Anterior Lumbar Approach
D. Alex Stroh
Brad W. Moatz
P. Justin Tortolani
DEFINITION
The anterior lumbar approach provides excellent access to the lumbar spine extending from the L2-L3 disc to first segment of the sacrum (S1).
ANATOMY
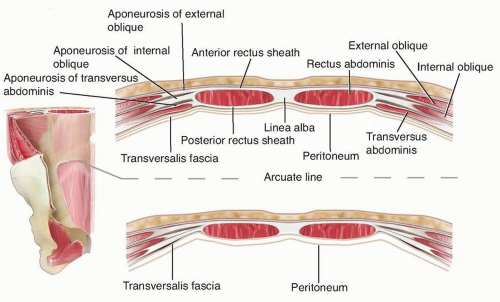
The anterior abdominal wall has a layered configuration that changes depending on whether the approach is proximal or distal to the arcuate line.
Above the arcuate line, the layers in order are skin, subcutaneous fat (containing fascia of Camper and Scarpa), anterior rectus sheath (aponeurosis of the external and internal oblique muscles), rectus muscle, posterior rectus sheath (aponeurosis of the internal oblique and transversus abdominis muscles), transversalis fascia, and peritoneum (FIG 1).
Below the arcuate line, the posterior rectus sheath is not present, and thus the rectus muscle lies directly on the transversalis fascia.
For retroperitoneal exposures, the approach goes through the abdominal wall to the layer of the transversalis fascia and then progresses laterally until this fascia ends, exposing the retroperitoneal fat.
For transperitoneal exposures, the transversalis fascia is divided in the midline, as is the peritoneum, and the exposure proceeds directly posterior to the level of the sacral prominence.
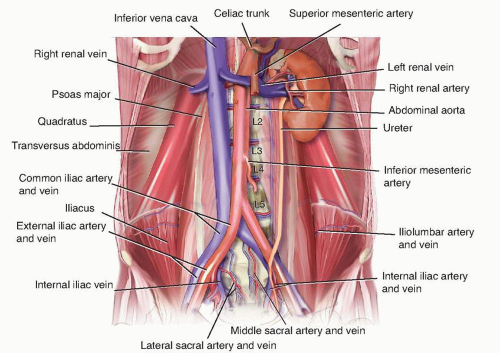
The abdominal contents are retracted to expose the great vessels overlying the anterior lumbar spine.
Key vascular structures with relationship to the spine are shown in FIG 2.
Vascular
The abdominal aorta and the bifurcation into the left and right common iliac arteries lies anterior to the venous system, and the left iliac artery is typically encountered first (L4-L5). In most people, the bifurcation occurs at L4-L5.
Preoperative scrutiny of magnetic resonance imaging (MRI) or computed tomography (CT) scans can help identify the location of the bifurcation, which can be important in planning.
The left renal artery and vein (L2) restrict exposure proximal to L2.
The inferior vena cava (IVC) lies posteriorly and to the right of the aorta, whereas the superior hypogastric plexus lies to the left of the IVC. Because of its deep, rightsided position, mobilization of the IVC from right to left (although less injurious to the sympathetic chain) risks side wall rupture. By contrast, mobilization from left to right places tension on the side wall of the left iliac vein and appropriate precautions must be taken.4
The L5-S1 disc occupies a position between the bifurcation of the aorta and the IVC in most patients, so mobilization of the large vessels is rarely required for access. The middle sacral artery and vein generally branch off of the left common common iliac artery and vein and should be ligated or cauterized if small.
Genitourinary
Left kidney: rarely visualized, surrounded by perinephric fat (L1-L2)
Left ureter: easily retracted anteriorly with peritoneal contents and can be identified by stimulated peristalsis or intraoperative administration of intravenous indigo carmine
Muscular
Psoas (paraspinal, L1-L5)
Neurologic
Sympathetic chain (paraspinal, anterior and medial to psoas)
Presacral plexus (directly over sacrum)
Lumbosacral plexus (posteromedial to and within psoas muscle)
Genitofemoral nerve (lies on anterior aspect of psoas)
Lymphatic
Paraspinal lymphatics and lymph nodes
Lymphatic drainage will appear as a milky white fluid, which is rarely of clinical consequence.
PATIENT HISTORY AND PHYSICAL FINDINGS
Previous abdominal surgery (eg, hysterectomy, hernia repair) can create challenges during this exposure. The presence of midline abdominal mesh, cellulitis or abscess, and a colostomy are relative contraindications to the anterior approach.
Previous exposure of the anterior lumbar spine, particularly if it involved mobilization of the great veins, makes revision approaches much more risky due to the greater likelihood of vascular injury.
Obesity (body mass index above 40 kg/m2) is a relative contraindication to anterior exposure of the lumbar spine due to the depth of the operative field.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs are used to assess the degree of aortic calcification and lumbopelvic deformity.
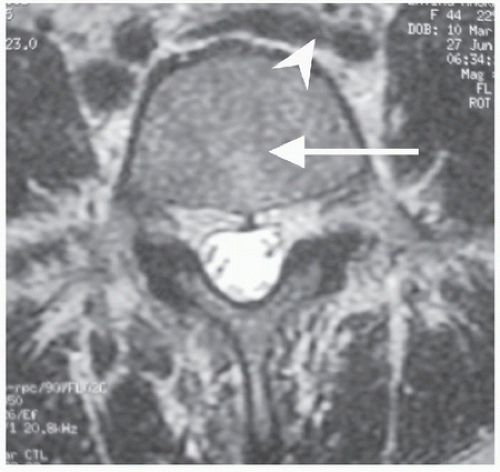
Preoperative axial MRI or CT allows for estimation of the level of the bifurcation of the aorta and IVC (FIG 3).
Routine angiography, CT angiography, or magnetic resonance angiography (MRA) is not necessary unless there is a concern for aberrant anatomy (eg, history of situs inversus).
Preoperative arteriograms, venograms, and prophylactic IVC filters should be considered before any revision approaches to the anterior lumbar spine. Preoperative ureteral stents can also help prevent ureteral injury during revision exposure.
SURGICAL MANAGEMENT
Indications for the anterior lumbar approach are as follows:
Anterior discectomy for interbody fusion, total disc replacement, disc débridement in cases of discitis and vertebral osteomyelitis, and radical discectomy for deformity correction
Anterior corpectomy for tumor resection, radical deformity correction, and vertebral body osteomyelitis
Contraindications are relative and include the following:
Prior anterior approach or other abdominal surgery, fascial mesh, colostomy, pelvic radiation, low bifurcating aorta or vena cava for L5-S1 approaches, untreated paraspinal infection, obesity (body mass index >40 kg/m2), and severe atherosclerosis or aneurysms preventing vascular mobilization
Preoperative Planning
When exposure of the L5-S1 disc is required, the direct anterior lumbar approach should be used in most cases, as the ilium blocks satisfactory access from a lateral approach.
The direct anterior approach is less morbid than the lateral approach to the lumbar spine because the latter involves greater division of the abdominal wall musculature.5
For these reasons, we prefer the direct anterior approach (vs. the lateral approach) even in cases of multilevel disc exposures (eg, lumbar scoliosis correction) unless the L1-L2 disc or L2 vertebra requires exposure or if anterior instrumentation in the form of screw-rod constructs is needed. Anterior plates can be used from a direct anterior approach at L5-S1 and, in some cases, L4-L5, depending on the vascular anatomy.
However, greater mobilization of the great vessels at the level of the bifurcation is needed from a direct anterior versus lateral approach. Thus, a lateral approach may provide better exposure to the spine if the great vessels are anticipated to be difficult to mobilize.
Positioning
The patient is positioned supine over an inflatable pillow (FIG 4A). Inflation of the pillow allows extension of the spine during discectomy and graft placement, if needed. Slight Trendelenburg may aid to retract an obstructive pannus.
The operating room table should allow for free passage of the fluoroscopic C-arm (FIG 4B).
Care should be taken to ensure that the pelvis is level so that true anteroposterior and lateral fluoroscopic images can be easily obtained.
The patient’s arms can be tucked to the side, placed into a “cross” position, or crossed over the chest but must not restrict appropriate fluoroscopic imaging (FIG 4C).
A pulse oximeter may be placed on the patient’s first toe of the left foot in order to provide an early warning for left iliac artery thrombosis or excessive retraction. This is especially important with surgery involving the L4-L5 level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree