Antegrade Intramedullary Nailing of the Femur
Navid M. Ziran
Bruce H. Ziran
DEFINITION
A femoral shaft fracture is any fracture of the femoral diaphysis from 5 cm below the lesser trochanter to within 6 to 8 cm of the distal femoral articular surface.
Some fracture lines extend proximal or distal to the shaft and are therefore not considered shaft fractures.
This description is mostly semantic, as the more important aspect of definition is understanding the “personality” of the fracture.
Fractures whose essential fracture element is diaphyseal with an extension into the outer regions are different from fractures whose essential fracture element is subtrochanteric or supracondylar with extension into the diaphysis.
In some circumstances, proximal and/or distal femur involvement may warrant a different treatment (ie, plating, cephalomedullary nail, etc.) than intramedullary nailing.
For the purposes of this chapter, we will focus on fractures that are amenable to antegrade nailing.30
The Abbreviated Injury Scale (AIS) score for an isolated femoral shaft fracture is three, thus making the Injury Severity Score for an isolated femoral shaft fracture a nine.
Open fractures are usually graded according to the Gustilo-Anderson classification, but this classification system was designed for the tibia—a subcutaneous bone. Thus, if absorbed energy is considered, significantly more energy would be required to fracture a femur because there is more soft tissue envelope around a femur than around a tibia. Nonetheless, this system is widely employed in the femur for descriptive purposes.
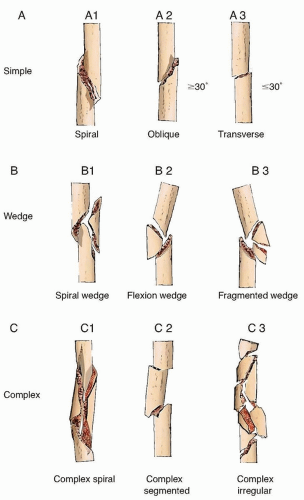
The fracture classification system previously used most commonly was the Winquist classification, but it has been modified and standardized with the AO Orthopaedic Trauma Association (AO/OTA) classification, which is the recommended system.22, 40 In the AO classification, the femur is number 32 and further subdivided in simple, wedge, and complex fractures as shown (FIG 1).
ANATOMY
The femur is the longest bone in the body. It is subject to very high stresses in the proximal region because of the need to transition the forces of body weight via a lever arm (femoral neck) into more axial forces distally. As such, the subtrochanteric area is subject to very high stresses.19
The femur is flat on the anterior and lateral surfaces. On the posterior femur surface, there is a taper that is confluent with the linea aspera.
The linea aspera is a very thick fascial structure and frequently remains in continuity but separates from the femur.
Entrapment of the linea aspera between the fracture ends may impede closed fracture reduction, especially with simple fracture patterns. The bone ends may need to be “unwound” to effect a reduction.
The linea aspera protects many perforating periosteal vessels and may help explain the high healing rate of femoral shaft fractures (about 95%).
There are three thigh compartments: anterior, posterior, and medial.
Thigh compartment syndrome may occur and generally involves the anterior compartment. Frequently, release of the anterior compartment will relieve pressure.
The proximity of the gluteal compartment places it at risk as well. It should also be considered with compartment syndromes.
The femur has an anterior bow and is not a circular bone.
Both anterior and lateral bowing is important to recognize, especially if abnormal (eg, metabolic bone disease).
The anterior bow has an average radius of curvature of about 120 cm.
If there is excessive bowing, good preoperative planning is needed.
Surgical options for such abnormal bowing include plate fixation or a controlled osteotomy to allow nail placement.22
The endosteal diameter is important to recognize, especially with young or sclerotic bone.
Normal aging and osteoporosis results in a biomechanical adaptation of enlarged inner diameter. Thus, elderly individuals may have a larger diameter femoral shaft with a thinner cortex. As in other cylindrical tubes, the bending rigidity of the femur is roughly proportional to the radius to the fourth power.
The vascular supply to the femur is a nutrient artery off the second perforating branch of the profunda femoris, entering posteriorly along the linea aspera.
Normally, periosteal arterial branches supply the outer one-quarter to one-third of the cortex; the direction of blood flow is directed centrifugally from the high-pressure medullary arterial system to the low-pressure periosteal system.27
Once fracture occurs, a reversal of blood flow occurs with blood flowing centripetally from periosteal vessels directed radially inward (because the higher pressure intramedullary system is disrupted).26
PATHOGENESIS
Femoral shaft fractures are high-energy injuries in the young; in the elderly, simple falls from ground level are sufficient to fracture the femur.
Fracture patterns give clues to the mechanism.
For example, a simple transverse fracture with a butterfly fragment is due to a bending force (eg, T-bone vehicle crash).
Spiral fracture patterns are usually due to torsional forces.
Indirect high-energy mechanisms, such as a fall from a height or motor vehicle crashes, will usually incur a significant initial deformity during the fracture process.
The active and passive recoil of the muscle soft tissue envelope will decrease the initial displacement. Thus, the extent of soft tissue injury can be difficult to appreciate.
Open fractures in this setting are usually “inside-out” injuries.
Direct mechanism fractures are from ballistic injuries, crush injuries, or other weapons (eg, chainsaw, axe).
With these injuries, there may be less initial displacement of the fracture and soft tissues, but the amount of soft tissue injury can still be extensive.
In ballistic injuries, the shock and cavitation can result in extensive tissue necrosis.
In both direct and indirect mechanisms, it is important to recognize that the zone of tissue injury may extend well beyond the fracture site.
NATURAL HISTORY
1500s: The earliest record of intramedullary splinting is from the Spanish and Aztecs who used wooden sticks to treat pseudarthroses.
1800s: Germans used ivory pegs with interlocking holes. In 1890, Gluck used the first interlocking ivory nail with interlocking pegs.
Early 1900s: In the early 20th century, the natural history of femur fractures was poor.
The mortality of wartime femur fracture before and during World War I (WWI) was approximately 80%. Serendipitous use of a wheeled splint for transport off the battlefield resulted in a precipitous drop in the mortality rate (the Thomas splint was thus developed). During WWI, Hey Groves used metallic rods for the treatment of gunshot wounds but there was a very high infection rate and it was not universally accepted.
Because surgical techniques were primitive in those times, fears about infection and surgical complications resulted in most fractures being treated in traction.
The outcome was frequently a shortened, rotated, varus malunion of the femur. Additional problems such as decubiti, venous thromboembolism, and pulmonary infections with prolonged bed rest resulted in high morbidity and mortality.
1930-1940s: In 1931, Smith-Petersen reported the first successful use of stainless steel nail for the treatment of femoral neck fractures—the Smith-Petersen nail sparked an interest in the application of intramedullary devices for fracture treatment.
Gerhardt Küntscher is considered the father of intramedullary nailing and much of his interest in intramedullary devices originated from his use of the Smith-Petersen nail for femoral neck fractures.
Küntscher’s first nail used (1940) was a V-shaped stainless steel antegrade nail; this V-shaped design had evolved to a cloverleaf design by the late 1940s. Küntscher’s original technique was on open nailing (ie, exposing the fracture site). In Western nations, poor surgical technique resulted in high rates of infection and nonunion.
1950-1960s: The 1950s saw the advent of intramedullary reamers and interlocking screws with Modny and Bambara introducing the transfixion intramedullary nail in 1953. Intramedullary nailing enthusiasm diminished in the 1960s in favor of compression plating, but by the late 1970s, renewed interest in developing closed nailing techniques appeared.5, 22
1970s: With diminished interest in compression plating and improved reaming methods, closed nailing gained popularity by the late 1970s. The dominant design was the slotted cloverleaf-shaped interlocked nail, the AO, and Gross-Kempf nails.
1980s: Küntscher’s method was resurrected in the United States by early traumatologists, such as S. Hansen and M. Chapman, who used Küntscher’s newer technique of “closed” femoral nailing.
In the late 1980s, Brumback and colleagues reported the high success rate (98%) of reamed, statically locked intramedullary nails.10, 11
The success rate of femoral nailing using closed technique resulted in low morbidity and began a change in practice to what we perform today.
Early studies outlined the benefits of early reamed femoral nailing.
1990s-present: As survival of more traumatized patients increased, a subset of patients who may benefit from “subacute” nailing developed.
Later studies identified patients at risk (eg, pulmonary injury, incomplete resuscitation, and brain injury) who benefited from stabilization of life-threatening injuries before fixation.
This reflects the paradigm shift from early total care (ETC) to damage control orthopaedics (DCO).4, 24, 31
Although some have advocated plating in such cases, there have been no studies demonstrating the superiority of one method over the other in terms of patient survival.6
PATIENT HISTORY AND PHYSICAL FINDINGS
Relevant history includes age, sex, mechanism of injury, associated injuries (ie, chest/head) loss of consciousness, weakness, paralysis, or loss of sensation.
Metabolic conditions and any musculoskeletal conditions should be elucidated if possible.
Patients should be evaluated according to the advanced trauma life support (ATLS) guidelines.
Particular attention should be given to hypotension because femoral shaft fractures can be associated with up to 1000 to 1500 mL of blood loss. Although not solely responsible for hypotension, femoral shaft fractures can be a contributory source.
Upon evaluation by first responders, the limb should be aligned and placed in a traction device, such as a Sager splint or a Thomas splint.
These initial splints should be removed and replaced with skeletal or limb traction because of the risk of skin problems in the perineal or ischial and ankle areas. Traction improves patient comfort, restores length, and tightens the surrounding muscles. The taut surrounding musculature decreases potential space for blood loss, provides a tamponade effect to hemorrhage, and serves as a soft tissue stabilizer to the fracture fragments.
It is essential to inspect the affected limb for any open wounds, swelling, and ecchymosis (see Exam Table for Pelvis and Lower Extremity Trauma, page 1).
The extent of the open wound does not always correlate with the degree of soft tissue or fascial stripping due to the fracture.
Vascular evaluation should include manual palpation of the popliteal, posterior tibial, and dorsalis pedis pulses.
It is important to understand that a pulse is a pressure wave and can still be present in the absence of flow; alternatively, the absence of a pulse does not always mean absence of flow. A Doppler ultrasound device should be used in cases where a pulse cannot be palpated.
Hypotension with peripheral vasoconstriction may accompany such injuries.
The limb should be aligned before vascular examination.
Asymmetric or absent pulses warrant a measurement of the ankle-brachial index (ABI). An ABI less than 0.9 is abnormal.
Arteriography should be considered to rule out vascular injury.
Neurologic evaluation includes motor and sensory function of the femoral and sciatic nerve.
The femoral nerve may be difficult to examine secondary to pain associated with the fracture.
Sciatic nerve function can be evaluated for both peroneal and tibial branches.
The peroneal branch is tested with ankle and toe dorsiflexion and sensation on the top of the foot.
Tibial branch function is tested with ankle and toe plantarflexion as well as sensation to the sole of the foot.
IMAGING AND OTHER DIAGNOSTIC STUDIES
The tenet of imaging a joint above and a joint below should be followed.
Good anteroposterior (AP) and lateral views of the hip, femur, and knee are required.
Such films can be obtained in the operating room but are essential in planning because the presence of a femoral neck fracture or a fracture about the knee will greatly change the operative tactic.
Attempts should be made to get an internal rotation AP view of the femoral neck. However, with current trauma algorithms, the commonality of the pelvic computed tomography (CT) scan allows imaging of the femoral neck. The scan should be viewed before deciding on the surgical tactic.
If radiographs are normal but the clinical examination suggests injury (eg, inability to bear weight, pain out of proportion to injury), coronal magnetic resonance imaging (MRI) may elucidate an occult fracture.
CT scanning in these situations may not be sensitive enough to find such fractures.
Occult femoral fractures may be hard to identify with preoperative radiographs.
Use of CT scans of the abdomen that go to the level of the femoral neck have been found to be sensitive enough to identify such occult femoral neck fractures and should be done for most cases.35
DIFFERENTIAL DIAGNOSIS
Other injuries may occur concomitantly with femur fractures, including pelvic fractures, acetabular fractures, femoral neck fractures, and ligamentous injuries to the knee.
If an effusion is present in the knee, the index of suspicion for a knee injury should be elevated.
Distal femur fracture may also occur but may not be radiographically evident, especially in osteoporotic bone.
In the absence of a reasonable mechanism, other causes for fracture such as metabolic bone disease or metastatic (or primary) fracture should be ruled out.
Although rare, compartment syndrome without fracture will also manifest as thigh pain with inability to bear weight. In these cases, the physician should perform serial examinations for compartment syndrome, measure compartment pressures if the clinical examination is equivocal or indeterminate, and have a low threshold for fasciotomy.
NONOPERATIVE MANAGEMENT
Nonoperative management has typically been reserved for patients who are unfit for surgery, patients who are quadriplegic or paraplegic, patients in whom the benefits do not outweigh the risks, or other precluding factors (eg, active infection).
Truly nondisplaced fractures in a compliant and able patient may also be treated nonoperatively.
Infants and young children may also be treated nonoperatively because of their ability to remodel.
Nonoperative management consists of bed rest and skeletal traction (either through the distal femur or proximal tibia) with 20 to 30 pounds of weight.
Attention should be given to mechanical and pharmacologic venous thromboembolism prophylaxis if this treatment is considered.
SURGICAL MANAGEMENT
Isolated femur fractures are not urgent. Appropriate evaluation and medical clearance should be performed to stabilize the patient expeditiously. Definitive treatment should be performed when appropriate resources are available (eg, knowledgeable staff, anesthesia,). It is not necessary to stabilize such fractures during off shifts unless indicated for other reasons (eg, open fracture, polytrauma).
In the multiple injured patient (Injury Severity Score of more than 18), with pulmonary compromise or head injury, fracture fixation should be delayed until suitably cleared for surgical intervention, and damage control methods with use of a temporary external fixator should be considered.3, 6, 23, 29
Patients with isolated femur fractures should have some method of traction, pain control, and deep vein thrombosis prophylaxis while awaiting surgical intervention.
Currently, statically locked femoral nailing with limited reaming is the standard of care.
The studies by Brumback et al7, 8, 9, 10, 11 determined that statically locked nails do not affect healing and avoid the problems of malrotation and shortening. Unreamed nails were proposed to limit effects of canal fill and the theoretical concern of infection. Neither concern was proven, and, in fact, small unreamed nails had the same problems as in the tibia: higher rates of nonunion. Currently, the “ream-to-fit” technique is used.38
Recently, the reamer-irrigator-aspirator (RIA) has been used to minimize the pressure-induced embolization from the marrow. As studies are ongoing and controversial, this method may reduce the risks in the multiply injured patients.33, 39
Open fractures can be safely nailed if a thorough irrigation and débridement is performed.
Absorbable antibiotic beads (calcium sulfate, not calcium phosphate, mixed with vancomycin or tobramycin) can be used at the time of definitive closure to provide local antibiotic delivery.28
In severely contaminated fractures, a staged approach using temporary antibiotic beads (using polymethylmethacrylate mixed with vancomycin or tobramycin) and external fixation, followed by nailing within 2 weeks (with or without use of absorbable beads), can be employed.
If there is no pin tract infection, conversion from external fixation to intramedullary nailing is best performed within 10 to 14 days after external fixation to minimize infection risk.13
In such cases, the risk of infection is increased but acceptable in lieu of prolonged bed rest.
Because of deforming forces in proximal femur fractures, the proximal segment tends to flex and externally rotate.
Care should be taken to ensure that the posterior cortex of the proximal fragment is not inadvertently reamed away.
In distal fractures, the distal segment tends to flex at the knee (recurvatum of fracture).
With distal fractures, care should be taken to avoid varus or valgus reduction. This can occur because the opening of the medullary canal distally does not have intimate contact with the nail and does not “self-align.”
Transverse fractures may contain a segment of intact linea aspera that peels off the posterior aspect and may get entrapped in the fracture.
It can result in shortening that may be difficult to overcome without either “unwinding” the fracture or opening the fracture site.
In skeletally mature children, intramedullary nailing offers the same benefits as in adults.
Attention should be paid to adolescents with very valgus neck angles, as some have hypothesized that this can increase the risk of avascular necrosis of the femoral head. However, with newer implants such as trochanteric entry or lateral entry nails, many of these concerns can be alleviated.
Preoperative Planning
All films should be reviewed, with particular attention paid to the presence of an ipsilateral femoral neck fracture.
The overall condition of the patient and any associated injuries should be contemplated before embarking on a surgical tactic.
In the presence of pelvic or acetabular fracture, pregnancy, or obesity, one should consider a more elegant tactic, such as retrograde nailing, as opposed to antegrade nailing.
If suitable, antegrade nailing in the supine position can be safely performed with proper positioning and knowledge.
Several options have to be considered during preoperative planning. They include the following:
Table: fracture table or radiolucent
Position: supine or lateral
Entry point: piriformis or trochanteric
Type of nail: cephalomedullary or standard
Use of traction: skeletal, boot, or manual
Reduction tools: Crutch, ball spike pushers, 5.0- or 6.0-mm Schanz screws with T-handles, mallet, F tool; in the remote case the surgeon needs to perform an open reduction, conventional reduction clamps such as Weber clamps or Verbrugge-type clamps can be useful.
As mentioned before, strong consideration should be given to checking fine-cut CT scans to evaluate the femoral neck. Before the surgeon leaves the operating room, he or she should ensure that femoral intramedullary nail fixation has resulted in satisfactory: (1) length, (2) alignment, (3) rotation, and (4) intact femoral neck (in cases where a piriformis-entry nail was used).
Positioning
Fracture table
Standard fracture tables (eg, those used commonly for hip fractures) can be used for antegrade femoral nailing but are best used for supine position nailing.
A large and well-padded perineal post should be used.
Traction should be used sparingly and only when needed.
The legs should be scissored to facilitate imaging and allow for appropriate countertraction. Placing the opposite leg in lithotomy position can allow rotation of the pelvis when traction is applied.
The ability to image all aspects of the femur should be verified before preparing and draping (FIG 2A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree