Anterior Cruciate Ligament Reconstruction with Autogenous Hamstring Tendon Autografts and EndoButton Femoral Fixation
Roger V. Larson
INDICATIONS/CONTRAINDICATIONS
Injuries to the anterior cruciate ligament (ACL) are common and appear to be increasing. The goal of treating an ACL-insufficient knee is to provide functional stability to prevent recurrent injuries that may lead to subsequent damage to the menisci and articular surfaces. Individuals of any age who wish to remain active in jumping and pivoting sports can become candidates for ACL reconstructive surgery. The success of ACL reconstruction depends on strict adherence to surgical principles, including the selection of a graft of adequate strength and stiffness, graft placement that avoids overstraining and bony impingement, and graft fixation that provides initial strength and stiffness to allow early rehabilitation (5).
Historically, many tissues have been used to serve as ACL substitutes, including autografts, allografts, and synthetic materials. The most common grafts currently used for ACL reconstruction include autogenous bone patellar tendon bone grafts as well as those of quadrupled hamstring tendons. Allografts are being used with increasing frequency. Both patellar tendon and hamstring autogenous grafts
have been shown to be effective in restoring normal anterior knee laxity when used correctly. The use of hamstring tendons offers the advantage of avoiding the extensor mechanism for graft harvest. This is of particular importance in patients with pre-existing patellofemoral disease as well as in situations of revision surgery where the patellar tendon has been used previously. Hamstring tendon grafts are also indicated when cosmesis is of more than a casual concern. There are no absolute contraindications to the use of hamstring tendon autografts for ACL reconstructive surgery with the exception of their unavailability due to previous harvest.
have been shown to be effective in restoring normal anterior knee laxity when used correctly. The use of hamstring tendons offers the advantage of avoiding the extensor mechanism for graft harvest. This is of particular importance in patients with pre-existing patellofemoral disease as well as in situations of revision surgery where the patellar tendon has been used previously. Hamstring tendon grafts are also indicated when cosmesis is of more than a casual concern. There are no absolute contraindications to the use of hamstring tendon autografts for ACL reconstructive surgery with the exception of their unavailability due to previous harvest.
The use of semitendinosus and gracilis tendon autografts for reconstruction of the ACL has been well established (3,8,19). When both the semitendinosus and gracilis tendons are harvested and doubled, the combined four-stranded graft offers several potential advantages over other commonly used autografts such as patellar tendons. The potential advantages of hamstring tendon autografts include increased strength, stiffness characteristics more similar to a normal ACL, a large surface area for graft revascularization or nutrient diffusion, a predictable means of tensioning, and adaptability to precise positioning (15).
When the semitendinosus and gracilis tendons are both doubled and used as an ACL graft, they provide a large-diameter, strong ACL substitute with a significantly greater cross-sectional area of collagen than a 10-mm-wide patellar tendon autograft. The ability to place a hamstring tendon graft precisely is enhanced over that of a patellar tendon, since bone tunnels can be created in the desired locations and then completely filled with collagen tissue. When using patellar tendon grafts with bone blocks on each end, it is necessary to overdrill bone tunnels to fit the bone block. Interference fit screws are frequently used for fixing patellar tendon grafts, and the use of interference fit screws can distort the position of the collagen portion of the graft. The ability of a multistranded graft to obtain nutrition by either diffusion or vascular ingrowth is enhanced over that of a solid graft due to the increased surface area and smaller depth of penetration needed for either revascularization or nutrient diffusion.
Another potential advantage of using hamstring tendons for ACL reconstruction is that the resulting graft tissue has stiffness characteristics that are more similar to a normal ACL, particularly when compared with a patellar tendon autograft (20). The stiffness characteristics at the time of implantation, however, depend on the type of fixation used (9,27,29). Newer techniques of fixing hamstring tendon autografts have alleviated what was once considered a weak link providing initial fixation comparable to or superior to the fixation of bone tendon bone grafts (17,20,32). Soft-tissue grafts such as hamstring tendons also allow for more precise tensioning of the grafts, making overconstraint of the joint less likely. It has also been shown that the process of tendon healing in a bone tunnel occurs relatively early, and thus with improved initial fixation rehabilitation protocols do not need to be significantly different from those used with bone tendon bone grafts (25). It also has been shown by histology and biochemical analysis that post implantation, semitendinosus grafts undergo changes in collagen crimp pattern, cell type, glycosaminoglycan composition, and collagen crosslinking, which suggest a structural change toward that of a normal ACL (14).
The most compelling reason to consider hamstring tendon autografts for ACL reconstruction, however, is the decreased surgical morbidity associated with this procedure. With the use of hamstring tendon autografts, problems of motion and patellofemoral arthrosis are rare (26,28). Several investigators have demonstrated equal success rates when using this technique compared with the use of patellar tendon autografts (1,18,21). These studies, when taken in combination, tend to show increased patient satisfaction with the use of hamstring tendons and slightly, although not significantly, tighter knees when reconstructed with patellar tendon grafts (4,6,7,13,22,24).
PREOPERATIVE PLANNING
Before embarking on surgical treatment of ACL insufficiency, it is imperative to document the abnormal laxity and to obtain radiographs that clearly demonstrate the bony anatomy. The diagnosis of ACL insufficiency can usually be suspected by taking a careful history of the injury and the subsequent symptomatology of the knee. The diagnosis can usually be confirmed by physical examination. In the acute situation, physical examination may be difficult and subsequent examinations to confirm the diagnosis must be planned. The most sensitive test for determining ACL laxity is the Lachman test, in which an anterior force is applied to the tibia with the knee flexed approxiately 25 degrees. This examination when compared with the normal knee can be diagnostic in up to 95% of cases, including acute injuries. Tests that elicit the “pivot shift phenomenon” are helpful in grading the ACL laxity, but can seldom be performed adequately in the acute situation.
An arthrometer can be helpful in demonstrating ACL laxity and documenting the extent of abnormal laxity. It has been shown that in normal individuals there is a 95% chance that there will be a side-to-side difference of less than 2 mm in ACL laxity. If 3 mm or greater of side-to-side difference can be demonstrated with an arthrometer, it can be assumed that the ACL has been injured.
Magnetic resonance imaging (MRI) when performed in the proper plane can be very accurate in diagnosing an injury of the ACL. With careful study of MRI images, partial tears of the ACL can also be identified when either the posterolateral or anteromedial band of the ACL may remain intact. The MRI may also show a typical bone bruising pattern involving the posterior aspect of the lateral tibial plateau and the mid anterior portion of the lateral femoral condyle. This bruising pattern in the “impact zone” is highly suggestive of a torn ACL. The MRI is also important in delineating associated pathology which may influence whether surgical intervention is undertaken or the timing of such intervention.
It is also necessary before embarking on surgical intervention to review the technical points that are important to a successful outcome. As with any surgical procedure, several technical points must be respected to predictably obtain a successful outcome when using hamstring tendon grafts. These include the successful harvest and preparation of the grafts, correct tunnel placement, secure graft fixation, and rehabilitation appropriate for the procedure performed.
SURGERY
Principles
Graft Harvest and Preparation: Technical Points
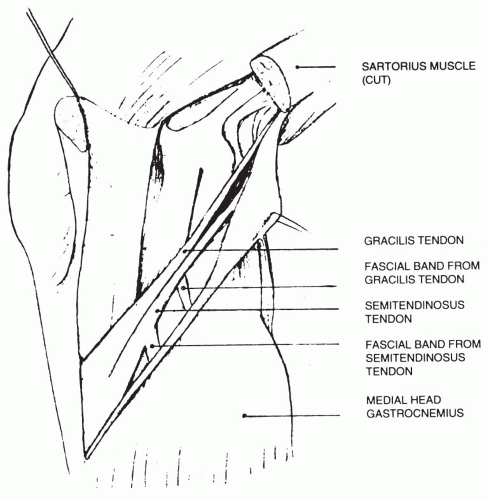
The potential difficulties in harvesting the hamstring tendons and the variability in tissue obtained were once major detriments to the routine use of these grafts. It was also once necessary to obtain considerable graft length to directly fix grafts extraosseously. With newer endoscopic techniques, it is usually only necessary to harvest 22 to 24 cm of tendon, and this amount of tendon can be consistently harvested. The quadrupled graft is generally from 7 to 9 mm in diameter, which is adequate for ACL substitution. It is important to be aware of the anatomy of the semitendinosus and gracilis tendons, particularly of the routinely encountered bands of tissue that extend from the inferior surfaces of each tendon to the medial head of the gastrocnemius (16, 23) (Fig. 16-1). These bands must be identified and sectioned before passing a tendon stripper to ensure that the stripper follows a direct course to the muscle
belly. In cases in which the semitendinosus tendon is of exceptionally high quality and length or where a gracilis tendon is inadequate, a quadrupled semitendinosus tendon graft can be used with some modification of fixation technique (2).
belly. In cases in which the semitendinosus tendon is of exceptionally high quality and length or where a gracilis tendon is inadequate, a quadrupled semitendinosus tendon graft can be used with some modification of fixation technique (2).
Once the tendons have been harvested and sized, it is important to remove muscle tissue from each graft and secure each end of each graft with a nonabsorbable suture. The use of a supplemental suture technique allows for the fixation of every fiber of the graft and for important secondary fixation. It has been shown that slippage under washers, or against interference fit screws, can be considerably reduced by adding a suture technique to the primary source of fixation.
Tunnel Placement
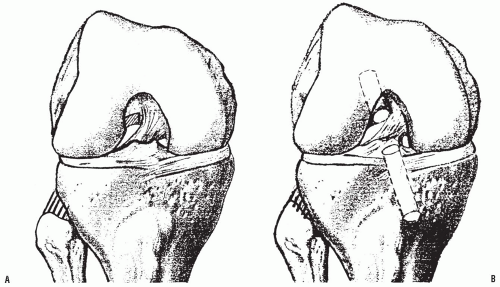
For a successful ACL reconstruction with hamstring tendons or any other graft, the graft must be placed so that it does not overstrain as the knee passes through a full range of motion and so that it does not impinge against the bony anatomy of the intercondylar notch, particularly in terminal extension. This can usually be accomplished by placing the tibial tunnel in a central position and the femoral tunnel at the extreme back of the intercondylar notch at approximately the 10:30 or 1:30 position (30) (Fig. 16-2A). This is at the point where the sidewall and roof of the notch meet. When properly positioned, this provides for a graft that deviates from the vertical position of the posterior cruciate ligament (PCL) at an angle of approximately 25 to 30 degrees. This placement requires careful attention to the start point of the tibial tunnel, particularly when the femoral tunnel is to be created through the tibial tunnel (12). When ideally placed, the ACL graft will avoid contact with the lateral wall of the intercondylar notch and will barely touch the roof of the intercondylar notch at full terminal extension. The proper placement will also avoid excessive impingement with the PCL, particularly in hyperflexion. The femoral tunnel should extend to or near the “over-the-top” area. It is acceptable to blow out the back wall of the notch when creating the femoral tunnel, and in fact this would ensure that the tunnel is far enough to the back of the notch.
With EndoButton (EndoButtonTM, Smith and Nephew, Corp., Boston, MA) fixation on the femur, blowing out of the back wall of the tunnel does not compromise fixation strength. The leading edge of the femoral tunnel should be chamfered to avoid a sharp corner that could traumatize the ACL substitute (21). The proper position of the femoral tunnel is demonstrated in Figure 16-2B.
With EndoButton (EndoButtonTM, Smith and Nephew, Corp., Boston, MA) fixation on the femur, blowing out of the back wall of the tunnel does not compromise fixation strength. The leading edge of the femoral tunnel should be chamfered to avoid a sharp corner that could traumatize the ACL substitute (21). The proper position of the femoral tunnel is demonstrated in Figure 16-2B.
The tibial tunnel should be created far enough posterior in the notch so that at full terminal extension the graft will barely graze the superior notch but will not be impinged or “guillotined” by it. It has been shown that impinged grafts remain inflamed and their MRI signals do not return to normal (10). With extreme impingement knee extension can be blocked and anterior graft fibers can be broken, creating a “cyclops” lesion (11). The tibial tunnel should also be placed in a position that avoids lateral notch impingement. If the femoral tunnel is to be drilled through the tibial tunnel, the start point must be medial enough to allow drilling of the femoral tunnel at the appropriate position. This usually requires starting the tibial tunnel within the fibers of the medial collateral ligament. It is appropriate when possible to fit the tunnels to the anatomic notch. Routine notchplasty should be discouraged, since with notchplasty the exposed cancellous surfaces often form fibrocartilage and eventual reformation of the anatomic notch.
Graft Fixation Options
The goal of ACL reconstruction is to provide an ACL substitute that will reproduce as nearly as possible the functional properties of the native ACL. For the graft to perform this function it must be placed in a near isometric or “physiometric” position, and it must have the strength and stiffness to mimic ACL function. During the first 6 to 12 weeks, before biologic healing of the grafts to the bone tunnels, the behavior of the graft depends not only on the material properties of the graft being used but also on the method of graft fixation used. The graft/fixation construct must be strong enough to avoid failure with tensile loading, and it must be stiff enough to restore the load displacement response of a normal ACL and secure enough to resist slippage with cyclic loading.
The important parameter to consider in fixation strength is yield load. This is the point at which plastic deformation begins and functional failure occurs (17). Most fixation devices used for the femoral fixation of hamstring tendon grafts have yield loads of between 350 to 800 newtons (N). The newer-generation fixation devices may increase this strength to 1,200 N. Techniques of femoral fixation that involve rigid cross-pin fixation provide the greatest initial strength.
Tibial fixation of hamstring tendon grafts is a more problematic consideration than femoral fixation. Initial fixation yield strength ranges from approximately 350 N for an interference fit screw to 1,160 N for tandem screws and washers. Graft slippage is an additional consideration, particularly with tibial fixation methods.
The initial stiffness of an ACL substitute is highly dependent on the fixation method used. Howell has pointed out that the stiffness of fixation methods is from four to 40 times less than that of grafts used. Increasing the stiffness of an ACL replacement would best be achieved, therefore, by selecting fixation methods with higher stiffness and not by shortening or increasing the cross-sectional area of the grafts used (33). The stiffness of a doubled semitendinosus and gracilis tendon complex alone is approximately 1,000 N/mm. The stiffness of various fixation devices of hamstring tendons varies from approximately 25 to 230 N/mm. A normal ACL has a stiffness of approximately 200 N/mm.
Slippage of grafts from their point of fixation during cyclic loading is a major early problem that can compromise results (31). The slippage around interference fit screws is considerably greater than that which occurs with a cross-pin technique. The slippage around an interference fit screw during cyclic loading is also quite dependent on bone quality, which can be extremely variable in a patient population. When using screw and washer fixation of soft-tissue grafts, slippage can be considerably reduced by utilizing an additional suture technique to secure the graft beneath the soft-tissue washer. Supplemental suture fixation for grafts fixed with interference fit screws is highly recommended.
Hamstring Graft Fixation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree