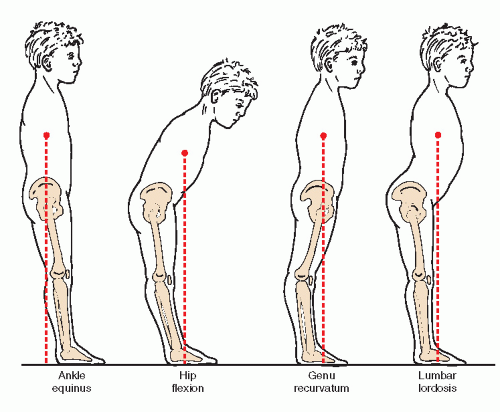
When an ankle joint equinus has been identified, its etiologic and associated compensatory pathologic features must then be determined. In the past, many authors offered their definitions and classifications of equinus along with their recommended corrective procedures. Until recently, however, few had attempted to break down the equinus deformity into specific forms and etiologic entities.
McGlamry and Kitting (
29), in 1973, classified and provided clinical definitions of five etiologic types of equinus foot: talipes equinus, osseous equinus, gastrocnemius-soleus equinus, metatarsal equinus, and forefoot equinus. Their definition encompassed more than ankle joint equinus because they described the equinus foot as “one which at rest drops below the dangling foot to leg angle. This excessive plantarflexion of the foot may occur at the ankle, but often occurs at the midtarsal joint or at the tarsometatarsal joint.” Obviously, this definition includes types of equinus occurring distal to the ankle joint.
Metatarsal equinus is a state of plantarflexion of the forefoot in relation to the rearfoot at the tarsometatarsal or Lisfranc joint.
Forefoot equinus is a plantarflexed attitude of the forefoot on the rearfoot at the midtarsal or Chopart joint. Both are examples of anterior cavus or equinus occurring in the foot and not in the ankle.
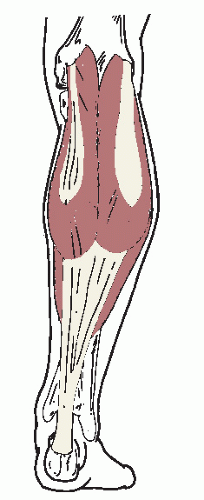
MUSCULAR FORMS
The posterior crural muscles individually, in part or as a whole, may be in a state of contracture and may thus produce an ankle equinus deformity. These contractures may be spastic or nonspastic (i.e., congenital, idiopathic, or acquired shortness).
Spastic equinus is the oldest known form of ankle joint equinus. It is usually found in patients with neuromuscular diseases such as cerebral palsy. The posterior crural musculature may be partially or wholly spastic and can overpower the weaker anterior musculature entirely. Hypertonicity of the involved musculature, hyperreflexia, and clonus are often found to be present. In this manner, pyramidal or corticospinal level spasticity may be differentiated from other motor disorders (
Table 43.2). In addition, efforts should be made to determine the muscle
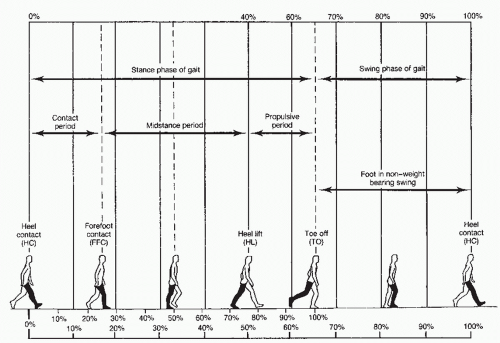
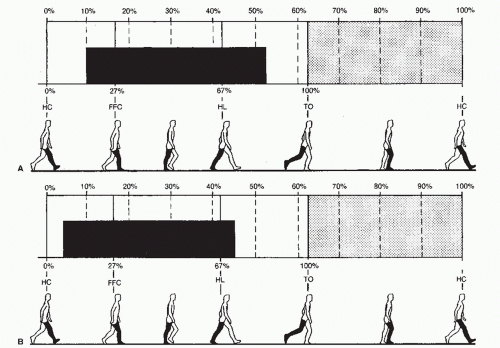
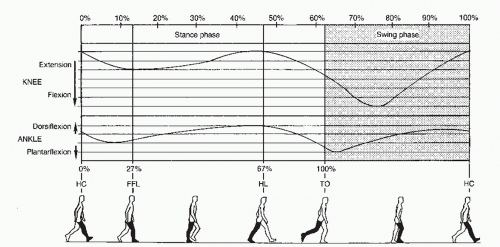
or muscles that are spastic inasmuch as this evaluation aids in proper treatment. As previously mentioned, in normal gait, the gastrocnemius and soleus muscles primarily function during the stance phase of the gait cycle. The anterior musculature, or dorsiflexors, are active mainly during the swing phase of the gait cycle. This, however, is not true in the presence of spastic equinus because the involved posterior crural musculature is spastic throughout the entire gait cycle. Depending on the degree of spasticity, the posterior group may overpower the anterior group. The gait is then no longer heel-toe but becomes toe-toe. This is the classic
toe walker, as described in the earliest literature. Lesser degrees of spasticity may allow the heel to come down or even contact the floor (toe-heel gait) (
31). Generally, the spastic forms of ankle equinus are more resistant to corrective treatment than are nonspastic forms.
Today,
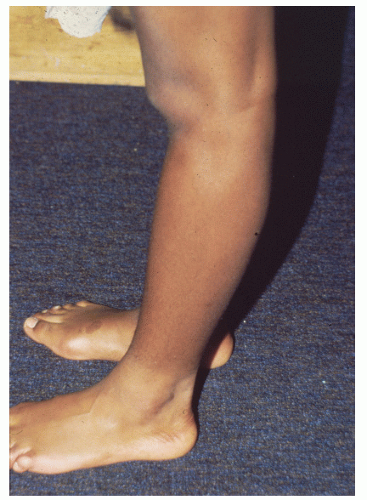
nonspastic muscular ankle equinus is discussed with increasing frequency and is now considered to be more common than spastic muscular ankle equinus. Congenital nonspastic shortness of the posterior crural musculature that creates an ankle equinus deformity was first reported by Hall et al (
6) in 1967. Toe walking may be considered normal when a child first begins to walk. However, within a 3- to 6-month period, or by age 7 years, the child should discontinue a toe-toe or toe-heel gait pattern and should learn to walk with a heel-toe gait. Children with a congenital shortness of the gastrocnemius or gastrocnemius-soleus complex may exhibit toe-toe gait but are able to lower their heels to the ground. The toe walking may be considered habitual when the child is capable of heel-toe gait, but prefers toe-toe or toe-heel gait. Occasionally, with examination or on surgical correction, an abnormally low insertion of the soleus muscle or an accessory soleus muscle may be identified (
32). Generally, however, no anomalies are identified, and results of the neurologic examination are completely normal. Thus, the diagnosis of congenital or idiopathic nonspastic ankle equinus is one of exclusion, in which the only abnormality is a limitation of ankle joint dorsiflexion (
33,
34,
35 and
36). In addition, several authors have described hereditary nonspastic gastrocnemius-soleus contractures as an autosomal dominant condition with variable severity of expression (
37,
38). More recently, Sobel et al (
39) analyzed 60 idiopathic toe walkers, and concluded that treatment should be initiated because fixed contractures may result with time.
In addition to congenital nonspastic shortness, acquired shortness of the posterior crural musculature creating an ankle equinus can result from nonspastic causes. Davis law states that “soft tissue under prolonged tension will elongate” and that the “same is true in retrospect.” Soft tissue contracts to its altered position, and this is the underlying etiologic factor in most cases of acquired muscular ankle equinus. Situations that create prolonged or repeated plantarflexed or equinus positions of the ankle may result in ankle equinus caused by muscular contracture. Common examples range from prolonged casting with the ankle joint plantarflexed to the repetitive use of highheeled shoes. Acquired shortness may also result from trauma (e.g., an Achilles tendon rupture with healing in a shortened position) or iatrogenic causes.
Although all or any portion of the posterior crural musculature may contribute to a muscular form of ankle equinus, gastrocnemius and gastrocnemius-soleus contractures are considered to be the most common. If a muscular ankle equinus deformity is suspected, the clinician must first determine whether the deformity is spastic or nonspastic by performing a complete neurologic history and physical examination. In patients with spasticity, studies have discussed the use of a tibial nerve block to help to differentiate the amount of fixed contracture from spastic contracture (
40,
41). These investigators measured the amount of torque about the ankle joint before and after the tibial nerve block. They theorized that the contracture present before the block was a result of both the spasticity and fixed contracture, and the contracture present after the block was the fixed contracture alone. This hypothesis may have future implications for the choice of surgical procedures or treatment to be performed.
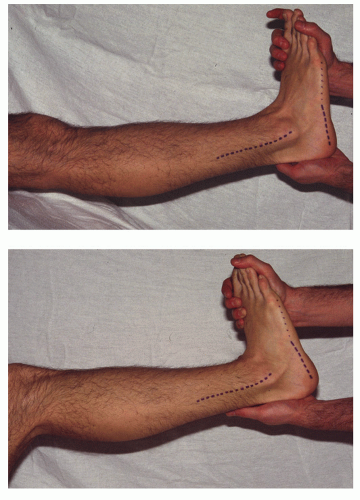
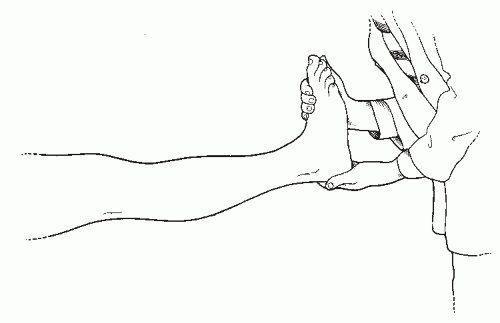
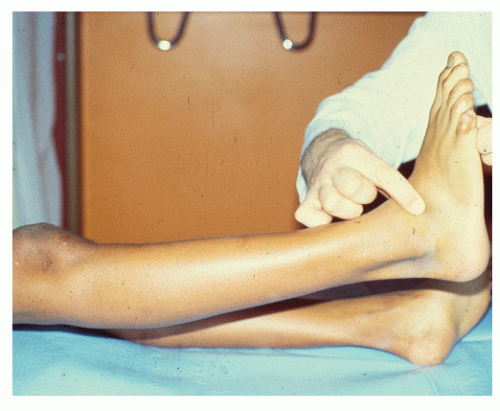
Once an assessment for the presence or absence of spasticity is completed, the examiner may evaluate the patient for the specific muscles involved. This later examination begins by confirming the presence of ankle or posterior equinus. With the patient lying flat and in a supine position, the leg is elevated slightly from the supporting surface with the knee maintained in an extended position (
Fig. 43.11). If genu recurvatum is found to be present, the measurement is made in that position, because that is the attitude in which the knee functions just before heel lift. The examiner then grasps the patient’s foot and maintains the subtalar joint in a neutral position (or a slightly supinated position, not pronated). Appropriate dorsiflexory pressure is then applied to the foot at the ankle joint, and the angle formed by the bisection of leg to the rearfoot in the sagittal plane is measured. If the amount of ankle joint dorsiflexion is less than 10 degrees (or greater than an 80-degree angle of foot to leg), a posterior or ankle equinus has been identified.
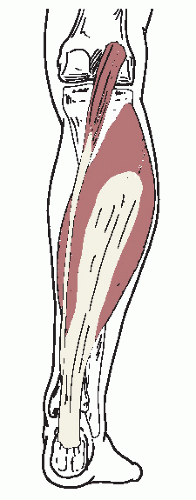
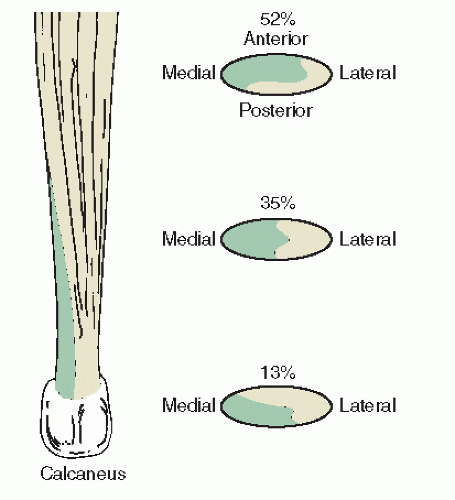
Gastrocnemius Equinus
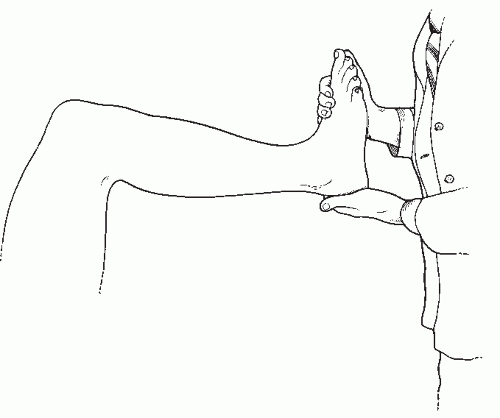
Gastrocnemius equinus is an etiologic type of ankle equinus caused by contracture or shortening of the gastrocnemius or plantaris muscles. Once a posterior or ankle equinus has been identified, the
Silfverskiold test may then be performed to differentiate gastrocnemius equinus from the remaining types of posterior equinus (
24). With the patient remaining flat and in the supine position, the examiner flexes the patient’s knee to a right angle and again dorsiflexes the patient’s ankle while making certain to maintain the subtalar joint in a neutral or slightly
supinated position (
Fig. 43.12). As before, a measurement of the sagittal plane angular relation of the bisection of the leg to the rearfoot is taken. If more than 10 degrees of ankle joint dorsiflexion (or less than an 80-degree angle of foot to leg) is found, a gastrocnemius equinus has been diagnosed. The gastrocnemius and plantaris muscles cross the knee joint, unlike the soleus muscle. When the knee is flexed, the courses of the gastrocnemius and plantaris are shortened, and the muscles are relaxed when the ankle joint is dorsiflexed. Conclusively, then, if there is a limitation of ankle joint dorsiflexion with the knee extended, but not with the knee flexed, the limitation can be attributed to tight gastrocnemius and plantaris muscles (
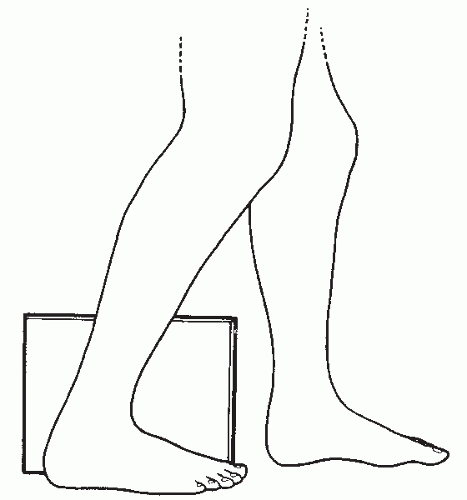
Fig. 43.13). If, after the Silfverskiold test is performed, a limitation of ankle joint dorsiflexion is still found to be present, other sources of ankle joint equinus must be present.
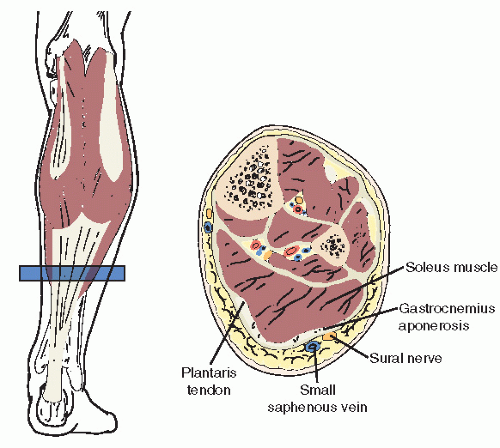
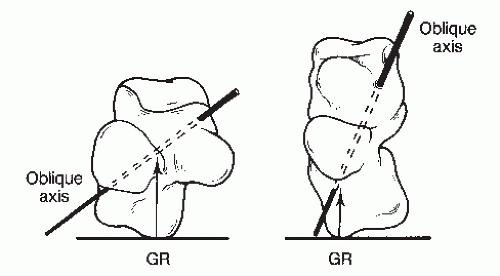
Gastrocnemius-Soleus (Gastrocsoleus) Equinus
Gastrocnemius-soleus (gastrocsoleus or gastrocsoleal) equinus is an etiologic type of ankle joint equinus caused by contracture or shortening of all or some of the soft tissue structures passing posterior to the ankle joint axis, including the components of the triceps surae. These sources may include any soft tissue structures that cross the ankle joint and not the knee joint. These structures, of course, must be capable of limiting ankle joint dorsiflexion and include the soleus muscle, the peroneal muscles (longus and brevis), the flexor longus muscles (digitorum and hallucis), the tibialis posterior muscle, and the ligamentous and capsular tissue of the ankle joint. Tightness and restriction by any of these structures may cause a limitation of ankle joint dorsiflexion with the knee in both the flexed and extended positions. Further, these conditions may cause a concurrent gastrocnemius (and plantaris) tightness. The tightness cannot be clinically isolated because of the limitation of ankle joint dorsiflexion with the knee flexed and extended and the
inconclusiveness of the Silfverskiold test. Consequently, most examiners assume that the gastrocnemius and plantaris muscles are tight when these other soft tissue structures are restrictive (
42). Gastrocsoleus equinus is the most common example of posterior equinus demonstrating a limitation of ankle joint dorsiflexion with the knee both flexed and extended. It must, however, be differentiated from osseous ankle equinus, which produces similar findings (
Fig. 43.14).
OSSEOUS FORMS
Osseous pathologic changes about the ankle may also limit ankle joint dorsiflexion and may cause an osseous form of ankle equinus. In addition, osseous equinus within the foot can cause the false appearance of an ankle joint equinus. This pseudoequinus is discussed and is differentiated as a form of osseous equinus.
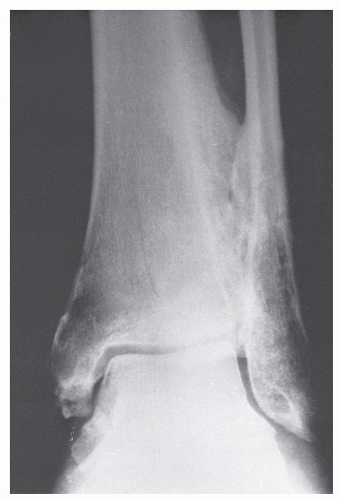
Talotibial Exostoses
Talotibial exostoses represent an etiologic type of ankle equinus and include any osseous projections from the margins of the trochlear surface of the talus and the distal articular surface of the tibia that could limit ankle joint dorsiflexion. Most commonly, these projections manifest as anterior talotibial exostoses that directly limit ankle joint dorsiflexion. However, posterior talotibial exostoses or, more rarely, other pathologic conditions about the ankle joint (e.g., osseous bridging between the tibia and fibula in the distal syndesmotic area) can also limit ankle joint dorsiflexion. This etiologic type of equinus demonstrates clinically limited ankle joint dorsiflexion with the knee both extended and flexed.
Although the range of ankle joint dorsiflexion is limited with both talotibial exostoses and gastrocsoleus equinus, the end range of dorsiflexory motion is soft or smooth in gastrocsoleus equinus and is hard or abrupt and firm in osseous ankle equinus caused by talotibial impingement. This observation is highly subjective, and considerable clinical experience is required to establish the correct diagnosis consistently without further evaluation.
Generally, additional evaluation is desired, and radiographs should be taken to eliminate the possibility that a bony blockage is associated with a talotibial exostosis. A conventional lateral radiograph of the ankle may be taken and examined for possible osseous projections from the margins of the trochlear surface of the talus or distal surface of the tibia that could limit the range of ankle joint dorsiflexion (
Fig. 43.15). In some instances, a tibial exostosis is seen along with a depression in the dorsal talar neck to accommodate the anterior tibial prominence. This has been described as the
divot sign, because the divot or depression occurs in the dorsal talar neck instead of a corresponding talar exostosis (
43). Additionally, synostoses may rarely occur between the tibia and fibula limiting ankle joint dorsiflexion. If this condition is suspected, a conventional mortise or medial oblique view of the ankle can be used to evaluate the distal tibiofibular articulation for any osseous pathologic changes (
Fig. 43.16). Further, a lateral weight-bearing radiograph of the ankle may be taken, with the patient instructed to bend the knee forward with as much force as possible (creating ankle joint dorsiflexion) while keeping the heel on the ground (
Fig. 43.17). This view, also referred to as a
charger view or
stress-dorsiflexion view, of the ankle may also be taken with the patient in a non-weight-bearing attitude. To obtain the view in a non-weight-bearing position, the examiner simply performs the aforementioned Silfverskiold test, and a lateral radiograph of the ankle is taken. Quantitatively, the sagittal plane angulation of the long axis of the tibia to the long axis of the talus is
measured in both the standard lateral and stress-dorsiflexion radiographs. If a limitation of ankle joint dorsiflexion is present in either view and a bony projection of tibia, talus, or other osseous structure is found to limit further dorsiflexion of the ankle joint, then a diagnosis of osseous ankle equinus can be made. If no apparent bony projections are present, a muscular gastrocsoleus ankle equinus with a tight triceps surae complex or associated posterior structures must be assumed (
8).
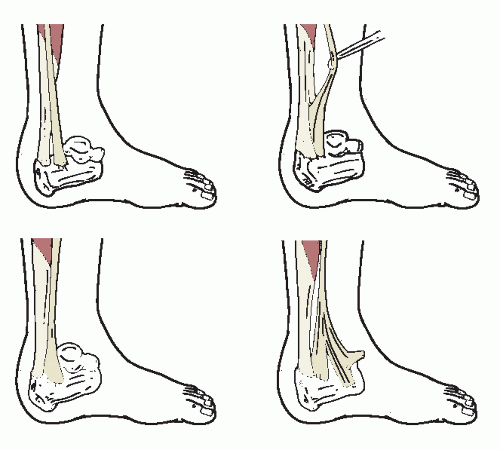
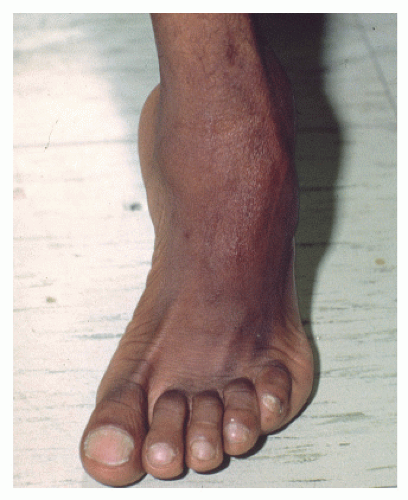
Pseudoequinus
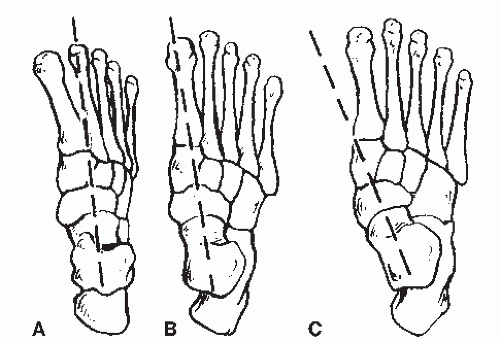
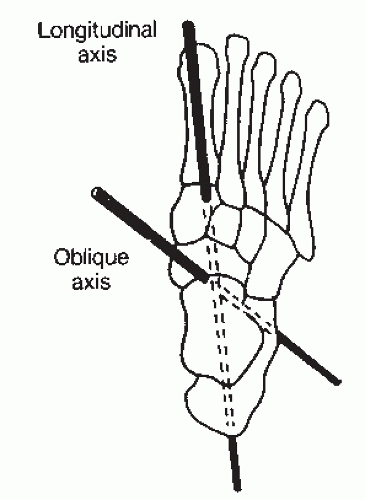
Anterior equinus, also known as anterior cavus, is a deformity represented by a plantarflexed attitude of the forefoot or any of its component parts. This type of equinus may be subdivided into four types based on the apex of the deformity in the sagittal plane. These types include the aforementioned metatarsal equinus and forefoot equinus along with lesser tarsal equinus (an excessive plantarflexed deformity occurring in the lesser tarsal bones themselves) or a combination of these deformities (
42). Although these types of anterior equinus do occur in the foot and not in the ankle, an apparent or false ankle equinus mistakenly can be measured clinically. To explain, ankle equinus is a sagittal plane measurement of the bisection of the leg to the rearfoot. The inexperienced clinician often falsely identifies an ankle equinus in the anterior cavus foot if he or she measures the sagittal plane bisection of the leg to the forefoot. This allows any plantarflexion of the forefoot on the rearfoot to be included in the measurement.
Identifying this problem and to avoid confusion, Whitney and Green (
42) appropriately coined the term
pseudoequinus to account for the false ankle equinus seen in an anterior cavus foot type as previously described. Thus, pseudoequinus is an angular relation of equinus of the forefoot to the leg in the sagittal plane without an equinus relation of the rearfoot to the leg in the sagittal plane. It is most commonly associated with a structural anterior equinus (i.e., anterior cavus) deformity. Pseudoequinus is not a true ankle joint limitation but an excessive demand for ankle dorsiflexion created by forefoot equinus. This occurs because the entire foot must be dorsiflexed at the ankle to allow the heel of the foot with anterior equinus to reach the ground. Thus, ankle joint dorsiflexion is overtaxed to compensate for the anterior equinus deformity (
42). Surgical correction of pseudoequinus is primarily by osseous correction to decrease the angular equinus relationship of the forefoot to the rearfoot (
Fig. 43.18). These surgical procedures are discussed elsewhere in this text.
COMBINATION FORMS
Perhaps one of the least understood forms of ankle equinus is that occurring as a combination of the aforementioned types. Unless the clinician is particularly attentive, these forms are often overlooked.
Pseudoequinus may occur in combination with any of the other forms of ankle equinus. If the examiner notes a sagittal plane equinus relation of both the rearfoot to the leg and the forefoot to the rearfoot, then such a relationship exists. Although this combined relationship is rare, it does occur, and one should not presume that the cavus foot cannot have an associated muscular or osseous ankle equinus. Once the cause of the anterior equinus is identified, the examiner may perform the tests used to differentiate the isolated ankle equinus deformities to determine whether the pseudoequinus is occurring in
combination with a muscular form of equinus (i.e., gastrocnemius or gastrocsoleus equinus) or a talotibial exostosis (
44).
Talotibial exostoses may also occur in combination with the other types of equinus. They can occur with a pseudoequinus. To determine an osseous equinus in combination with a gastrocnemius or gastrocsoleus equinus, one must first surgically resect the osseous block. Once the osseous block has been removed, the surgeon may then reevaluate the patient for muscular ankle equinus. If one finds 10 degrees of ankle joint dorsiflexion to be present with the knee fully extended, the osseous equinus may be assumed to be an isolated deformity. Often, however, the posterior musculature has adapted, and a gastrocnemius or gastrocsoleus equinus is discovered. Obviously, the Silfverskiold test can then be used to differentiate these muscular forms of ankle equinus (
44).
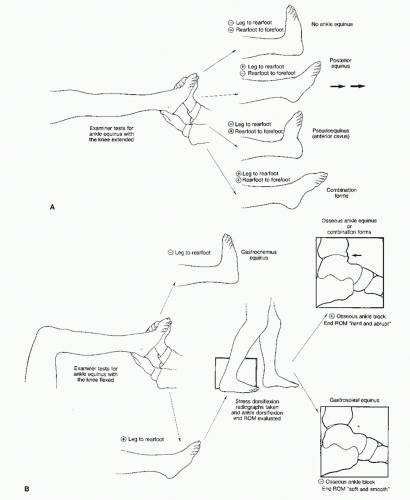
In summary, a stepwise approach can be used in the etiologic evaluation of ankle equinus (
Fig. 43.19). The clinician must be aware that equinus of the ankle often has more than one cause.