Anterior Shoulder Instability: Suture Plication
Robert M. Lucas
Anthony A. Romeo
Scot A. Youngblood
Neil Ghodadra
Matthew T. Provencher
Disclaimer: The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States government.
Anterior instability is the most common type of shoulder instability with an estimated incidence of 2% for traumatic anterior dislocation over the lifetime of the general population. It can lead to significant functional disability and decreased quality of life. Numerous anatomic lesions can be responsible, including disruption of the glenoid labrum from its attachment at the glenoid, stretching or disruption of the glenohumeral ligaments, poor dynamic control of the shoulder girdle, rotator cuff tears, and osseous lesions of the glenoid rim and humeral head. By arthroscopically repairing the pathology present in the capsuloligamentous complex and glenoid labrum, the biomechanics of the glenohumeral joint are reliably restored (1, 2).
Open repair of the unstable shoulder has previously been considered the gold standard given its high success rate. However, recent advances in arthroscopic procedures have shown that if performed correctly, arthroscopic repair of shoulder instability can equal the success of open repair. Arthroscopic stabilization by suture anchor fixation with capsular plication has shown failure rates ranging from 5% to 11%, comparable with open repair (3). Arthroscopic repair has several advantages over open repair, including reduced postoperative morbidity and pain, shorter hospitalization, improved range of motion, more complete inspection of the glenohumeral joint, and less damage to surrounding soft tissue, including the subscapularis tendon. However, certain cases of anterior instability repair, especially those patients with significant bony deficiencies, are better approached by an open technique (4). The keys to the successful arthroscopic treatment of anterior shoulder instability are to first properly identify pathology amenable to arthroscopic repair and then ensure that the capsulolabral structures are adequately repaired and tensioned to the glenoid.
PATHOLOGY
Biomechanically, the glenohumeral joint is a shallow ball and socket joint with stability maintained by both static and dynamic anatomic mechanisms. The dynamic stabilizers consist of the muscle-tendon units of the rotator cuff, tendon of the long head of the biceps, superficial muscle layer, and scapulothoracic muscles. Static stabilizers include the concavity of the glenoid fossa, adhesion- cohesive properties of synovial fluid, negative intra-articular pressure, and soft tissue structures consisting of the glenoid labrum and capsular ligaments. The glenohumeral capsuloligamentous complex consists of collagenous bands, which originate from the glenoid labrum and attach to the humerus. They serve to statically restrain the glenohumeral joint against excessive translation in varying positions of arm rotation and may also have a proprioceptive role in shoulder stability. The anterior band of the inferior glenohumeral ligament (IGHL) attaches to the glenoid at the anteroinferior labrum and is the primary static restraint to anterior translation in the abducted and externally rotated shoulder.
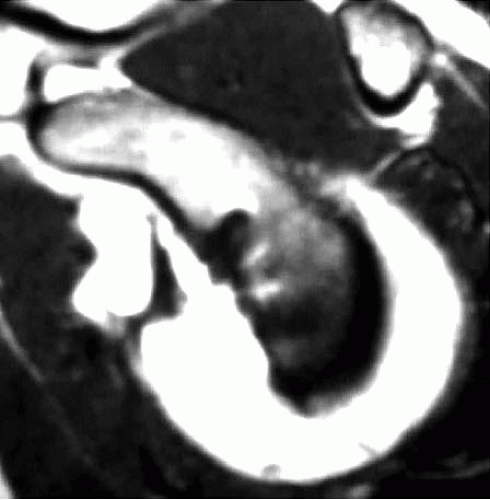
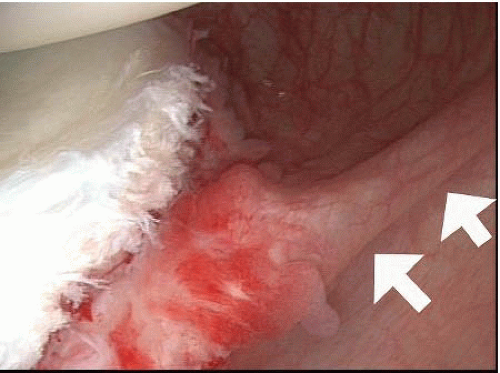
The glenoid labrum is a fibrocartilaginous ring, which lines the glenoid fossa and is a critical static stabilizer of the shoulder (Fig. 17.1). The labrum itself acts to support the glenohumeral joint by increasing the surface area and concavity of the joint and by acting as a bumper to prevent translation of the humerus on the glenoid. It also serves as a fibrocartilage transition zone where the glenohumeral ligaments and long head of the biceps tendon attach to the glenoid rim. The Bankart lesion, which is an avulsion of the anterior inferior glenoid labrum from the bony glenoid rim, is commonly encountered in anterior shoulder instability and often involves a fracture of a piece of the inferior glenoid (Fig. 17.2). As mentioned, the anterior band of the IGHL attaches to the glenoid at the anteroinferior labrum, and disruption of this attachment can lead to excessive anterior humeral translation. It is often disrupted during a traumatic dislocation event.
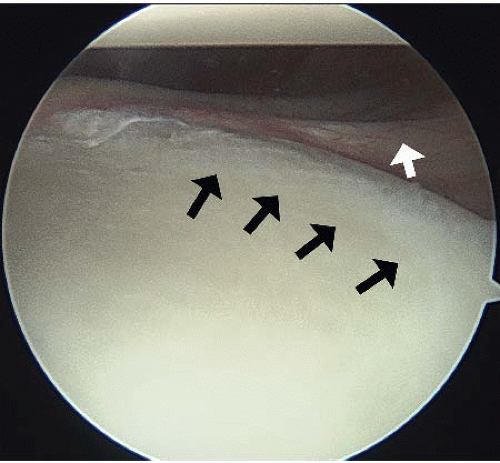 FIGURE 17.1. The glenoid labrum is shown including the chondrolabral junction on the glenoid (black arrow). The IGHL (white arrow) is also shown. |
While the Bankart lesion has been referred to as the essential lesion of anterior instability, Speer et al. (5) demonstrated that an isolated Bankart lesion was insufficient to cause significant increased translation and instability and surmised that in addition to the Bankart lesion, plastic deformation of the IGHL must also occur for instability to exist. A previous study by Bigliani et al. (6) showed that the IGHL undergoes strain injury during an anterior shoulder instability event and may become permanently stretched even without detachment from the anterior glenoid labrum. Open revisions of failed arthroscopic instability repairs have shown marked capsular laxity even in the presence of healed Bankart lesions (7) due to permanent deformation of the glenohumeral ligaments and anterior capsule. This emphasizes the need for appropriate retensioning of capsular laxity in addition to repair of the glenoid labral lesion in order to achieve successful results.
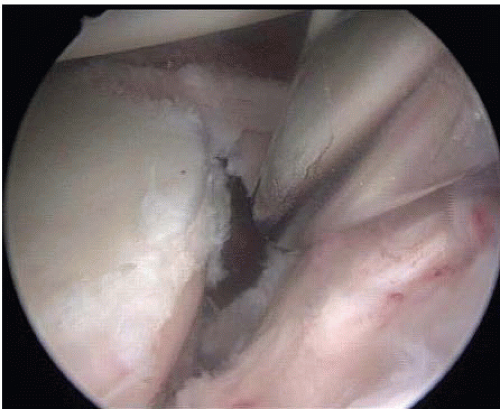 FIGURE 17.2. Typical appearance of a Bankart lesion. This represents a soft tissue type of Bankart tear—with an avulsed anterior labrum from the glenoid. |
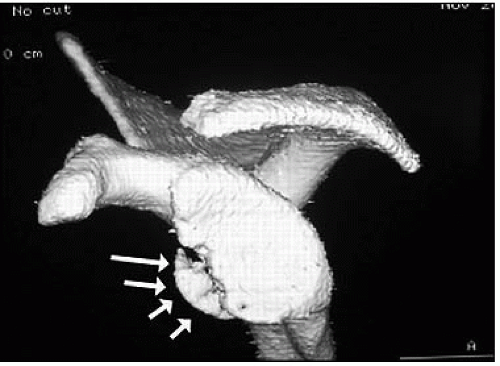 FIGURE 17.3. A bony Bankart injury is demonstrated on a sagittal oblique CT scan, demonstrating an avulsed anterior portion of the glenoid. |
Bony lesions associated with anterior instability are typically located in the anteroinferior quadrant and consist of a displaced fracture fragment or an attritional bone loss due to bone erosion from repetitive episodes of subluxation or dislocation (Fig. 17.3). This can lead to the glenoid taking on the shape of an inverted pear, which has been shown to correlate with a bone loss of 25% to 30% (Fig. 17.4) (8). Another common lesion encountered in instability is at the rotator interval, which is the triangular space bordered superiorly by the supraspinatus tendon and inferiorly by the subscapularis tendon. Widening of this interval can lead to a voluminous capsule and a resultant decrease in glenohumeral stability. It has been shown that in select patients adjunct treatment with closure of the rotator interval can improve anterior instability (9).
Other articular lesions associated with anterior instability include a superior labral anterior posterior (SLAP) lesion, which is a detachment of the glenoid labrum at the insertion of the long head of the biceps tendon, the medial displacement of the labrum and glenoid sleeve of the anterior glenoid (anterior labral periosteal sleeve avulsion or ALPSA) and the humeral avulsion of the glenohumeral ligament (HAGL lesion). The presence of these lesions can lead to significant instability and future dislocations if not properly addressed. Therefore, care must be taken to identify their presence (Fig. 17.5).
CLINICAL EVALUATION
History
When evaluating the patient with recurrent anterior instability, the history should include a complete description of symptoms and any previous shoulder dislocations, injuries, or previous surgery. A full history of glenohumeral instability should also be obtained and includes the nature of previous dislocations (voluntary vs traumatic), the nature of the reduction (self-reductions vs reduction by a healthcare professional), the number and duration of dislocations or instability events, and any previous therapy or treatments to the affected shoulder.
The type of activity in which the patient is engaged and the specific activities that cause instability should be noted. Patients with anterior shoulder instability most often present with feelings of subluxation or impending dislocation with apprehension during certain shoulder positions (namely, abduction and external rotation and with overhead activities). In addition, they may also complain of pain and weakness in the affected shoulder. Subjective feelings of instability are often experienced during repetitive overhead activities, such as throwing and swimming. Patients may also complain of sudden, transient, sharp pain, numbness, or weakness that usually resolves spontaneously as the only symptom of instability.
Physical Examination
Physical examination should include a comprehensive evaluation of the shoulder to include visualization, palpation, ranges of motion, strength, neurologic exam, and specific stability testing. An evaluation of posture and gross examination of shoulder symmetry should be performed in comparison with the contralateral shoulder. Active and passive range of motion should be measured bilaterally in external rotation, internal rotation, flexion, and abduction, with attention also directed to scapular function during range of motion. Instability encountered during mid-range of motion may indicate significant bony defects. The affected shoulder should be palpated to assess for inflammation, deformity, muscle wasting, and tenderness with attention to AC joint and biceps tendon involvement. Strength testing should be performed for each motion and compared with the contralateral shoulder. Differences in active versus passive range of motion may be evidence of an associated rotator cuff tear or nerve injury. A complete neurologic examination of the extremity should be performed to rule out injury to the brachial plexus, axillary nerve, or any cervical or peripheral nerve involvement.
Apprehension testing recreates the position of anterior instability with an abduction external rotation force placed on the humerus. The apprehension test is positive when the patient senses an impending dislocation. With the relocation test, the feeling of dislocation is alleviated with a posteriorly directed force to the humeral head. The presence of pain is not indicative of a positive test.
Translational load and shift tests should be performed to assess the degree and direction of instability and to rule out multiple direction instability (MDI). These tests may be performed in the lateral decubitus position and compared with the contralateral side in the anterior and posterior planes, documenting the presence of pain or instability throughout the exam. A directional force is applied to the concentrically loaded humeral head and the amount of translation of the humerus on the glenoid is then graded zero (minimal translation), 1+ (translation of the humeral head up to the face of the glenoid labrum without subluxation), 2+ (translation with subluxation over the glenoid rim and spontaneous reduction), and 3+ (translation over the glenoid rim completely without spontaneous reduction) (10, 11).
An inferior translation (sulcus test) should also be performed to look for MDI by placing an inferiorly directed force on the adducted arm in both the neutral and the externally rotated positions measuring the amount of separation in centimeters between the humeral head and the acromion to evaluate for inferior laxity. This can be graded according to the measured distance of the sulcus ranging from 0 to 3+ (10, 11). If a large sulcus persists in external rotation, it is likely that a rotator interval lesion is contributing to a component of the patient’s overall instability pattern (Fig. 17.6).
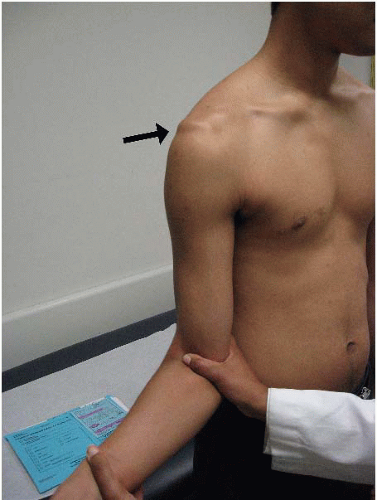 FIGURE 17.6. A sulcus finding that persists in external rotation (black arrow) is indicative of an incompetent rotator interval. |
Other joints should be evaluated for laxity including the contralateral shoulder and tests to evaluate for global joint hyperlaxity such as the ability of the patient to bring the thumb to the wrist. Specific tests such as the crossbody adduction, Neer’s and Hawkin’s impingement tests, O’Brien’s active compression test, and Speed’s test may help in identifying other possible causes of shoulder pain.
Radiologic Evaluation
Anterior glenoid bony defects may be present in most anterior instability cases. Plain film radiographs of the shoulder in the anterior-posterior (AP), supraspinatus outlet, and axillary views can help assess the integrity of the glenoid rim and humeral head and can rule out other osseous lesions. The West Point, Garth, and Stryker notch views are also helpful in determining the extent of bone loss of the glenoid rim and the presence of Hill-Sachs lesions.
Imaging with a computed tomography (CT) scan can help to better visualize bony defects or abnormalities and can further aid in the diagnosis and operative planning. If a significant bony glenoid lesion is suspected, a CT scan with 3D reconstruction and digital subtraction of the humeral head can be used to evaluate the extent and location of bone loss. A 3D CT can be used to accurately measure anterior bone loss and aid in preoperative planning, ensuring that an arthroscopic repair is a viable option for the patient (12). The extent of bone loss on imaging studies is an important consideration before choosing arthroscopic management of shoulder instability as those with significant bony defects of the glenoid and/or humeral head may have higher rates of recurrence without open augmentation (4).
Magnetic resonance imaging (MRI) can also be used to visualize bony lesions and soft tissue injuries and to evaluate labral and capsuloligamentous integrity. MRI should be considered in patients over age 40 with anterior shoulder instability due to the high incidence of associated rotator cuff tearing in this population. MR arthrogram provides additional sensitivity in the detection of capsulolabral pathology, and it has been shown that MR arthrogram can successfully measure capsular volume in relation to the degree of instability (Figs. 17.7 and 17.8) (13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree