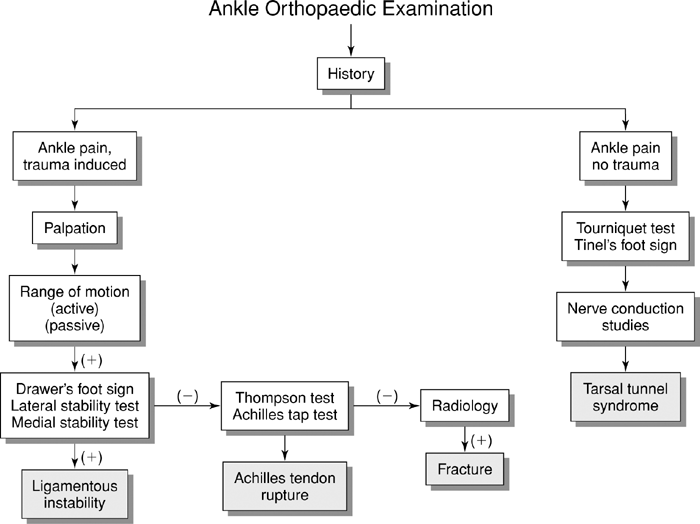
Ankle Orthopaedic Tests
Palpation
Medial Aspect
Descriptive Anatomy
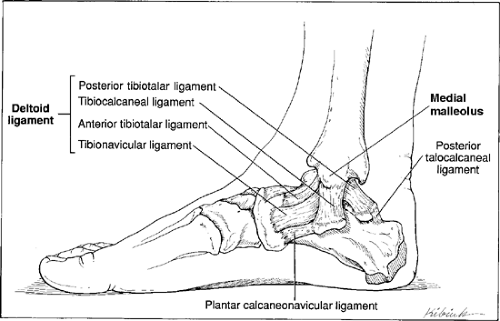
The medial malleolus is the most distal prominence of the tibia. It embraces the medial aspect of the talus and gives the ankle joint bony stability. Attached to the malleolus is the strong deltoid ligament, which connects with three tarsal bones: the talus, navicular, and calcaneus. The deltoid is a four-part ligament that is named according to its attachments: tibionavicular, anterior and posterior tibiotalar, and tibiocalcaneal (Fig. 15-1). The deltoid ligament strengthens and provides medial stability to the ankle joint and holds the calcaneus and navicular bones against the talus. A common injury is a forceful eversion of the foot that causes an avulsion fracture of the deltoid ligament on the medial malleolus.
Procedure
With the patient’s weight off that foot, palpate the medial malleolus and deltoid ligament for tenderness and/or swelling (Fig. 15-2). Tenderness and/or swelling secondary to trauma may indicate periosteal contusion, sprain, or avulsion of the deltoid ligament.
Descriptive Anatomy
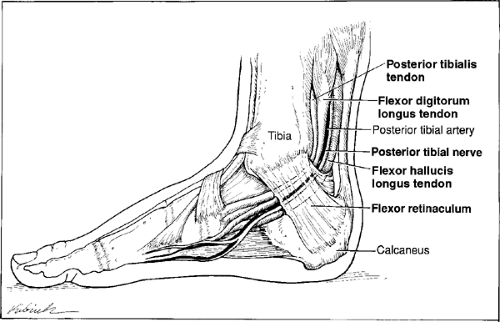
The posterior tibial tendon passes posterior to the medial malleolus and inserts into the tuberosity of the navicular bone (Fig. 15-3). The action of the muscle is to plantar-flex the ankle and invert the foot. The flexor digitorum longus tendon is posterior to the posterior tibial tendon; it closely follows the tibia and passes behind the medial malleolus (Fig. 15-3). It inserts into the distal phalanges of the lateral four digits. The action of the muscle is to plantar-flex the ankle and flex all of the joints of the last four toes. The flexor hallucis longus tendon is posterior to the flexor digitorum longus tendon, and it passes behind the ankle joint, not posterior to the medial malleolus. It inserts into the base of the distal phalanx of the great toe (Fig. 15-3). Its action is to flex the great toe.
Procedure
To palpate the tibialis posterior tendon, invert and plantar-flex the patient’s foot. Palpate medial to the tibia posterior to the medial malleolus (Fig. 15-4). Note the continuity of the tendon and any tenderness or swelling. Tenderness and/or swelling may indicate a strain secondary to trauma or tendinitis. Loss of continuity and a valgus foot secondary to trauma may indicate a ruptured tendon.
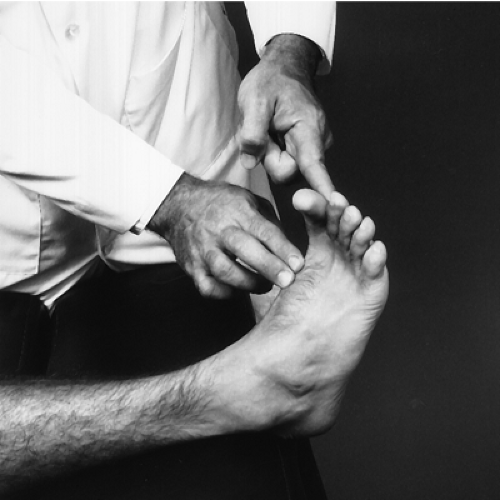
Palpate the flexor digitorum longus tendon, which is posterior to the tibialis posterior tendon. With one hand, resist flexion of the patient’s toes, and with the other hand palpate the tendon (Fig. 15-5). Note any tenderness, swelling, or crepitus. These signs may indicate a strain or tendinitis of the tendon. The flexor hallucis longus tendon is not palpable and not described in this book.
Descriptive Anatomy
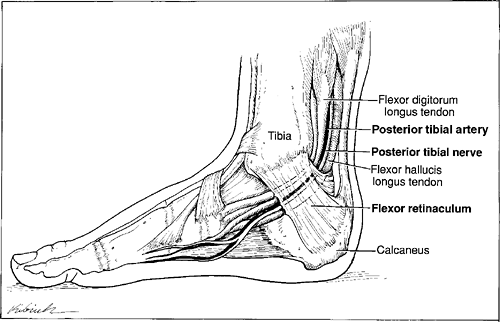
The posterior tibial artery runs between the tendons of the flexor digitorum longus and flexor hallucis longus muscles. This artery is the major blood supply to the foot. The tibial nerve is a branch of the sciatic nerve. It runs with the posterior tibial artery under the flexor retinaculum of the ankle and posterior to the medial malleolus (Fig. 15-6). The flexor retinaculum may become constricted and cause a neurovascular deficit to the foot similar to carpal tunnel in the wrist.
Procedure
Using light pressure with your middle and index finger, palpate the posterior tibial artery (Fig. 15-7). Note the amplitude and compare bilaterally. A decrease in the pulse amplitude may indicate a compression of the posterior tibial artery. The tibial nerve is difficult at best to palpate and is not discussed in this book. It is an important nerve supply to the sole of the foot.
Lateral Aspect
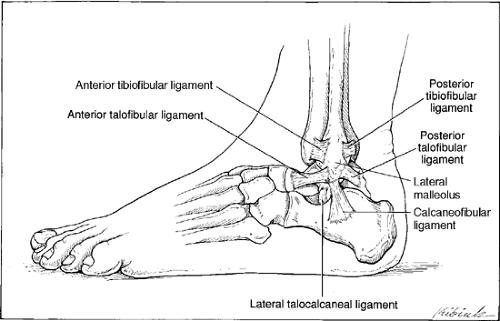
Descriptive Anatomy
The lateral malleolus is the protuberance at the distal end of the fibula. Attached to the malleolus are three clinically important ligaments:
Anterior talofibular ligament
Calcaneofibular ligament
Posterior talofibular ligament
These ligaments provide lateral support to the ankle, but they are not as strong as the deltoid ligament on the medial aspect (Fig. 15-8). These ligaments are prone to tears in inversion injuries.
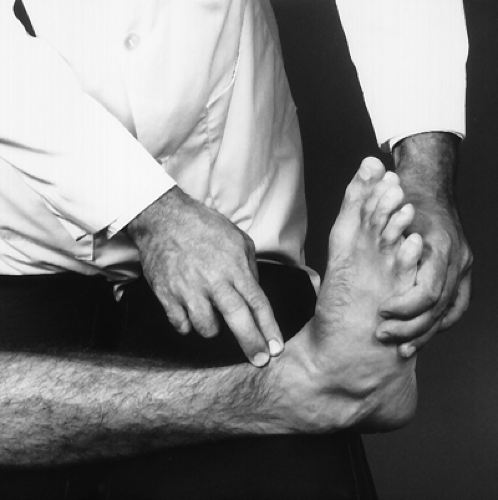
Procedure
Palpate the lateral malleolus with your index and middle fingers (Fig. 15-9). Note any tenderness and/or swelling. These signs may indicate periosteal contusion, fracture, avulsion fracture, or inversion sprain of any of the previously mentioned ligaments secondary to trauma.
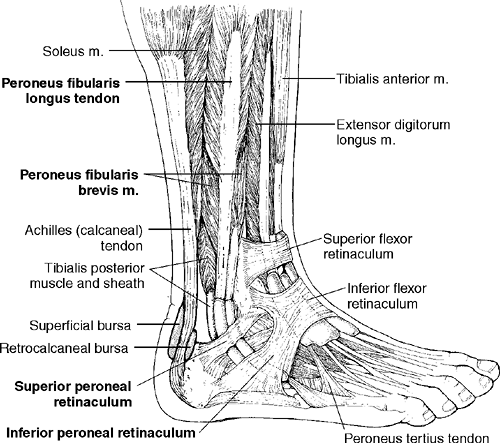
Descriptive Anatomy
The peroneus tendons travel together behind the lateral malleolus and are held in place by the peroneal retinaculum (Fig. 15-10). The action of the muscles are to plantar flex and evert the foot.
Procedure
With the patient not bearing weight, palpate behind the lateral malleolus with one hand, and passively invert (Fig. 15-11) and evert (Fig. 15-12) the foot with the other hand. Note any tenderness, swelling, or snapping. Tenderness and/or swelling may indicate tenosynovitis of either or both tendons. Tenderness with snapping may indicate a defect of the peroneal retinaculum that causes the peroneal tendons to subluxate or dislocate.
Anterior Aspect
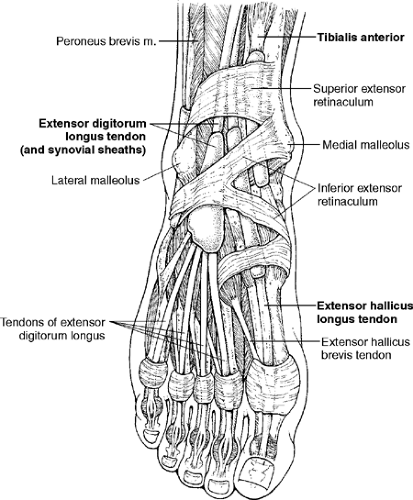
Descriptive Anatomy
The tibialis anterior tendon lies against the anterior surface of the tibia under the extensor retinaculum. It attaches to the medial cuneiform bone and first metatarsal (Fig. 15-13). Its action is to dorsiflex the ankle and invert the foot. The extensor hallucis longus tendon passes under the superior and inferior extensor retinacula. It inserts into the dorsal aspect of the great toe (Fig. 15-13). The action of the muscle is to dorsiflex the ankle and extend the great toe. The extensor digitorum longus tendon lies lateral to the tibialis anterior. It inserts into the middle and distal phalanges of the lateral four toes. It passes under the superior and inferior flexor retinacula (Fig. 15-13). Its action is to dorsiflex the ankle, evert the foot, and extend the lateral four toes.
Procedure
To palpate the tibialis anterior, instruct the patient to dorsiflex and invert the foot. The tendon should become prominent. Palpate the tendon for point tenderness (Fig. 15-14). Tenderness may be caused by overpronation, especially in runners. Tendinitis or a strain of the tendon also may be present. This muscle and tendon support the longitudinal arch of the foot.
To palpate the extensor hallucis longus tendon, instruct the patient to extend the great toe (Fig. 15-15). The tendon should be prominent. Palpate the tendon for point tenderness. This may indicate tendinitis or strain of the tendon.
To palpate the extensor digitorum longus tendon, instruct the patient to extend the toes. Palpate the tendon first where it crosses the ankle (Fig. 15-16), then when it divides into the four parts (Fig. 15-17) that insert into the middle phalanx. Tenderness may indicate tendonitis or tenosynovitis from overuse, especially in the runner.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree