ANATOMY
The ankle joint is simply not a hinged joint that gives uniplanar motion, but the complex anatomy of the ankle joint permits triplanar motion (
1,
2). The talus rests within the framework of the distal tibia and fibula (
Fig. 109.1). The tibia and fibula are held together by the syndesmotic ligaments that comprise the anterior and posterior inferior tibiofibular ligaments, interosseous ligament, and the inferior transverse ligament. The syndesmotic ligaments permit the distal fibula to rotate approximately 12 degrees relative to the tibia (
3). The talar dome and distal tibial plafond create a congruent and stable articular joint that is able to withstand four times the body weight during the stance phase of gait. The talar dome is wider anteriorly than posteriorly and has a central indentation that separates two crests (
4). Posteriorly, the distal tibia has a shallow groove for the flexor hallucis longus tendon. The lateral surface of the tibia includes the fibular notch, which articulates with the fibula. Superior to the notch is the interosseous tibiofibular ligament. The tubercle at the anterior border of the fibular notch, tubercle of Tillaux-Chaput, and the posterior malleolus, at the posterior border of the fibular notch, assist to stabilize the posterior ankle joint (
5,
6,
7,
8,
9,
10 and
11). The posterior inferior tibiofibular ligament originates from the posterior tubercle laterally on the posterior tibial surface. The posterior inferior transverse ligament also originates from the posterior tubercle. Lateral talar rotation in the transverse plane may injure the posterior tubercle. Loading of a plantarflexed talus may cause fracture of the posterior malleolus (Volkmann fracture) due to excessive tension to the posterior ligaments (
5,
11,
12). The anterior inferior tibiofibular ligament starts 5 mm above the articular surface and descends obliquely between the tibia and fibula (
13). It proceeds anteriorly to the syndesmosis to the anterior aspect of the lateral malleolus and assists in stabilizing the hindfoot to the forefoot during push-off in gait (
14). The talus has medial and lateral articular surfaces that articulate with its respective malleoli.
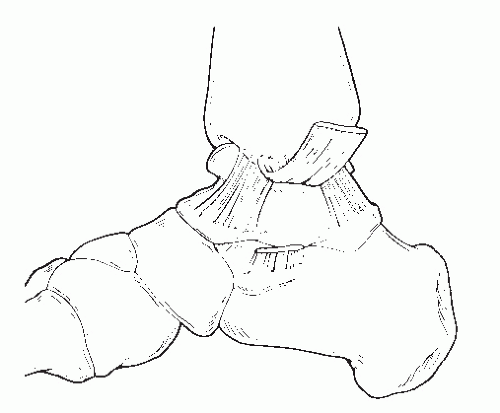
Medially, the distal tibia extends into the medial malleolus that consists of the anterior and posterior colliculi. The deep deltoid ligament originates in the intercollicular groove between the colliculi (
15,
16). The deep deltoid ligament has an intermediate and posterior component (
Fig. 109.2). The posterior component originates from the intercollicular groove and posterior colliculus. The deep deltoid ligament inserts just distal to the medial talar surface on the central and posterior aspects. The superficial deltoid originates from the anterior colliculus and attaches to the anterior talar neck, the navicular tuberosity, spring ligament, and the sustentaculum tali of the calcaneus (
16,
17 and
18). Talar external rotation is prevented by the deep deltoid ligament, and hindfoot eversion is prevented by the superficial deltoid ligament (
19). Excessive plantarflexion and eversion of the foot may cause rupture of the superficial deltoid at the anterior colliculus (
5,
17). Anterior colliculus fractures contribute 15% to 20% of medial malleolar ankle fractures (
20,
21,
22,
23 and
24). Similarly, excessive dorsiflexion stresses the posterior deep deltoid at the posterior colliculus. Fracture patterns may vary due to the deltoid ligament complex (
22,
23). Direct varus inversion of the ankle forces the talus against the medial malleolus, which may cause a vertical supracollicular fracture pattern (
25,
26,
27,
28 and
29).
The distal fibula includes the origin of the three lateral ankle ligaments. The medial surface of the distal fibula presents an articular facet placed anteriorly for the lateral surface of the body of the talus. Posterior to the articular fossa is the malleolar fossa, which is a rough depression for the origin of the posterior talofibular ligament and inferior transverse ligament. The anterior border of the lateral malleolus is the origin of the anterior talofibular and the calcaneofibular ligaments. The posterior border of the lateral malleolus presents a shallow groove, called lateral malleolus sulcus, which permits the passage of the peroneal tendons. The apex of the lateral malleolus is rounded and may contribute to the origin of the calcaneofibular ligament. The anterior talofibular ligament restricts foot anterior displacement, internal rotation, and talar inversion and is the weakest of the lateral ankle ligaments (
14,
30,
31 and
32). The calcaneofibular ligament, deep to the peroneal tendons, helps to stabilize the subtalar joint and restricts inversion (
30,
31,
32,
33 and
34). The posterior talofibular ligament restricts foot posterior displacement and is the strongest lateral ankle ligament (
32).
CLASSIFICATION SYSTEMS AND MECHANISM OF INJURY
Understanding the mechanism of injury allows physicians to categorize the fracture patterns, communicate the injury, evaluate the severity of the bone and soft tissue damage, and determine the treatment approach.
The mechanism of most ankle fractures is the result of the body weight and momentum compressing and rotating the tibia and fibula in relationship to the talus. The talus is fixed against the ground, while the tibia and fibula are moving to create the fracture dislocation. Vertical gravity, transverse movement, and the torsional force of the tibia and fibula against the fixed talus exceed the structural integrity of the ankle ligaments and bone. The description of these movements is very confusing in the literature. Some articles describe the movement of the tibia to the talus, and others describe the movement of the talus against the tibia. Most authors have presented the mechanism in terms of describing the motion of the talus with respect to the tibiofibular mortise. To quote William Hamilton in his book, Traumatic Disorders of the Ankle, “this custom will be observed in this text.”
The position of the ankle joint, the position of the knee, and the movement of the body determine the pathomechanics of the osseous and soft tissue damage. The combination of gravity, anterior movement, lateral movement, or posterior movement can predict the injury. A straight perpendicular gravity fall with the knee fully extended and locked will produce a vertebra compression fracture and a joint depression calcaneal fracture. An anterior movement with the knee fully extended will produce a tendo Achilles rupture or an anterior tibial axial compression or pilon fracture. A posterior movement will produce a hip fracture or low back injury. A forced ankle dorsiflexion movement with the knee flexed will produce a talar neck fracture. A lateral transverse fall will produce a supination or pronation subtalar joint dislocation. The focus of this chapter is the more common ankle malleolar fractures.
Two classifications have prevailed and are commonly used today. They provide insight into the diagnosis of occult soft tissue injuries. They are the Lauge-Hansen classification and the Danis-Weber classification.
Although not the first classification system to correlate ankle fractures to the mechanism of injury, Lauge-Hansen classification system has been widely accepted as the primary classification system in evaluating ankle fracture patterns (
35,
36,
37,
38,
39,
40,
41 and
42). The classification is simple; only four types accurately describe over 95% of all ankle fractures.
Lauge-Hansen fracture patterns and observations were made based on cadaveric models. Injuries were classified with a two-word description: first by the foot position (supination or pronation) and second by direction of the talus in relation to the tibia and fibula (abduction, adduction, or eversion). The original work was done in a laboratory setting. It is the rotation of the talus that supplies the forces necessary to injure the bony and ligamentous structures (
43). The classification system breaks down each fracture pattern into a sequential series of events based on the severity of injury (
44). Two basic concepts make this classification useful. First, a soft tissue injury and a bone injury cannot occur during the same stage. If there is tension on a ligament, either the ligament will tear or the ligament will remain intact and avulse a piece of bone, but both ligament and the bone cannot be damaged. Second, the injury cannot skip a stage. In the sequence of an injury, as each stage happens, either the ligament is torn or the bone is fractured. If the radiographs do not show a fracture, then the soft tissue injury must have occurred at that stage. These two concepts allow accurate evaluation of soft tissue damage based on radiographic evaluation and assist in the surgical decision making. There are four types of fibular fractures:
Transverse at or below the joint line
Short comminuted with a “butterfly” fragment at the joint line
Spiral at the joint line
High above the joint line
All of these are unique to the classification and sequence stage. These are called hallmark fractures. There are two types of tibial fractures: (a) vertical and (b) transverse. The vertical fracture is unique and a hallmark fracture. The transverse fracture is either an avulsion of the deltoid ligament or a “knock-off” fracture by the rotating talus and is common to three classification stages. Simply identifying these osseous hallmarks fractures on an x-ray will identify the exact mechanism and stage of accompanying soft tissue injury in both a Lauge-Hansen and Danis-Weber classification. The Lauge-Hansen classification identifies fibula fractures, tibia fractures, and ligament damage. The Danis-Weber classification identifies only fibular fractures and ligament damage. The hallmark fractures are underlined in
Table 109.1.
As such, the supination-adduction type refers to inverting the foot and ankle on a supinated foot. The pronation-abduction type refers to everting the foot and ankle on a pronated foot. The pronation-eversion type refers to internally rotating the leg on a pronated fixed foot. The supination-eversion type refers to internally rotating the leg on a supinated fixed foot.
Ankle dislocations and open fractures are commonly seen in the latter stages of these fracture patterns (
6,
45). Although this system illustrates the mechanism of injury and the method to reduce fracture dislocations, the reliability of the Lauge-Hansen classification system has been noted to vary on the observer (
41,
46,
47 and
48).
LAUGE-HANSEN CLASSIFICATION
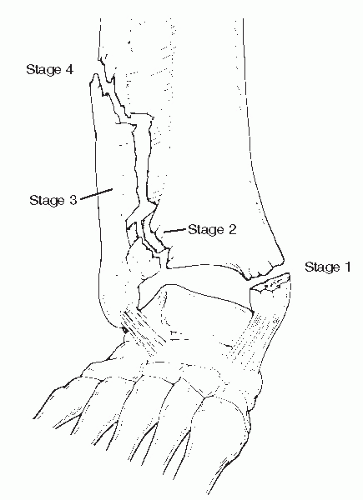
Supination-Adduction
The mechanism of injury is created by a frontal plane loading when the foot is supinated. The talus is inverted away from the lateral malleolus (
47). The lateral ankle ligaments can rupture or a transverse avulsion fracture of the lateral malleolus develops at or below the ankle joint (avulsion of the fibular styloid) (
38,
47,
49). If the fibula is fractured, the lateral ankle ligaments are intact and avulse the fibula. This is a hallmark fracture. An example would be a tennis player with lateral movement and an abrupt stop or a slight step off a curb with direct frontal plane inversion of the ankle with the body weight directing down. This is a stage 1 injury (
Fig. 109.3). If this stage is the ankle ligaments, the x-rays will be normal. A rupture of the anterior talofibular ligament, calcaneal fibular ligament, and posterior talofibular ligament is indeed an ankle fracture (SADD stage 1) injury.
In stage 2, the medial malleolus is impacted, which can cause a vertical fracture starting at the plafond with or without impaction (
50). This is a compression fracture as the talus moves medial and there is no strain or tension on the deltoid ligament. The deltoid ligament is intact. This is a hallmark fracture. Despite no radiographic evidence of a lateral malleolar fracture when a vertical medial malleolar fracture is present, it can be reasoned that the lateral ankle ligaments have been compromised (
38,
51,
52). This should be verified with stress testing for confirmation. The SADD injury has two hallmarks. The presence of a low transverse lateral malleolar fracture or a vertical medial malleolar fracture is pathognomonic for a supination-adduction type injury.
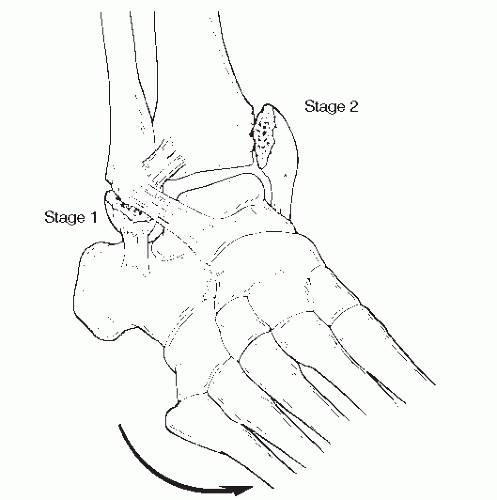
Pronation-Abduction
The pronation-abduction injury is created by a frontal plane loading of an everting talus when the foot is pronated (
38,
39,
53,
54). The talus moves away from the medial malleolus. The talar motion strains the deltoid ligament. The deltoid ligament may rupture or transfer the force to the medial malleolus, creating a transverse fracture at or below the ankle joint (stage 1). An example would be a snow skier with lateral movement and catching the inside edge of her ski or a slight step off a curb with direct frontal plane eversion of the ankle with the body weight directing down. See
Figure 109.4 for the sequence of events.
The continuation of the injury results in a partial or complete rupture or avulsion of the anterior inferior tibiofibular or posterior inferior tibiofibular ligaments (stage 2). There is a wide
variety of anatomic variations in the distal tibial fibular articulation and syndesmosis. If there is no actual cartilage articulation surface present, the interosseous ligament extends to the talus articulation. If there is an articulation surface, this cartilage can be damaged in this injury as an avulsion fracture line. The articular surface can extend as far as 2 cm proximal to the distal joint line seen on an x-ray. An avulsion of the anterior inferior tibial fibular ligament off the anterolateral tibia is called a Tillaux-Chaput fracture. An avulsion of the anterior inferior tibial fibular ligament off the anterior fibula is called a Wagstaffe fracture.
If the talus continues to rotate, the force is then transferred to the fibula (stage 3). A short oblique distal fibular fracture is sustained, commonly in a “butterfly”-shaped fragment. This is a hallmark. Because of the possible combinations of small bone avulsions, this fibular fracture is often comminuted and difficult to fixate.
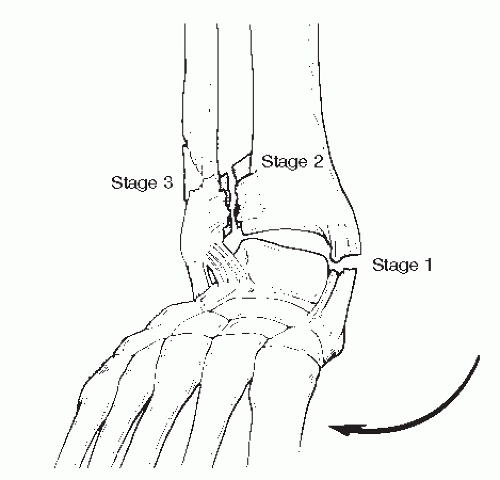
Supination-External Rotation
A supination-external rotation (SER) injury accounts for about 80% of ankle fractures. As the leg internally rotates on a supinated foot, the talus is again forced into rotation. There is a slight moment of dorsiflexion of the ankle and indeed patients relate the mechanism as “sitting or falling on their ankle.” This would describe the knee flexed, the ankle dorsiflexed, and the patient falling backward and sideways as the hip compresses onto the ankle. An example would be tipping on a curb or down an incline, the knee buckling and falling onto the ankle with all its weight. The initial leg rotation strains the anterior inferior tibiofibular ligament. As the talus rotates in stage 1, the anterior inferior tibiofibular ligament ruptures, avulses the anterolateral tibia (Tillaux-Chaput fracture), or avulses the anterior fibula (Wagstaffe fracture) (
38,
55).
Figure 109.5 illustrates the progression of this injury.
If the talus continues to rotate, the distal fibula is impacted, creating a distinct clean spiral oblique fracture starting anterior distal and progressing proximally and posteriorly (stage 2). This is the most common ankle fracture, a SER stage 2 injury. This is a hallmark.
Stage 3 occurs as the rotating talus then strains the posterior inferior tibiofibular ligament, resulting in rupture or avulsion of the posterior malleolus (Volkmann fracture) (
56). Variations of this mechanism may hinder closed reduction, necessitating open reduction (
57,
58 and
59).
In stage 4, the lateral talar rotation stresses the deltoid ligament. The deltoid ligament may rupture or the medial malleolus fractures transversely at the joint level (
60,
61). The presence of a medial clear space may not reliably indicate deltoid ligament integrity (
62). Fractures at this level are unstable.
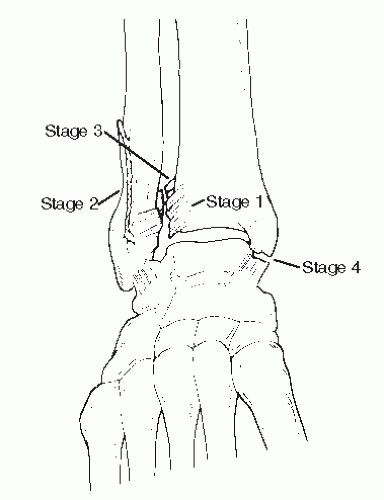
Pronation-External Rotation
As the leg is internally rotated on a pronated foot, the medial structures are strained first. The talus rotates and strains the deltoid ligament, resulting in a rupture or a transverse medial malleolar fracture (stage 1). There is a slight moment of plantarflexion of the ankle and indeed patients relate the mechanism as “twisting their ankle out.” This would describe the knee extended, the ankle plantarflexed with the foot out in front of the body as the patient moves forward. Typically, the foot contacts an immovable surface and the patient feels the ankle everting and rotation out of the mortise as the body fall forward. An example would be a baseball player sliding into second base with the knee extended and the foot forward, catching the base, or running and jumping forward with their foot against a fence to catch a ball.
Figure 109.6 illustrates the sequence of events in this mechanism.
The talus then stresses the anterior inferior tibiofibular ligament, which can either rupture or avulse from the tubercle of Tillaux-Chaput (stage 2).
Stage 3 injury patterns can be unique to this mechanism of injury. The talus rotates into the fibula, creating an oblique or
spiral fracture proximally. The fibular fracture typically starts in the distal shaft just proximal to the tibiofibular articulation (
54,
55,
60,
63). The interosseous membrane is ruptured from distal to proximal at the level of the fibular fracture (
38). Maisonneuve fractures are high fibular fractures near the fibular neck, which will necessitate tibial-fibular radiographs on suspected cases (
11,
54,
63,
64,
65 and
66). In rotational ankle fractures, a Maisonneuve fracture is pathognomonic for a pronation-external rotation (PER) mechanism of injury.
Stage 4 results as the posterior inferior tibiofibular ligament either ruptures or creates a posterior malleolar fracture (Volkmann fracture). Fractures at this stage are highly unstable.
The Danis-Weber classification system has been described as a “surgical classification” as a quick way to assess the fibular fracture (
51,
67,
68). This evaluation focuses on treatment plan for the fibular fracture and distal tibiofibular syndesmosis to restore ankle mortise stability (
Fig. 109.7).
DANIS-WEBER CLASSIFICATION
Type A Fracture
A Danis-Weber type A fracture is an avulsion of the distal tip of the fibula by an intact calcaneal fibular ligament. The fracture is transverse and is at or below the transverse joint line (
51,
52). The articular surface between the tibia and fibula and the syndesmosis is not injured. A type A fracture is a stage 1 Lauge-Hansen supination-adduction injury. In isolated conditions, this can typically be treated conservatively (
69). An additional vertical or oblique medial malleolar fracture is a stage 2 Lauge-Hansen supination-adduction injury and may require surgical reduction (
56,
70).
Type B Fracture
A Danis-Weber type B fracture is a short oblique or spiral oblique pattern beginning at articulation between the tibia and fibula (
51,
52,
63,
71). The articular surface can extend about 2 cm proximal to the transverse joint line. Most ankle fractures are type B patterns (
61,
72,
73 and
74). The anterior syndesmosis may be involved. Typically, the short oblique type B fractures are seen commonly with rupture of the anterior inferior tibiofibular ligament. Usually with short low oblique fractures, the anterior inferior tibiofibular ligament ruptures (
71,
72,
73,
74 and
75,
75,
76,
77,
78,
79,
80,
81,
82 and
83). There is greater variation of type B fracture patterns and can be seen with Lauge-Hansen pronation-abduction or SER (
40,
51,
52,
63,
75).