Anterior Shoulder Instability: Suture Anchor
Benjamin Shaffer
Jonas R. Rudzki
Patrick Birmingham
Anterior shoulder instability is a common problem, particularly in the young athletic population, with a prevalence of anterior shoulder dislocation between 2% and 8% (1). Although most of these instability events are traumatic dislocations, some patients experience an initial subluxation. Recurrent instability (dislocations and subluxations) is often age-dependent, with the risk among patients younger than age 20 averaging between 50% and 65%, although in some series it can be as high as 90% with nonoperative treatment. (1) This recurrence rate drops below 50% in patients greater than 25 years old (2).
The high recurrence rate, combined with the significant athletic impairment in patients with anterior instability, has led us to consider operative intervention as the definitive treatment for most young athletes. For nearly a century, stabilization has been achieved through an open surgical technique, the Bankart repair, with reported success rates up to 97% (1, 3, 4). However, with the advent of less invasive technology, arthroscopic techniques for anterior instability have flourished and over time evolved to become the de facto standard for many physicians treating this condition. In comparison to traditional open approaches, arthroscopic repair offers the potential advantages of decreased postoperative pain, stiffness, recurrent instability, and a faster functional recovery. Although there is current dispute whether arthroscopic repair affords better stability results than open, the practical benefits of arthroscopic repair have been well established.
Arthroscopic stabilization has seen a dramatic evolution in technology over the last few decades, transitioning from a simple reapproximation of the detached labrum with a metal staple to a more stable fixation technique using suture anchors. Suture anchors offer numerous advantages over other current techniques including flexibility in number and type of suture used, and the ability to individually titrate capsular patholaxity in each case.
Today’s operative success rates of 90% to 95% are attributable in part to advances in technology but can also be traced to refinements in our indications, recognition and treatment of contributory pathology (especially concomitant capsular patholaxity), and advances in surgical technique and experience. The purpose of this chapter is to provide an overview of our understanding and approach to treating the patient with anterior instability, emphasizing the clinical evaluation and indications, and to provide a detailed map for the successful arthroscopic repair technique using suture anchors.
NORMAL SHOULDER FUNCTIONAL ANATOMY
The shoulder is a highly unconstrained ball and socket joint, which relies upon both static and dynamic mechanisms for stability. Its intrinsic lack of constraint allows for its wide range of motion, translation, and function, although these render it vulnerable to instability. Architecturally, the glenoid is a shallow socket whose concavity and depth are increased 50% to 80% by the surrounding labrum. The fibrocartilaginous labrum helps to increase the diameter of the socket by up to 57% in the transverse direction and 75% vertically (5). In conjunction with adjacent capsular ligaments, the labrum significantly enhances glenohumeral stability.
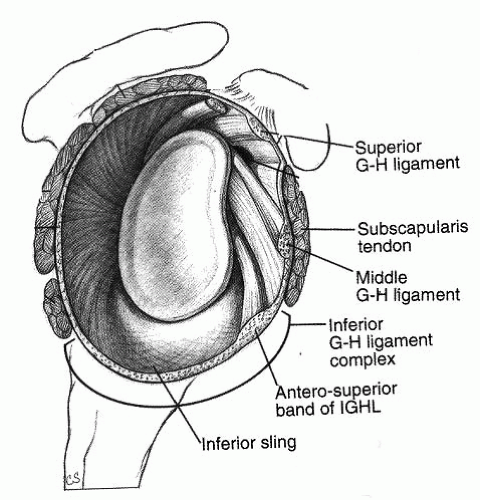
Viewed arthroscopically, the shoulder capsule comprises three discrete glenohumeral ligaments, which serve as static stabilizers (Fig. 16.1). Selective cutting and biomechanical studies have shown that their individual contributions vary depending upon arm position, rotation, and magnitude of the applied force. The superior glenohumeral ligament (SGHL) serves to resist inferior translation with the arm in the adducted position and is thought to play a significant role in patients with inferior laxity and multidirectional instability (MDI). The middle glenohumeral ligament (MGHL) varies in size and shape but resists external rotation and translation with the arm abducted 45°. The most important of the glenohumeral ligaments is the inferior glenohumeral ligament (IGHL) complex, which is the primary stabilizer to anterior humeral translation at 90° of abduction (6). This complex consists of anterior and posterior bands with an intervening sling cradling the
humeral head inferiorly. The bands have been described to function as a hammock, with the anterior band reciprocally tightening in abduction and external rotation whereas the posterior band comes under tension with forward elevation and internal rotation. Together with the glenoid labrum, these ligaments form a capsulolabral complex, which serves as the primary static stabilizer of the glenohumeral joint (6).
humeral head inferiorly. The bands have been described to function as a hammock, with the anterior band reciprocally tightening in abduction and external rotation whereas the posterior band comes under tension with forward elevation and internal rotation. Together with the glenoid labrum, these ligaments form a capsulolabral complex, which serves as the primary static stabilizer of the glenohumeral joint (6).
Dynamic stability is provided by the rotator cuff muscles, which through concavity-compression center the humeral head on the glenoid (6). The interaction between these static and dynamic stabilizers helps to maintain glenohumeral stability through a broad range of motion.
Anterior shoulder instability is typically thought to occur subsequent to injury to the static stabilizers, specifically to the anteroinferior labrum and capsule (6,7). Detachment of the labrum from the anterior glenoid in the setting of recurrent anterior shoulder instability was originally described in 1938 (Fig. 16.2) These lesions have been reported in 65% to 95% of shoulders, undergoing surgical treatment for anterior instability (3); however, there is likely no single “essential lesion” in anterior shoulder instability. Basic science data have shown that isolated labral detachments are in fact uncommon, and most instability has some element of associated capsular pathology. This underscores the importance of addressing concomitant capsular patholaxity along with labral repair.
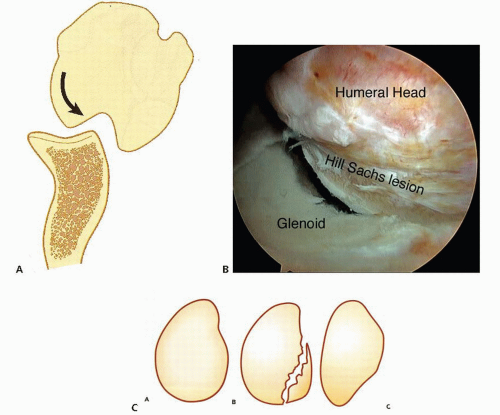
In addition to soft tissue injury, bony pathology is not uncommon in patients with shoulder instability. Osteochondral injury to the posterior humeral head, known as a Hill-Sachs lesion, is common resulting from humeral head impaction against the anterior-inferior (AI) glenoid at the time of subluxation or dislocation (Fig. 16.3). Several studies have reported a considerable increase in recurrence rate following arthroscopic stabilization in patients with significant “engaging” Hill-Sachs lesions.
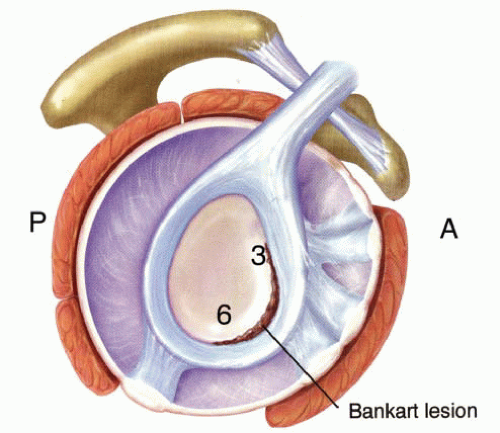 FIGURE 16.2. The Bankart lesion describes a detachment of the labrum and capsuloligamentous sleeve, usually from the approximately 3 o’clock to 6 o’clock position; A, anterior; P, posterior. |
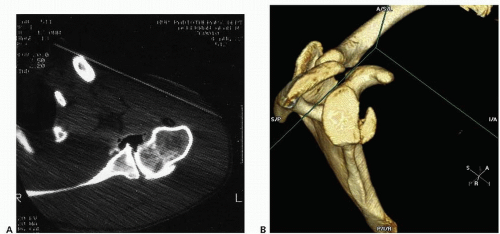
On the glenoid side, osseous Bankart lesions with fracture of the adjacent anterior-inferior glenoid rim may occur in up to 73% of cases (3) (Fig. 16.4). The avulsed fracture fragment typically remains attached to the capsulolabral tissue. This bony injury is significant because it may result in compromise of the normal articular arc and decrease the threshold of force necessary for humeral head translation, leading to recurrent subluxation and/or dislocation. Soft tissue procedures that repair the labrum
and/or address capsular patholaxity are not likely to be effective in the face of articular arc deficiency.
and/or address capsular patholaxity are not likely to be effective in the face of articular arc deficiency.
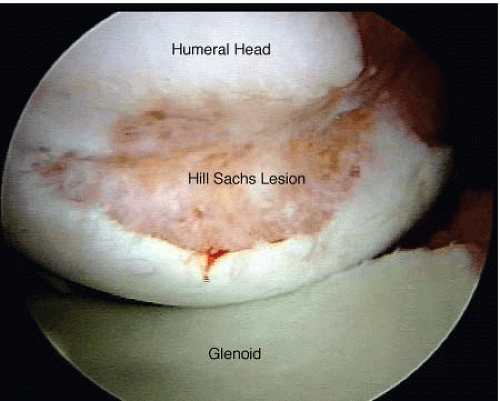 FIGURE 16.3. The Hill-Sachs lesion, a hatched-shaped defect in the posterolateral head, is seen in this arthroscopic photo of a right shoulder in the lateral decubitus position. |
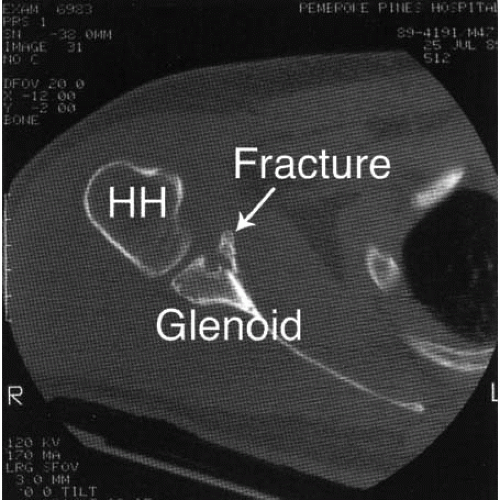 FIGURE 16.4. Fracture of the anterior-inferior glenoid rim is assessed via CT scan, in this axial section demonstrating greater than 25% compromise; HH, humeral head. |
Less commonly, instability can occur subsequent to other structural injuries. Tears of the rotator cuff can occur with shoulder dislocation and can predispose to recurrence either in isolation or accompanying a labral detachment. Subscapularis tendon disruptions are uncommon but require consideration in traumatic instability among contact/collision athletes. Capsular failure on the humeral side, known as a HAGL (humeral avulsion of the glenohumeral ligament) lesion, can cause instability without labral injury.
CLINICAL EVALUATION
The clinical evaluation of the patient with anterior shoulder instability begins with a thorough history, paying particular attention to the patient’s age at the time of initial injury, mechanism of injury, hand dominance, and desired occupational and/or recreational activity level. Age at the time of acute shoulder dislocations has been shown to influence the subsequent risk of recurrent instability with patients under 20 years of age at greatest risk. Eliciting the mechanism helps with understanding the likely injury pattern and possible presence of concomitant pathology.
One should determine the severity of the instability, episode and its precipitating cause. Did the shoulder completely dislocate or just sublux? How many instability episodes have occurred, have the instability episodes changed over time, and have they required manipulative reductions or recurred with less provocation? In what position has the arm been positioned at the time of these instability episodes? Was the dislocation documented with X-rays? All these considerations affect understanding the significance of the problem and influence both the evaluation and the treatment decision-making.
Physical exam must include standard tests for active and passive range of motion, deltoid and cuff strength, and neurovascular status. In the acutely dislocated shoulder, physical examination may be of limited value because of pain and apprehension. Patients with recurrent instability offer an easier exam.
Tests specific for instability include glenohumeral translation and functional instability testing, which help determine the direction and extent of the instability pattern and may suggest concomitant pathology. It is important to distinguish laxity, an objective measurement of joint translation, from instability, which is symptomatic laxity.
In laxity, assessment loads are applied to the glenohumeral joint, noting the degree of humeral head translation. Because of variable laxity in the population, comparison with the opposite shoulder is important. Occasionally, translation testing will reveal mechanical catching or grinding consistent with labral pathology, or elicit symptoms that occur with the patients’ instability episodes.
Several grading classifications for translation testing have been described. In one such scale, Grade 0 represents no translation. Grade 1 is mild translation, in which the humeral head moves slightly up the face of the glenoid 0 to 1 cm. Grade 2 refers to moderate translation, in which the humeral head rides up the glenoid face to but not over the rim (1 to 2 cm translation). In Grade 3, there is severe (greater than 2 cm) translation, in which the humeral head rides up and over the glenoid rim (though it usually reduces when stress is removed).
Subjective functional instability tests attempt to elicit symptoms by placing the arm in provocative positions and under various loads. The time-honored apprehension test may be of greatest value, placing the arm in the abducted, externally rotated (i.e., throwing) position. Some patients require some translation force in this position to elicit the sense of instability. This can be performed either in the supine position with gentle anterior load applied to the posterior shoulder or in an upright seated position. Prior to applying the translation force, the humeral head is loaded in the glenoid and then shifted, thus the name “load-and-shift” tests. Our preference is to perform the test supine, which provides for a more relaxed exam.
The “relocation” test may be of value in detecting subtle anterior instability, particularly in patients without a history of overt dislocations. In this test, the arm is placed in the abduction, external rotation position, and a gentle anterior load applied to the humeral head. This test is considered positive when the patient feels subjective apprehension or discomfort under anterior load, alleviated by posterior translation to the humeral head with presumed reduction of the joint.
Tests that facilitate detection of other pathology include an apprehension and load-and-shift test for posterior instability, and the active-compression test (among
others) for detection of superior labral (SLAP) pathology. Inferior instability can occur in conjunction with anterior instability, and has traditionally been assessed using the sulcus sign in adduction, repeated again in external rotation. The sulcus sign is considered more significant if it persists with external rotation. Because the sulcus sign may be normal in some patients with generalized laxity, it is important to assess overall soft tissue laxity such as metacarpophalangeal (MCP) hyperextension, elbow recurvatum, and the “thumb-to-forearm” tests.
others) for detection of superior labral (SLAP) pathology. Inferior instability can occur in conjunction with anterior instability, and has traditionally been assessed using the sulcus sign in adduction, repeated again in external rotation. The sulcus sign is considered more significant if it persists with external rotation. Because the sulcus sign may be normal in some patients with generalized laxity, it is important to assess overall soft tissue laxity such as metacarpophalangeal (MCP) hyperextension, elbow recurvatum, and the “thumb-to-forearm” tests.
Evaluation of the rotator cuff is important particularly in contact, collision sport athletes with a traumatic dislocation in which compromise of the cuff may coexist with labral pathology. Conventional tests for supraspinatus strength (empty-can position against resistance) and infraspinatus strength (external rotation of the adducted arm at the side against resistance) are standard. Evaluation for occult subscapularis injury includes the abdominal compression and lift off tests. In the patient with recurrent instability, observation of scapulothoracic mechanics is an important component of a comprehensive exam as scapulothoracic dysfunction may contribute to instability in some patients. Finally, the neurovascular status of the upper extremity (e.g., axillary nerve) and a cervical spine examination complete a thorough assessment of the shoulder.
Diagnostic imaging of anterior shoulder instability includes standard anterior-posterior (AP) and axillary views. Abnormalities may warrant more specialized radiographs, such as a Stryker view for evaluation of a Hill-Sachs lesion and a West-Point axillary view to better assess an osseous Bankart lesion (Fig. 16.5). In cases where there is a significant Hill-Sachs or bony Bankart lesion, a CT scan with three-dimensional reconstruction can better quantify the extent of articular-arc compromise and the potential need for alternative surgical strategies (Fig. 16.6).
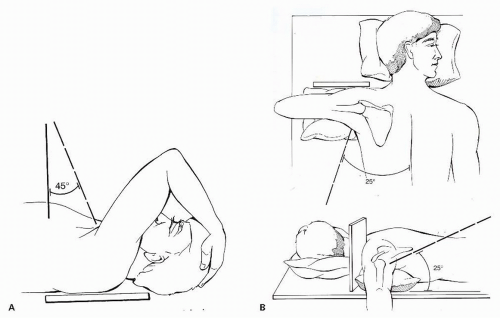 FIGURE 16.5. A: Stryker Notch view to assess Hill-Sachs lesion. B: West-Point view to assess the anterior glenoid for a bony Bankart lesion or glenoid insufficiency. |
Magnetic resonance imaging is not routinely necessary in the evaluation of shoulder instability, though it may be appropriate in specific circumstances. These include patients with first time instability over age 40 to evaluate the cuff integrity and following significant trauma to assess possible subscapularis tendon rupture. An MRI can be helpful in evaluating the location and extent of the capsulolabral injury. Enhanced-imaging techniques with chondral sequencing have enabled some magnets to provide vivid detail of the capsulolabral complex and osteochondral anatomy without contrast. MR arthrography is not usually necessary, though may be of value in some cases with unclear instability patterns.
TREATMENT DECISION-MAKING
Following reduction (spontaneously or with manipulation) of an anteriorly dislocated shoulder, most patients with acute shoulder instability are managed
nonoperatively. Nonoperative treatment should focus on a rehabilitation program that avoids the provocative position and incorporates a strengthening program designed to enhance the dynamic shoulder stabilizers. Patients with recurrent instability following nonoperative treatment may be surgical candidates. Studies have shown that in the young athlete, nonoperative treatment is largely ineffective with recurrence rates approaching 90% in those under 20 years of age (1). Because of the high risk of recurrence in some groups, surgical treatment of the first-time dislocator in the younger athlete has gained traction. Other factors that may influence primary repair of the first-time dislocator include arm dominance, type of sport or activity, level of participation and performance, goals, timing with respect to their athletic season, and factors related to the instability episode itself such as the presence of a repairable bony Bankart lesion.
nonoperatively. Nonoperative treatment should focus on a rehabilitation program that avoids the provocative position and incorporates a strengthening program designed to enhance the dynamic shoulder stabilizers. Patients with recurrent instability following nonoperative treatment may be surgical candidates. Studies have shown that in the young athlete, nonoperative treatment is largely ineffective with recurrence rates approaching 90% in those under 20 years of age (1). Because of the high risk of recurrence in some groups, surgical treatment of the first-time dislocator in the younger athlete has gained traction. Other factors that may influence primary repair of the first-time dislocator include arm dominance, type of sport or activity, level of participation and performance, goals, timing with respect to their athletic season, and factors related to the instability episode itself such as the presence of a repairable bony Bankart lesion.
The threshold for operative intervention in patients with recurrent instability and functional impairment is considerably lower. Painful instability episodes, repeated stints in physical therapy, athletic disability, and impairment in activities of daily living all contribute to the surgical decision-making.
INDICATIONS
The current ideal indication for arthroscopic stabilization is a patient with recurrent posttraumatic anterior instability who has a Bankart lesion, good quality labral tissue, and no evidence of significant bony pathology. From an athletic standpoint, arthroscopic stabilization has been particularly emphasized over open procedures in the throwing population in which motion preservation is critical.
CONTRAINDICATIONS
Current contraindications to arthroscopic stabilization include patients with “significant” bony pathology and poor quality capsulolabral tissue. “Significant” bony defects include glenoid insufficiency in which greater than 25% of the anterior-inferior glenoid surface is deficient and/or an “engaging” Hill-Sachs on the humeral side, typically constituting greater than 30% of the articular surface (Fig. 16.7). Yet even these guidelines are not absolute and some authors have reported successful outcomes with arthroscopic management of anterior shoulder instability even in the face of a deficient glenoid (termed an “inverted pear” (8)). In addition, several procedures have been introduced that arthroscopically address articular arc deficiency. These include soft tissue advancement of the infraspinatus tendon into the humeral head (Hill-Sachs) defect (“Remplissage” technique (9)) and bone grafting of the humeral head defect (10). However, most authors would agree that significant bony pathology warrants open reconstruction by an anatomic open Bankart repair that addresses the bony defect directly, or a nonanatomic open repair such as the Bristow-Latarjet procedure.
Compromised soft tissue capsulolabral tissue is relatively uncommon but may be a limiting factor in patients who have undergone thermal capsulorrhaphy or revision surgery. In these cases, open repair using soft tissue augmentation may be necessary.
Until recently, other contraindications included patients with HAGL lesions (more easily fixed open),
those undergoing revision surgeries, and those playing contact or collision sports. As arthroscopic techniques have evolved and experience is accrued, each of these have become only “relative” contraindications with operative decision making influenced by the presence of concomitant pathology, technical experience, and surgeon preference.
those undergoing revision surgeries, and those playing contact or collision sports. As arthroscopic techniques have evolved and experience is accrued, each of these have become only “relative” contraindications with operative decision making influenced by the presence of concomitant pathology, technical experience, and surgeon preference.
The optimal approach for treatment of contact and collision-sports athletes remains a controversial topic. Historically, open anterior stabilization has been advocated as the “gold standard” or treatment of choice for this patient population. Arthroscopic stabilization in a contact and collision sport athlete has been contraindicated because of reports suggesting a higher risk of failure. Some authors have advocated open stabilization in this group of athletes citing low recurrence rates. But outcome data have recently called this conclusion into question. Stratifying the data based on factors other than simply the sport have shown that recurrence is more likely due to bone deficiency, which is more common in contact athletes, rather than the surgical technique (11). Mazzocca reported an 11% rate of recurrent dislocation in their series of collision and contact athletes treated with arthroscopic suture anchor shoulder stabilization.
Many studies have shown satisfactory outcomes with revision surgery following failed open or arthroscopic surgery. The key is the quality of the soft tissue and bone integrity, expectations of the patient, and skill of the surgeon. Patients with voluntary instability in which there may be secondary gain or psychological issues are not appropriate candidates for arthroscopic stabilization and are probably inappropriate candidates for open surgical repair as well. Likewise, patients who are unable to comply with the postoperative immobilization or rehabilitation risk a compromised outcome and may be better treated without surgery. Favorable surgical outcomes can follow conservative management, rehabilitation, and bracing (position dependent) until the completion of the season (11).
SURGICAL TECHNIQUE
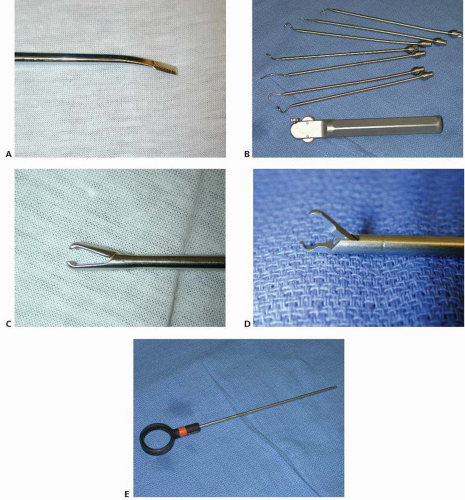
Instrumentation, Implants, and Cannula Selection
In addition to the standard setup for shoulder arthroscopy, stabilization requires specific instrumentation (Fig. 16.8). This includes a 70° arthroscope and cannulas with internal diameters sufficient to accommodate anchor and suture passing instruments. An angled arthroscopic elevator (Liberator rasp, ConMed Linvatec, Largo, FL) is required to mobilize the capsulolabral complex. Shaver blades that both debride and abrade are necessary for glenoid preparation. Several different types of suture passing instruments are helpful to minimize struggling during this step. A soft tissue grasper, suture retriever, knot pusher, and knot cutter complete the instrumentation.
Several considerations influence the physician’s preference and choice of a suture anchor, including the composition, size, number and type of sutures per anchor, and ease of use. Pullout strength is probably sufficient for most anchors currently on the market, so this biomechanical factor is of little significance when choosing an implant. Some surgeons still favor metallic implants due to their comfort level, low cost, ability to visualize on X-ray, and lack of osteolysis. However, limitations of metal implants include possible suture abrasion through the eyelet (depending upon eyelet design), difficulty with anchor extraction if improperly placed or proud, and the potential for devastating chondral wear in cases of suboptimal positioning or migration. Metal anchors are also visible on X-rays which depending upon one’s perspective may or may not be advantageous; and, in cases of recurrent instability or postoperative complications may interfere with MR interpretation due to artifact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree