Anterior Odontoid Fixation
Ronald I. Apfelbaum
Rick C. Sasso
INDICATIONS
Direct anterior odontoid screw fixation is indicated in patients with acute type II and high type III (with a shallow base) odontoid fractures (Fig. 6-1). The rationale for direct anterior fixation is the achievement of immediate fixation in anatomical alignment, stabilizing the atlantoaxial complex while providing the best environment for fracture healing. The construct preserves C1-C2 rotation while providing rigid internal fixation and avoids restrictive bracing and the complications associated with bone grafting techniques. It has a higher success rate than and reduces the morbidity associated with prolonged halo immobilization, which had been used preferentially in the past. Direct anterior osteosynthesis of the odontoid fracture with anterior odontoid screw fixation is often the preferred alternative to atlantoaxial arthrodesis for management of odontoid fractures. This technique has been shown to achieve a high healing rate, similar to that of posterior atlantoaxial arthrodesis (88% to 100%), with a similarly low complication rate (1,4,9,27,30,31), and has the advantage over posterior methods of achieving this without intentionally sacrificing atlantoaxial motion (2,27,30).
Polytrauma patients, in whom immediate mobilization has proved beneficial, are also good candidates for anterior odontoid screw fixation as they often are not candidates for halo-vest stabilization. Direct osteosynthesis also can be used in patients who refuse halo treatment and in those in whom fracture reduction can be obtained but not maintained in this apparatus.
CONTRAINDICATIONS
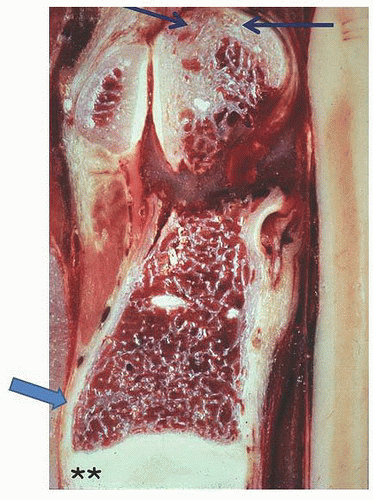
Caution should be used in osteopenic patients; many patients with odontoid fractures are elderly and will have decreased bone mineralization. There is less reason to be concerned about the bone density of the cancellous interior of the odontoid and the C2 body because healing occurs primarily across the cortical bone at the junction of these two. Therefore, if the cortical shell of C2 and the odontoid are reasonably well ossified and there is good apical bone at the tip of the odontoid, screw fixation maybe considered. The lag screw needs to have good purchase in the strongest region of the odontoid—the dense apical cortex—and have a good buttress at the strong anterior inferior aspect of the C2 body to be effective (Fig. 6-2).
A fixed kyphotic angulation of the neck or a barrel chest with a short neck may preclude obtaining the low trajectory needed to place a screw from the inferior edge of C2 to the odontoid apex. This can be checked before surgery using lateral fluoroscopy when the patient is optimally positioned. If the trajectory is not adequate, we will not proceed with direct odontoid screw fixation but rather reposition the patient and perform a C1-C2 instrumented fusion. Compromising the trajectory and accepting an entry site for the screw on the anterior face of C2 rather than the inferior one is not recommended.
Anatomic reduction of the odontoid fracture is imperative before the fixation screw is placed across the fracture. Inability to achieve reduction prior to commencing surgery was therefore previously considered to be an absolute contraindication to the procedure; however, intraoperative reduction and perfection of the alignment of the odontoid to the body of C2 can be obtained using the techniques and instrument system described in this chapter, so this is no longer a contraindication. An absolute contraindication to anterior screw fixation is (the relatively rare) concomitant transverse atlantal ligament (TAL) disruption since, in such a case, fixation of the odontoid alone will not stabilize the C1-C2 complex.
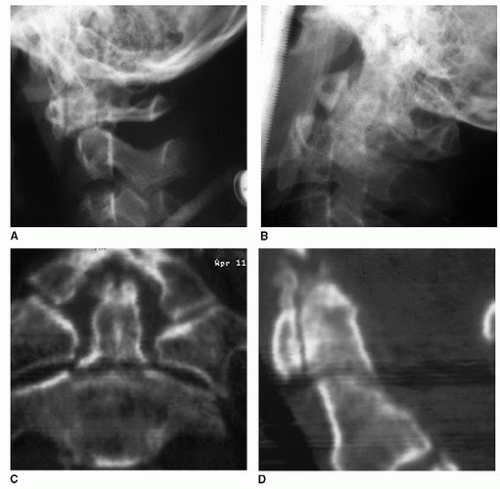 FIGURE 6-1 Type II odontoid fractures: with odontoid anterolisthesed (A) and retrolisthesed (B). High Type III odontoid fracture (C, D). (Copyright Dr. Ronald I. Apfelbaum). |
Chronic fracture nonunions over 6 months old and oblique fractures in an anteroinferior-to-posterosuperior plane that could cause the odontoid fragment to shear anteriorly at the fracture site during lag compression are relative contraindications. The success rate of direct screw fixation for fractures over 6 months of age (25%) has been substantially lower than in those treated earlier. Patients with fractures treated within the first 6 months, such as those treated after failure of a trial of halo immobilization, did as well as those with fresh fractures (4). This is similar to the experience in treating patients with nonunions of anterior cervical interbody fusions with posterior rigid fixation. Once the motion is eliminated, a high percentage of patients with anterior nonunions go on to achieve solid fusion. In regard to oblique fractures, if the overall bone quality is adequate, fixing them in a slight retrolisthesed position in anticipation of the translation of C1 anteriorly on C2 can result in the final alignment being anatomic. In such a case, we would also use a hard collar for 6 weeks to restrict neck flexion. Others also have reported good success with shallower anterior oblique fractures (11).
PREOPERATIVE PREPARATION
Examination and Evaluation/Pathology
Odontoid fractures are relatively common upper cervical spine injuries, constituting nearly 60% of all fractures of the axis and 10% to 18% of all cervical spine fractures (6,24,30). Proportionally greater space is available for the spinal cord in the upper cervical spine than in the lower cervical spine. Therefore, the incidence of neurologic involvement in upper cervical spine injury is relatively low (18% to 26%) (12,38). Furthermore, when significant cord damage does occur in the upper cervical spine, patients frequently do not survive because of respiratory arrest. Modern immobilization and transportation techniques have reduced the incidence of secondary injuries at this level and resulted in more survivors with injuries that previously might have been fatal.
Although odontoid fractures occur in all age groups, the bimodal distribution observed in the past is changing. In younger patients, who represent the first peak incidence, these fractures are usually secondary to high-energy trauma; motor vehicle accidents are responsible for the majority of the odontoid injuries (6,13). Often, the injured patient was a nonrestrained passenger in the front seat whose neck was violently hyperextended when his or her head or face struck the windshield. Concomitant spinal injuries are present in up to 34% of patients; 85% of these associated injuries occur in the cervical spine, most commonly the atlas (12,23,38). These injuries have become much less frequent with the increased use of seat belts and the proliferation of passive restraints such as airbags. The second peak in the incidence of odontoid fractures occurs among the elderly (30). In fact, odontoid fractures are the most common cervical spine fracture in patients older than 70 years (34,35,37). These fractures, unlike those in the younger patients, tend to result from low-energy injuries, such as falls from a standing height. The mechanism of injury is often hyperextension that results in posterior displacement of the odontoid. Associated spinal trauma is much less common in elderly patients (7,12). With increased longevity, these injuries are being seen more frequently and make up the clear majority of odontoid fractures.
Preoperative Radiographic Evaluation
Which imaging studies should be obtained for a comprehensive, diagnostic approach in evaluating suspected upper cervical spine injuries remains a topic of controversy, particularly in the presence of polytrauma or for obtunded patients. The standard, initial cervical spine radiographic series in trauma patients includes a cross-table lateral view, an anteroposterior (AP) view, and an open-mouth view. The value of the AP view has been questioned because it provides little additional information (18). Although this three-view screening series can detect 65% to 95% of axis injuries (30), the C2 vertebra is often obscured by overlying bony maxillary, mandibular, and dental structures; therefore, C2 fractures may be missed. Thin-section computed tomography (CT) is the best study for evaluating C2 bony fractures (8). Sagittal reconstruction of CT images is important because axial images may not show a transverse odontoid fracture. These views can also provide valuable information about the cortical bone density, the status of the subaxial spine, and the presence of anterior osteophytes that may factor into the decision regarding choice of approach.
Although CT is excellent in demonstrating bony injuries, soft tissue and significant ligamentous injuries may not be apparent. Therefore, dynamic flexion/extension lateral fluoroscopic evaluation has been advocated for polytrauma patients to identify occult ligamentous instabilities and confirm that the cervical spine is uninjured (25). Magnetic resonance imaging (MRI) also is helpful in assessing the spinal cord in patients with and without neurologic deficits and gives important information about the subaxial spine. It also is becoming increasingly important in evaluating the status of ligamentous structures such as the TAL.
The assessment of TAL integrity in patients with odontoid fractures is an important consideration in selecting appropriate treatment options (15). Anterior odontoid screw fixation will not provide C1-C2 stability if the TAL is not competent. TAL disruption has been reported to occur in 10% of patients with odontoid fractures (22); however, in our experience, we have rarely noted instability when evaluating TAL integrity by flexing the patient’s neck under fluoroscopy after odontoid fixation. This brings into question the accuracy of the MRI criteria. Nevertheless, the combination of MRI, CT, and plain radiographs is important for evaluating unstable C2 fractures and planning a rational treatment course. When a C2 fracture is identified, it is necessary to also evaluate the subaxial spine carefully because 16% of patients have a noncontiguous fracture (39).
TECHNIQUE
Positioning
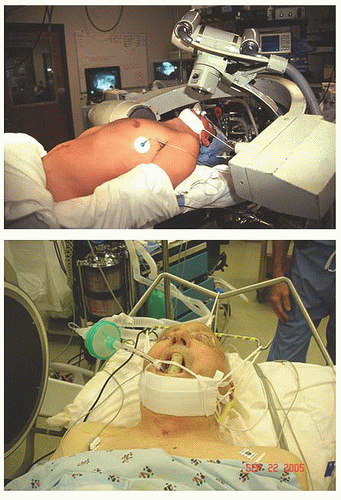
Before beginning the operation, the surgeon must ensure that reduction of the odontoid to a more anatomic position is possible. Some prefer to do this by simple traction or manipulation while the patient is awake, with lateral fluoroscopic imaging. Typically, we will place the patient on the operating table with a folded blanket or other suitable padding under the shoulders and a similar padding under the head to keep the neck in a neutral position (Fig. 6-3). If the patient’s odontoid in this position is anterolisthesed, we extend the patient’s neck while observing the alignment under fluoroscopy and gradually remove the head pads. This may reduce the anterolisthesis of C1 and the odontoid process relative to C2 while also optimizing the patient’s head position for both intubation and screw placement. If the patient’s odontoid is retrolisthesed, the degree of mobility can be assessed under fluoroscopy when the neck is slightly flexed. These preliminary maneuvers help ascertain that reduction will be possible intraoperatively. Intubation should be done without moving the patient’s neck in the direction that increases the subluxation. This may require fiberoptic intubation techniques.
To achieve a proper screw trajectory and clear the anterior chest with the instrumentation, it is usually necessary to extend the patient’s neck; however, unless this position results in optimal reduction and alignment, this is best done once the screw guidance tubes are in place as is described below. In essence, we will accept the best aligned position to begin the approach but prepare the setup to allow us to modify the patient’s head position once the C1-C2 relationship is perfected intraoperatively. Therefore, “perfect” preoperative reduction is not required to proceed.
Once the patient is intubated, a radiolucent mouth gag is placed to allow for transoral imaging. A wine bottle cork notched for the patient’s teeth or gums is excellent for this. We then use halter traction, with the patient’s head resting on a foam donut rather than any type of pin fixation so further intraoperative position changes can be made. If C1 and the odontoid are in an anterolisthesed position, we can optimize the alignment as achieved in the preanesthetic evaluation described above, slowly removing any additional padding, other than the donut, and then dropping the head of the table if necessary under fluoroscopic control to maximize the reduction (Fig. 6-3, top). If C1 and the odontoid are in a retrolisthesed position, rotating the patient’s head about a transverse axis approximately through the ear canals by placing one hand under the chin and the other on the occiput may reduce this completely or partially (Fig. 6-4). This occurs because the center of rotation is above the odontoid, so this motion brings the odontoid anteriorly. These maneuvers may result in full or partial reduction. Biplanar fluoroscopy using two C-arms is used not only for the initial reduction but also for tracking the progress of the operation and screw placement. Excellent visualization of the odontoid in both planes is mandatory. The recent application of fluoroscopic-derived CT imaging and stereotactic guidance systems allows for the use of this modality to substitute for the AP images once the reduction is obtained. Because the scan will only be accurate if no further motion has occurred, it must be used with caution and not relied upon until the final position is obtained.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree