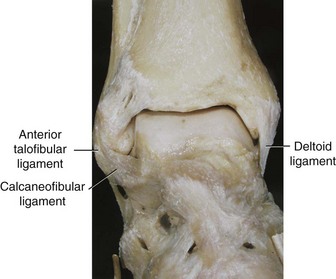
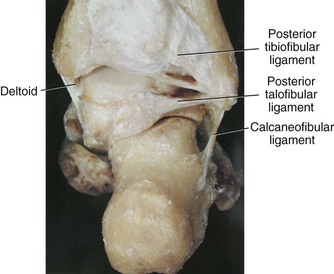
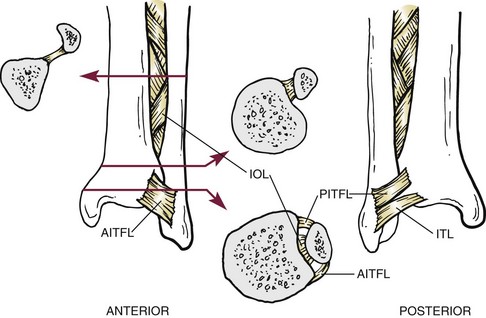
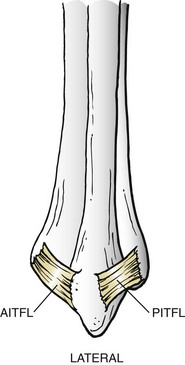
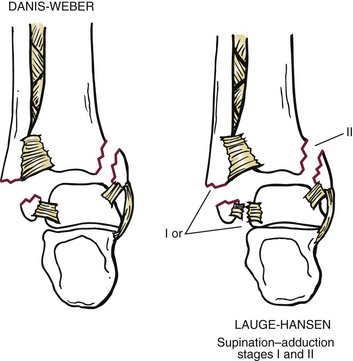
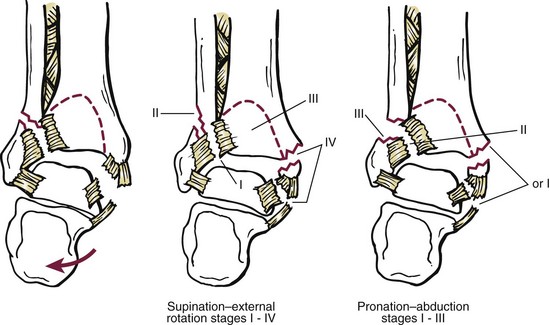
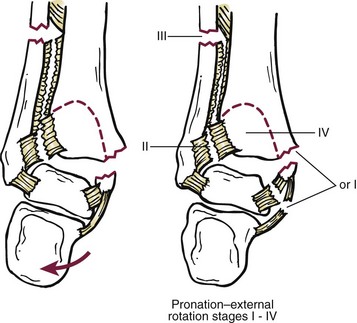
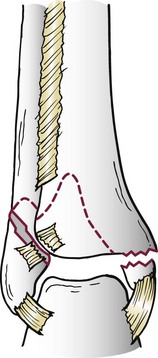
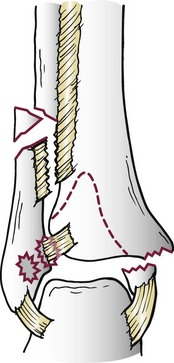
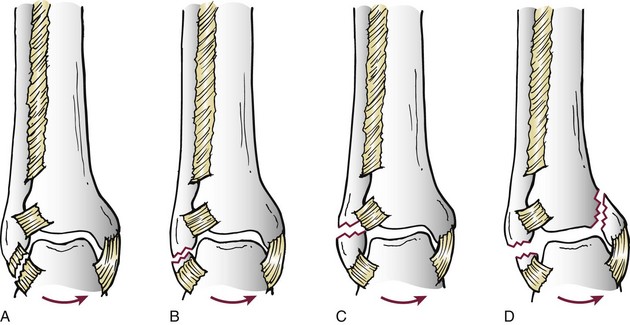
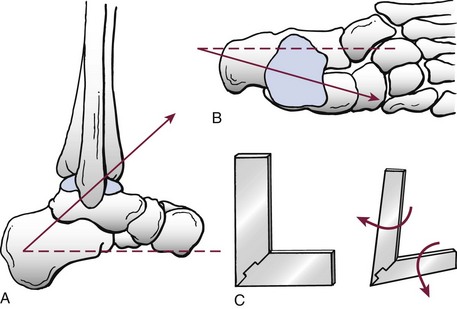
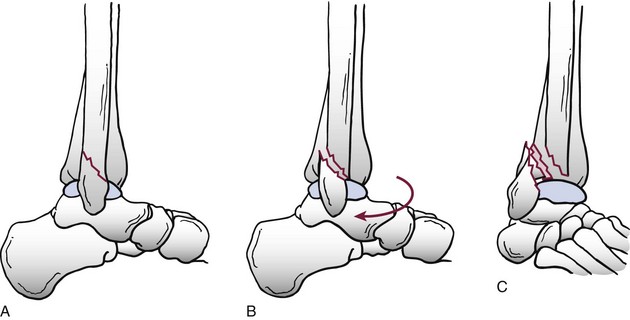
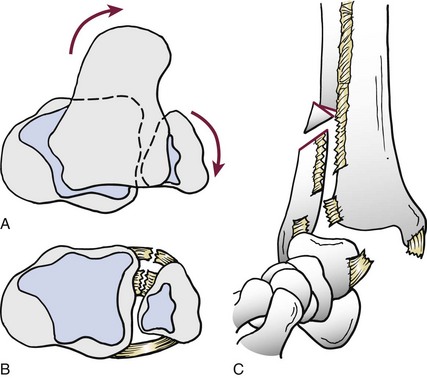
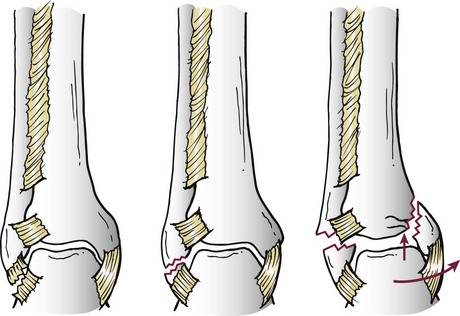
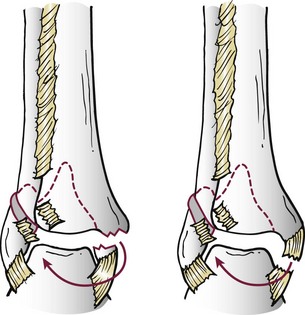
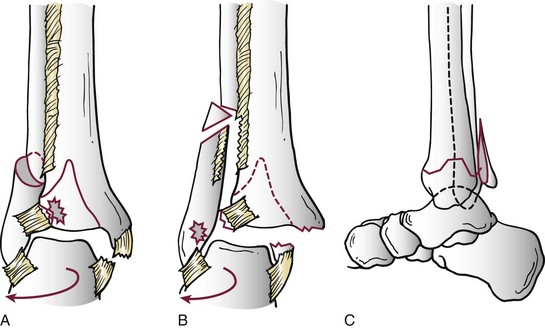
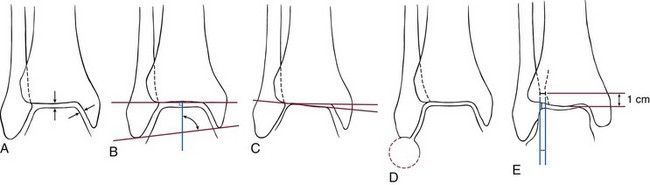
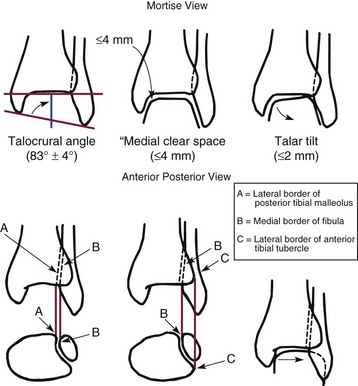
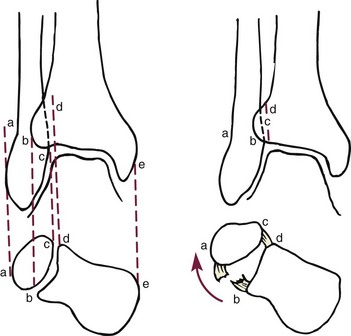
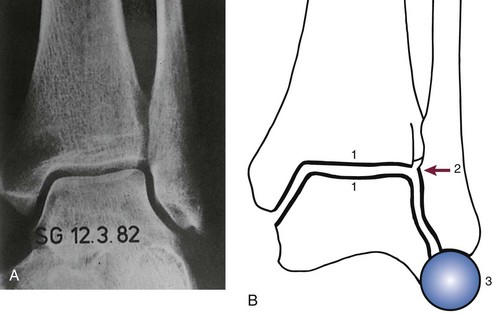
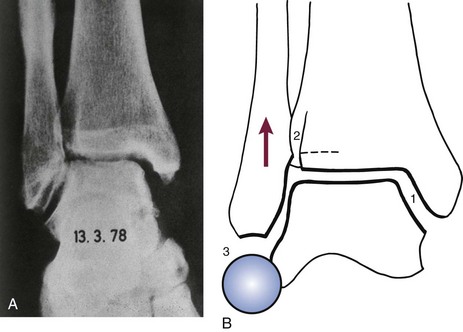
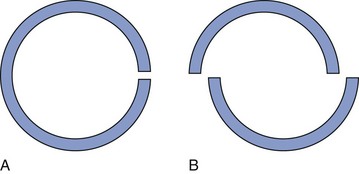
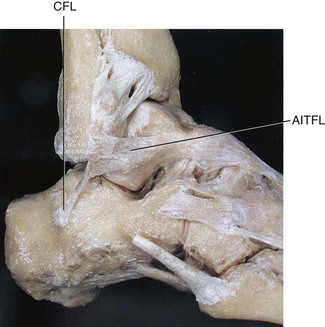
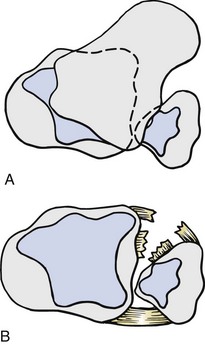
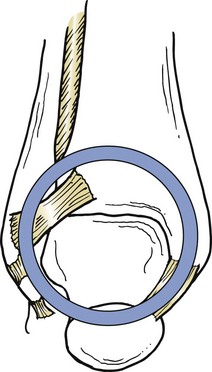
Chapter 37 The fractured ankle is the most common intraarticular fracture of a weight-bearing joint. Volumes have been written regarding ankle fracture, diagnosis, and treatment.31 Fractures of the ankle are routinely treated by most orthopaedic surgeons, and the available literature regarding the subject is abundant. Ankle fractures thus seem so ordinary that there is a certain amount of disregard for their seriousness. Attention to detail in their treatment remains critical if one wishes to avoid complications and obtain a satisfactory outcome. It was originally shown by Ramsey and Hamilton60 that malunion of the ankle leads to abnormal pressure distribution and arthritis. Thus the goals of treatment of fractures of the ankle are a congruent joint, fracture union, and the prevention of arthritis. A good outcome is likely if a congruent reduction, whether by closed or open means, can be obtained and maintained. The choice between performing an open procedure versus a closed reduction depends on whether the open treatment will provide superior results to closed treatment. The ankle is a modified hinge joint that does more than simply allow dorsiflexion and plantar flexion in the sagittal plane. The joint is much more complex, with coupled rotations occurring in both the axial and coronal planes.33 The ankle joint consists of three bones (tibia, fibula, and talus) and their connecting ligaments (deltoid, lateral ligament complex, and syndesmosis) (Fig. 37-1). The interaction of the joint surfaces of these bones is quite complex. The talus articulates with the tibia above and the calcaneus below, the navicular medially, and the fibula laterally. The dorsum of the talus mirrors the configuration of the tibial plafond, but it has two shallow crests rather than the single round dome that might be interpreted on radiographs.45 It also is wider anteriorly than posteriorly. The medial talar articular surface is curvilinear and comma shaped in its articulation with the medial malleolus. The talar articulation laterally with the lateral malleolus is more triangular in its configuration. These various articulations are held together by strong ligamentous support. The deltoid ligament provides medial support and is divided into two portions: superficial and deep (Fig. 37-2). The superficial portion extends from the tip of the medial malleolus and inserts broadly onto the navicular, sustentaculum tali (calcaneus), and the talus.20 The deep deltoid portion is a strong condensation of capsular fibers extending from the intercollicular notch of the medial malleolus to the medial talus. Functionally, the superficial deltoid resists hindfoot eversion, and the deep portion prevents external rotation of the talus. The deep portion also is the primary soft tissue restraint to medial opening. The lateral ligament complex is made up of three discrete components: the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL) (Fig. 37-3). These ligaments are neither as strong nor as bulky as their medial counterparts. The ATFL is a primary restraint to anterior displacement, internal rotation, and inversion of the talus. It is also the most frequently injured. The CFL is deep to the peroneal tendons and runs from the distal fibula to the posterior lateral tubercle of the calcaneus. It helps to stabilize the subtalar joint and is most susceptible to injury in extremes of inversion.10,16 The PTFL runs from the posterior aspect of the fibula to the posterior aspect of the talus (Fig. 37-4). Figure 37-3 Lateral anatomy of the ankle. AITFL, anterior inferior tibiofibular ligament; CFL, calcaneofibular ligament. The syndesmosis holds the distal ends of the tibia and fibula together. It is made up of four ligaments and the interosseous membrane (Figs. 37-5 and 37-6). Anteriorly is the anteroinferior tibiofibular ligament, which runs from the lateral surface of the tibia to the fibula and is quadrilateral. This ligament can be avulsed with its tibial attachment at the tubercle of Chaput, resulting in the Chaput fracture. Posteriorly, in a corresponding position between the tibia and fibula, is the smaller posteroinferior tibiofibular ligament. Nearly contiguous with the posteroinferior tibiofibular ligament is the inferior transverse ligament running from the posterior articular margin of the tibia to the fibula. These ligaments can avulse various-sized portions of the posterior malleolus of the tibia. A successful classification system should be able to offer treatment options based on the type of fracture, and provide the physician and patient a prognostic expectation.31,74 The two most commonly used classification systems are the Lauge-Hansen and Danis-Weber (Association for Osteosynthesis [AO] Müller) systems. The Lauge-Hansen36 system is based on the suspected injury mechanism. Fractures are categorized by a combination of foot position (supination or pronation) and direction of force (abduction, adduction, or eversion). Unfortunately, this complicated classification system has a steep learning curve and a high degree of interobserver unreliability.53,61 The Danis-Weber system75 is based on the level of the fibula fracture and is divided into three types. This system is easier to remember and has more relevance to operative decision making. These classification systems are different, but they are not mutually exclusive. Mast and Teipner41 first combined these in 1980. They pointed out that although the two systems do partially overlap, direct translation is not possible in all cases (Figs. 37-7 to 37-9). The most recent edition of AO Principles of Fracture Management62 uses a similar combination of the systems to describe the current AO Müller classification, which will be presented here (Figs. 37-10 to 37-12). The position of the foot and the direction of the deforming force dictate the pattern of failure of the osseoligamentous mortise. The position of the foot determines which structures are tight at the onset of the deformation and therefore most likely to fail first. If the foot is supinated (inverted), the lateral structures are tight and the medial structures are relaxed. By contrast, in pronation (eversion), the medial structures are tight and fail first. The deforming force can be rotational, usually external, or translational in abduction or adduction. The resulting specific fracture patterns of the lateral malleolus form the basis for the classification. With the foot supinated and an adduction deforming force applied to the talus, the first injury will occur on the lateral side, which is under tension. This can be rupture of the lateral ligament, osseoligamentous avulsion, or transverse fracture of the lateral malleolus at or just below the level of the tibial plafond. If the deforming force then continues, the talus tilts, and this causes a shearing compression fracture of the medial malleolus (Fig. 37-13). The commonest pattern of injury occurs with axial loading of a supinated foot. By virtue of the obliquity of the axis, about which subtalar movement occurs, inversion results in external rotation of the talus (Fig. 37-14). First the fibula fails, producing an oblique fracture. The fracture starts at the level of the ankle joint and extends proximally from anterior to posterior. Progressive talar external rotation causes posterior displacement, resulting in either an injury to the posterior syndesmotic ligament or fracture of the posterior malleolus. Finally, as the talus subluxates posteriorly, the medial complex fails either by a transverse fracture of the medial malleolus or by rupture of the deltoid ligament (Fig. 37-15). A third type of injury occurs when the foot is in pronation, the medial structures are under tension, and an external rotation force is applied (Fig. 37-16). The first injury occurs on the tensioned medial side in the form of a deltoid ligament rupture or a medial malleolar avulsion fracture. This allows the medial side of the talus to translate anteriorly. As the talus rotates externally, it forces the fibula to twist about its vertical axis, resulting in a rupture of the anterior syndesmotic ligament, followed by the interosseous ligament. At this point, the tibia dislocates medially off the rotating talus, forcing separation (diastasis) of the fibula from the tibia. This causes failure of the posterior syndesmotic ligament (or rarely, avulsion of the posterior malleolus), and finally an indirect fracture of the shaft of the fibula. The level of the fibular fracture depends on how far proximally the interosseous membrane rupture extends (Fig. 37-17). Figure 37-17 A, The fibula rotates and translates laterally. B, Rotation causes failure of the syndesmotic ligaments. A transverse fibular fracture below the level of the ankle joint implies an adduction injury with the syndesmotic ligament remaining intact (Fig. 37-18). With foot supination and talar external rotation, the fibular fracture is oblique and starts anteriorly at the level of the ankle joint, with possible partial disruption of the anterior syndesmotic complex (Fig. 37-19). The interosseous membrane, as a rule, remains intact. The posterior syndesmotic complex is either intact or detached in continuity with a fracture of the posterior lip (the Volkmann triangle). An indirect fibular shaft fracture, not extending below the syndesmotic ligaments, implies that both the medial and syndesmotic complexes have been disrupted and there is likely to be major instability (Fig. 37-20). The interosseous membrane, from the ankle joint proximally to at least the level of the fibula fracture, and the syndesmotic ligaments are ruptured through their substance or avulsed with their bony attachments. Although this is the common and potentially the more serious implication of this pattern, a suprasyndesmotic spiral fracture can occur from a purely external rotation of the fibula. This will disrupt only the anterior tibiofibular ligament, resulting in a more stable pattern as the fibula rotates externally on the intact interosseous membrane and posterior tibiofibular ligament. Radiographs of the ankle provide information regarding the mechanism of injury, the severity of the injury, the best approach to the injury, and the adequacy of treatment, be it surgical or nonsurgical. Attempts to determine when an ankle radiographic series should be performed in patients with acute ankle injuries have resulted in the publication of the Ottawa Ankle Rules.15,59 Under these guidelines, an ankle radiographic series is required only if the patient has pain in the malleolar zone and any one of the following findings: bone tenderness at the posterior edge or tip of the lateral malleolus, bone tenderness at the posterior edge or tip of the medial malleolus, or inability to bear weight both immediately and in the emergency department. Although the intent of these rules is to avoid the expense of unnecessary radiographs, the medicolegal climate in the United States would probably dictate that you “cannot treat what you cannot see” and to err on the side of caution. In short: If in doubt, obtain radiographs. Anteroposterior (AP), lateral, and mortise (an oblique view with the foot internally rotated 15 to 20 degrees) views are standard9,73 and allow evaluation of the integrity of the ankle mortise and of the tibiofibular syndesmosis. Criteria for displacement continue to evolve, but radiographic evaluation of the uninvolved extremity can serve as a valuable comparison for subtle displacement or instability. Radiographs should be evaluated for documented reduction criteria (Fig. 37-21). Of utmost significance is the medial clear space. Widening indicates talar translation or external rotation and loss of the integrity of the ankle mortise (Fig. 37-22).46 Permanent displacement of the medial clear space greater than 4 mm or narrower than 1 mm is associated with poor outcome.47,48 Talar shift of as little as 1 mm can result in a 42% reduction in talotibial contact area.60 Figure 37-22 Anteroposterior radiograph demonstrating lateral talar translation with medial clear space widening. The integrity of the syndesmosis is best assessed on the AP projection; however, measuring this remains difficult. Direct measurement of the syndesmosis width is taken 1 cm above the joint surface of the talus and is defined as the horizontal distance from the tibial incisura to the medial border of the fibula (Fig. 37-23).8,43 Complete disruptions, if undisplaced, can appear normal. The external rotatory malalignment that occurs when only the anterior tibiofibular ligament is torn is subtle (Fig. 37-24). The tibiofibular clear space (from the lateral border of the posterior tibial malleolus to the medial border of the fibula) might not change as the fibula rotates outward. This distance should be less than 5 mm. It is necessary to check the extent of overlap of the fibula by the anterior tibial tubercle. The tibiofibular overlap from the medial border of the fibula to the lateral border of the anterior tibial prominence should be less than 10 mm. The medial clear space can be widened by laxity of the syndesmotic ligament, which also produces a slight talar tilt. Despite continuity of the deltoid ligament, the medial clear space can increase 2 to 3 mm.14 Comparison views or even stress views with the ankle in external rotation may be needed. On the mortise view, the ankle articular spaces should appear symmetrical. The superior surface of the talus should be congruous with the tibial plafond, and the medial and lateral articular spaces should be equal and comparable to the superior surface. The subchondral bone that forms the Shenton line should be intact. There should also be a continuous curve between the lateral talus and the recessed tip of the distal fibula (Fig. 37-25).76 Disruption of this line and circle is usually the result of shortening and external rotation of the fibula (Fig. 37-26). An additional measurement is that of the talocrural angle. This is formed by a line perpendicular to the distal tibia articular surface and a line connecting the ends of the medial and lateral malleoli (see Figs. 37-21 and 37-23). This angle averages 83 ± 4 degrees, and there should be less than 2 degrees of variance from the contralateral ankle.63 A too-shallow angle suggests fibular shortening. Another useful marker for ankle alignment is talar tilt (see Figs. 37-21 and 37-23). A line is drawn across the talar dome in the AP view, and a second line is drawn perpendicular to it. A third line is drawn down the weight-bearing center of the tibia and through the angle formed by the intersection of the first two lines. More than 5 degrees of difference from the contralateral ankle is abnormal.17,47 On the mortise view, the talar tilt can be calculated by drawing a line across the tibial plafond and another across the top of the talus. A distance of more than 2 mm between these lines indicates an abnormal ankle.67 In addition to the standard radiographic views, a full-length view of the tibia and fibula may be needed to identify pronation external rotation injuries resulting in Maisonneuve fractures.38 CT scanning is also appropriate when indicated for more complex or comminuted fractures and is invaluable when assessing nonunions and malunions. Prolonged immobilization results in multiple undesirable sequelae, including muscle atrophy, myostatic contracture, decreased joint motion, proliferation of the connective tissues in the capsular structures, internal synovial adhesions, cartilaginous degeneration, and bone atrophy.54 Mobilization that is instituted as early as possible obviates or decreases these abnormal processes. The decision of whether an ankle fracture requires open reduction and internal fixation (ORIF) should be based on how best the normal anatomy can be restored and stability maintained.62 Conceptualizing the ankle joint as a ring, similar to the pelvis, is helpful in deciding which fractures are stable or unstable (Fig. 37-27).51 One fracture in the otherwise intact ring is stable. A second fracture or an additional ligamentous disruption (a fracture equivalent) is unstable and more likely to require surgical stabilization (Fig. 37-28). Figure 37-27 The ankle with ligament and bony stabilizers acts as an intact ring, similar to the pelvis. Because ankle mortise incongruity is poorly tolerated and leads to abnormal loads on the articular cartilage, classically, closed reductions have been deemed unsatisfactory if radiographs show a medial clear space greater than 2 mm or a displacement of the medial or lateral malleolus greater than 2 mm (Fig. 37-29).58 Radiographic criteria can be misleading because they are based on a two-dimensional static picture of a three-dimensional dynamic joint. When deciding whether or not to accept any displacement in an ankle fracture, it is important to remember the effects of even small displacement on ankle congruity. Yablon et al81 showed that the talus follows the lateral malleolus. Ramsey and Hamilton60 postulated that a 1-mm lateral shift of the talus in the mortise reduces the contact area of the ankle by 42%. Hartford et al29 demonstrated that there is a significant loss of tibiotalar contact with posterior malleolar fractures involving greater than 33% of the joint surface. Fitzpatrick et al,23 in a cadaver study with four fracture simulations, found no increased contact stresses near the articular incongruity but found that the remaining joint bore increased stress and that the center of stress shifts anteriorly, loading cartilage that normally sees little load. In contrast, in a group of 150 patients with displaced fractures of the ankle caused by external rotation and abduction forces treated with ORIF, and with an average follow-up of 3.5 years, DeSouza et al18 reported 90% satisfactory results could be obtained even if up to 2 mm of residual lateral displacement of the lateral and medial malleoli were present. Pereira et al57 demonstrated that there was not a significant effect on tibiotalar contact area after mortise widening from syndesmotic injury. Although there is no reason not to strive for anatomic alignment, the stringency of Ramsey and Hamilton does not seem justified. The aforementioned parameters of up to 2 mm of displacement of the malleoli and 1 to 2 degrees of talar tilt seem to be compatible with a satisfactory outcome.81 If the closed reduction is determined to be adequate, the patient may be treated with cast immobilization and frequent follow-up. The types of fractures that are often stable enough for nonoperative treatment are isolated infrasyndesmotic (type A) fractures of the distal fibula that do not involve the medial side and isolated nondisplaced transsyndesmotic (type B) fractures of the lateral malleolus that do not involve the medial side (Fig. 37-30). If closed reduction is inadequate, ORIF should be considered. Likewise, all displaced ankle injuries are likely to be unstable, and accurate anatomic reduction can usually only be obtained with ORIF.
Ankle Fractures
Anatomy
Classification
Type A: Infrasyndesmotic Injury
Type B: Transsyndesmotic Injury
Type C: Suprasyndesmotic Injury
Radiographic Evaluation

Treatment Concepts
Operative versus Nonoperative Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ankle Fractures