented with the use of 3-inch-wide tape secured to the operating table on one side, brought over the shoulder and hip, and then secured to the opposite side of the table. It is preferable to flex the hip in order to relax the psoas muscle. A Foley catheter and a nasogastric tube are inserted to decompress the bladder and minimize the risk of intra-abdominal gas formation from the anesthetic. If the iliac crest is to be used for bone harvesting, draping of the surgical site should be performed in such a manner as to allow exposure of the crest. Once the patient is securely stabilized on the table, the surgical site is draped and the skin sterilely prepped.
Surgical Procedure
The incision can be made through the 9th, 10th, or 11th rib, depending on the length of exposure needed in the thoracic region. Once the determination of the rib level is made, the proposed skin incision is drawn over this rib, beginning posteriorly and extending anteriorly and distally to the level of the pubic symphysis if necessary. It can be made in a curvilinear manner, which would allow full exposure of the distal thoracic and lumbar spine as needed (Fig. 13-3). The skin incision is then made sharply through the skin and subcutaneous tissues.
The latissimus dorsi muscle is split, as is the posterior serratus if necessary, which exposes the rib (Fig. 13-4). The rib can also be used as bone graft. The rib periosteum is split, and the rib is then removed in a subperiosteal manner. It is important to make the incision of the periosteum in the cephalad half of the rib to prevent injury to the neurovascular bundle, which lies in the rib groove caudally.
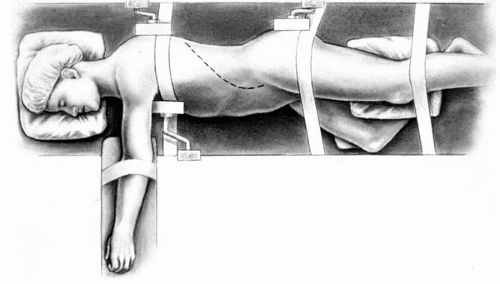 FIGURE 13-1 Positioning the patient in the appropriate manner allows good visualization of the surgical site and allows all bony pressure areas to be adequately protected. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree