Anterior Cervicothoracic Approach
C. Chambliss Harrod
Christian Klare
Todd J. Albert
INDICATIONS/CONTRAINDICATIONS
The cervicothoracic junction anatomically and biomechanically is a complex region transitioning from the lordotic highly mobile cervical spine to the kyphotic, rigid thoracic spine (1). Anatomically, complex vascular, respiratory, alimentary viscera combined with local neurologic and osseous structures place a high demand on appropriate approach selection to obtain good outcomes (2). The spinal cord in this region is at its widest due to the cervical enlargement, while the bony canal volume is the smallest. Additionally, the upper thoracic cord is a watershed area with the anterior spinal blood supply transitioning from the vertebral and cervical arteries to the intercostals. Anterior- and posterior-based approaches both carry advantages and disadvantages. Careful analysis of disease etiology, extent, and surgical goals allows the correct approach to obtain surgical goals— namely, decompression, stabilization, and arthrodesis. Posterior-based approaches include direct posterior (laminectomy) and posterolateral approaches (transpedicular, transfacet, costotransversectomy, lateral extracavitary).
A number of anterior approaches to the cervicothoracic junction have been described including low cervical-supraclavicular (Smith-Robinson variant), transmanubrial-transclavicular, the modified anterior, the transsternal, and the high transthoracic (third rib resection) (3, 4, 5, 6, 7, 8, 9, 10, 11, 12,14). Each of these techniques has its own unique advantages and disadvantages. Experience of the surgeon, cosurgeon availability, and familiarity with the approach and anatomy of the patient are of utmost importance when deciding on which approach to use. We discuss the transmanubrial-transclavicular approach, which offers extensive, simultaneous exposure of the lower cervical and upper thoracic vertebral bodies of the cervicothoracic junction.
Pathologic processes occurring at the cervicothoracic junction typically involve the vertebral bodies, making an anterior approach preferred. The most common indications for surgical intervention at the cervicothoracic junction include neoplasms (metastatic more common than primary), infections, and fractures (15, 16, 17). Metastatic lesions widely outnumber primary lesions in all regions of the spine. Lymphomas, myelomas as well as solid cancers such as lung, breast, prostate, renal, gastrointestinal, and thyroid lesions are common metastatic or systemic neoplasias. Primary lesions can be benign (hemangiomas, osteochondromas, osteoid osteomas, aneurysmal bone cysts, giant cell tumors), malignant (osteosarcomas, chondrosarcomas), or locally invasive chordomas less frequently. Perhaps, the most common spinal lesion to the cervicothoracic spine is a direct local invasion of a primary pulmonary mass (Pancoast tumor, historically tuberculomas) transpleural to the osseous spine or epidural space. Although these lesions may be approached posterolaterally in this region of the spine, sacrifice of unilateral or bilateral C8 and T1 nerve roots can be devastating and avoided by utilizing anterior resection and reconstructions (13). Also, mediastinal tumors such as neuroblastomas or ganglioneuromas can impinge on the spine or epidural space. Often, the natural progression of diseases at the cervicothoracic junction includes anterior collapse of the vertebral bodies with resultant kyphosis increasing the difficulty in obtaining adequate surgical exposure. Commonly, these procedures will need additional supplemental posterior stabilization.
PREOPERATIVE PREPARATION
Adequate preoperative planning entails two main factors: understanding the anatomy of the cervicothoracic junction and the thoracic inlet and adequately imaging/localizing the pathology. Cranially, the Smith-Robinson anteromedial approach to the lower cervical spine can be utilized with dissection proceeding through the platysma, between the strap muscles, trachea, esophagus, thyroid, and parathyroid glands medially and the sternocleidomastoid (SCM), carotid sheath (common carotid artery, internal jugular vein, and vagus nerve) laterally. Caudally, the first thoracic structures encountered are osseous and include the manubrium, sternum, medial third of the clavicle, and their articulations in addition to the insertions of the strap and SCM muscles. These structures protect the thymus, great vessels, thoracic duct, and pleural structures laterally. Notably, the brachiocephalic and subclavian veins right brachiocephalic artery and arch of the aorta, left subclavian artery, the carotid sheath, and recurrent laryngeal nerves (RLNs) will be encountered.
Imaging of this area is often difficult to assess with plain radiography though “winking eye” (pedicle erosions) can be seen while also being classified as osteolytic or osteoblastic. Swimmer’s lateral, oblique, flexion-extension views can aid in visualizing the junction, neuroforamen, and destabilizing nature. However, computed tomography better assesses both fractures and the extent of osseous pathology. Most importantly, MRI best assesses the extent of spinal cord compression with or without intradural extension. Gadolinium administration with enhancement is particularly useful with neoplasms and infection associated with abscess formation. Vascularity of lesions is important to identify which patients might benefit from arteriography and embolization to avoid catastrophic blood loss. Lastly, careful attention to the lateral extension cervical spine radiographs and midsagittal CT or MRI images will allow identification of the most caudal vertebra or disc space to be accessed without splitting midline osseous structures. In thin, long-necked patients, T2 is possible via the standard anterior approach to the neck. Contrastingly, short-necked patients can make access even to C6-C7 difficult. The following technique relates to the anterior transmanubrialtransclavicular approach to the cervicothoracic junction.
PATIENT POSITIONING
The patient should be positioned supine on a regular radiolucent operating table with a rolled towel between the scapulae, allowing for slight extension of the neck. We use multimodality neuromonitoring employed with a combination of transcranial motor evoked potentials, somatosensory evoked potentials, and free-running EMGs to monitor the spinal cord throughout the procedure. After preintubation motor baseline potentials are obtained, intubation is performed along with appropriate hemodynamic access and monitoring via the anesthesia team. The table is then reversed 180 degrees from anesthesia to allow additional room for fluoroscopic imaging during the procedure. If intraoperative traction is used, Gardner-Wells skull tongs are placed after induction of anesthesia with baseline of 10-pound traction placed with aid of a Mayfield horseshoe head holder. We do not routinely use them for cases needing corpectomy at T1 or below. Care must be taken to pad bony prominences and ensure safety of peripheral nerves. The patient’s arms should be tucked at his or her sides. We tape down the shoulders firmly to help with fluoroscopic evaluation of the cervicothoracic junction (or the most caudal cervical vertebrae). We also monitor the brachial plexus and check the signals after taping of the shoulders. We do clip any chest hair on male patients and then drape out our operative field from the lips to 3 cm below the xiphoid process caudally and laterally along the midaxillary lines crossing the acromioclavicular joints and then cranially to the SCM insertions at the mastoid processes. After scrubbing skin and prepping with ChloraPrep, a World Health Organization “time-out” is performed to verify the details of the procedure and equipment and review major intraoperative risks with the anesthesia, surgical, and nursing teams.
TECHNIQUE
Low Cervical Approach (Smith-Robinson)
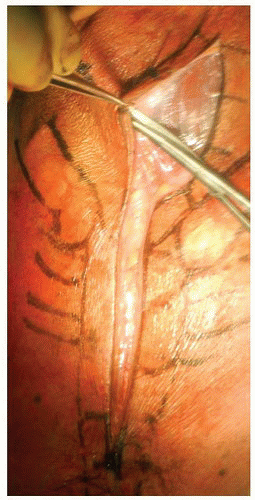
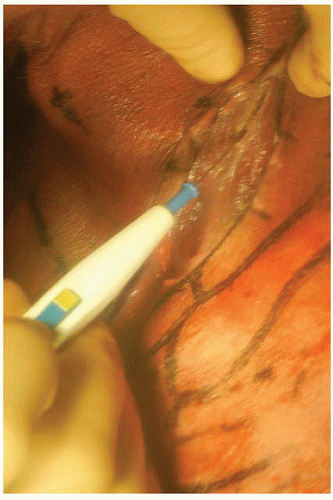
We utilize an anterolateral oblique skin incision along the anterior border of the SCM muscle, extending to the sternal notch and continued along the anterior aspect of the sternum distal to the manubriosternal junction (Fig. 7-1). Supraplatysmal subcutaneous flaps are elevated (Fig. 7-2), and the platysma is split in line with the skin incision using Bovie electrocautery (Fig. 7-3). Subplatysmal flaps are then created with Metzenbaum scissors caudally to the sternal notch, sternoclavicular (SC) joint, and medial clavicle laterally. The external jugular veins may be sacrificed for increased exposure if necessary. Knowledge of the fascial layers of the neck is mandatory for safe dissection. The superficial cervical fascia (splits into superficial and deep layers enveloping the platysma), deep investing cervical fascia (splits anteriorly to envelop the SCM and posteriorly the trapezius muscles), pretracheal fascia (separates the trachea-laryngeal cartilage-esophagus medially from the carotid sheath laterally), and prevertebral fascia (between the longus colli muscles overlying the vertebrae and discs) compose the cervical fascia layers. The retropharyngeal space runs from the clivus into the mediastinum ventral to the prevertebral fascia. Careful dissection of the deep investing cervical fascia is performed medial to the SCM muscle, allowing for the mobilization and release of the omohyoid muscle (Fig. 7-4). This muscle does not typically need to be reapproximated or repaired unless operating on a vocalist.
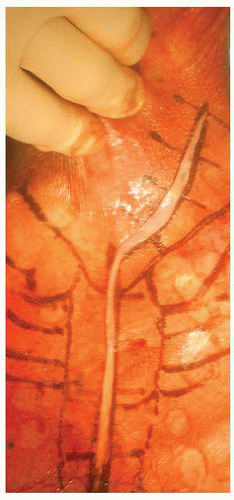 FIGURE 7-1 The field has been prepped and draped, and the combined oblique low cervical and midline transmanubrial incision has been made. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree