Anterior Thoracic Approach
Morgan N. Chen
Samuel C. Overley
Sheeraz A. Qureshi
Andrew C. Hecht
DEFINITION
The anterior approach can be used to access the thoracic spine for decompression, deformity correction, and stabilization.
This approach allows for access to treat conditions such as intervertebral disc herniation, infection, tumor, and trauma.1
ANATOMY
The thoracic spinal cord may have a tenuous blood supply, particularly in patients with congenital anomalies and kyphosis.
The midthoracic cord represents a watershed zone for vascularity. The artery of Adamkiewicz supplies the thoracic cord but can have a variable origin. Its origin is usually (80%) from the left side at the T10 level but can vary from T5 to L5.2
Because of the thoracic spine’s tenuous blood supply and the potential for anterior spinal artery compression caused by thoracic disc herniations, indirect approaches were developed, obviating the need for wide laminectomy and direct visualization of the cord. The goal of these techniques, including the posterolateral transpedicular and transthoracic anterior approaches, is to minimize direct cord manipulation via retraction and prevent subsequent microcontusion and cord ischemia.
SURGICAL MANAGEMENT
Preoperative Planning
Location of pathology is a key element to choosing the optimal approach to the thoracic spine.
In terms of disc pathology, evidence has shown that more axially located disc herniations are better treated with an anterior approach, whereas a posterolateral approach is better suited for lateral or foraminal disc herniations.
Radiographs of the thoracic spine and chest should be obtained to determine the level of surgery and help in “rib counting.”
It is often helpful to obtain lumbar radiographs also to determine the number of lumbar segments below the most distal thoracic rib. Knowing this information preoperatively helps in counting “up” from the sacrum intraoperatively if needed.
In the absence of obvious bony pathology such as fractures, infections, or tumors, it is very easy to inadvertently localize the wrong level in the thoracic spine. The surgeon should be sure to have a strategy for intraoperative level identification based on careful scrutiny of radiographs and magnetic resonance imaging (MRI) or computed tomography (CT) scans before surgery, understanding that the quality of intraoperative fluoroscopy may not be optimal.
When obtaining an MRI to better understand the nature of the pathology in relation to the thoracic spinal cord, the surgeon should ask for a topogram to be performed so that there is no question as to the level or levels of involvement.
On CT or MRI scans, the surgeon should pay close attention to the position of the aorta and inferior vena cava, especially on the axial cuts, as this may affect the side from which the spine is approached, especially if a corpectomy will be performed.
Anesthesia considerations include the use of an oral gastric tube and double-lumen endotracheal tube, which allows for collapse of the ipsilateral lung.
If the surgical site is T10 or caudal, selective deflation of the ipsilateral lung is usually not necessary. Additionally, a left-sided approach may prove more advantageous at the thoracolumbar junction, as the elevated right hemidiaphragm may prevent adequate exposure.
If the surgical site is proximal to T10, selective deflation is helpful in keeping the lung out of the field, but it may lead to more postoperative issues with atelectasis.
We routinely use neurologic monitoring when performing thoracic operations.
Positioning
The patient should be in the lateral decubitus position with the arms in prayer position.
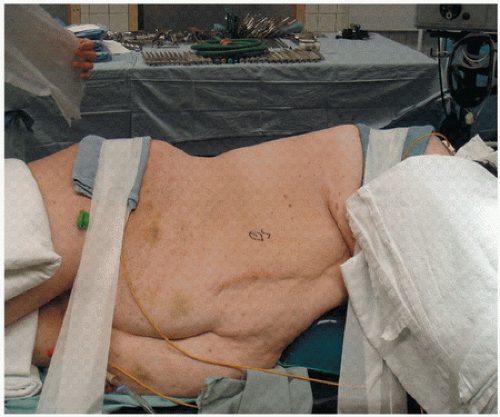
The thorax vertex should be positioned over the break of the bed, all pressure points should be padded, pillows should be placed between legs and arms, and an axillary roll should be used to prevent compression of the axillary vessels (FIG 1).
Approach (Right versus Left)
Considerations for thoracic approaches include the following:
Approach from the side of herniation in cases of posterolateral or lateral herniation.
Look at the axial CT or MRI scans to determine the location of the heart and great vessels. In most thoracic cases, these structures are either on the left or central. Thus, all other factors being equal, a right-sided approach is favored in most cases.
In the distal thoracic spine (eg, T10-T12), the elevated right hemidiaphragm and liver may be in the way of a right-sided approach. Because it is a bit more difficult to retract the liver than the kidney or spleen, a left-sided approach may be favorable.
Considerations for thoracolumbar approaches include the following:
The left-sided approach is generally favored, as it is easier to mobilize the great arteries (aorta, iliacs) from their left central position to the right rather than mobilizing the great veins (which tend to be further to the right).
TECHNIQUES
▪ Anterior Thoracic Approach from T1 to T4
For upper thoracic exposures, a right-sided approach is preferred to avoid the heart.
The surgeon makes a curved skin incision below the tip of the scapula (TECH FIG 1A).
This incision is carried down to the latissimus dorsi muscle and then the latissimus is incised, leaving a cuff of the muscle on the scapula for later closure (TECH FIG 1B).
A large retractor (ie, Richardson retractor) can then be held by the assistant while the surgeon incises the periosteum over the appropriate rib and then resects the rib as far anteriorly and posteriorly as possible (TECH FIG 1C).
At this point, the chest is entered through the rib bed and a Finochietto or Omni retractor can be placed, with one of the blades holding the scapula up and out of the way.
Now the lung can be deflated and retracted anteriorly and inferiorly (TECH FIG 1D).
The pleura overlying the spine is now sharply incised. Placing suture into the edges of the pleura makes subsequent closure easier.
Segmental vessels are identified and ligated as needed, and the vertebral bodies (the “valleys”) and disc spaces (the “hills”) are identified.
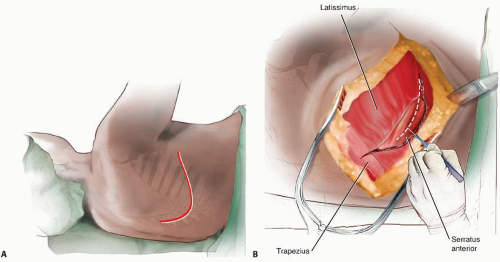 TECH FIG 1 • Anterior thoracic approach from T1 to T4. A. A curved incision should be made just under the tip of the scapula. B. The incision is carried down to the latissimus dorsi. A cuff of muscle is left attached to the scapula for repair upon closure. (continued)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|