Ankle Arthrodesis with Onlay Graft
Vincent J. Sammarco
INTRODUCTION
Arthrodesis is a well-established method of relieving pain due to degenerative joint disease of the ankle. In the uncomplicated patient with little deformity, a standard open, mini-open, or arthroscopic technique can produce excellent results including pain relief, improved stability, and return of function. Some conditions may make successful arthrodesis more challenging. In the high-risk patient, the addition of an onlay fibular autograft can be utilized to increase stability and compensate for bone loss (1). It is possible to create the fibular onlay graft so that it remains vascularized through its periosteal blood supply. Utilizing a vascularized graft in this setting has the advantage in that the graft functions not only as a structural support but also adds a strut of living bone that bridges the fusion site. This has distinct advantages over free harvested autograft or allograft. This technique also spares the patient the morbidity of a second surgical site and potential complications from harvesting tricortical iliac crest autograft when structural graft is needed.
Patients with avascular bone due to trauma or systemic disease are at risk for nonunion due to the compromised biology of the fusion site. The addition of a fibular onlay graft in these patients can significantly improve the chances of success. Patients with diabetes often present with significant bone loss and deformity due to neuroarthropathy. A fibular onlay graft in patients with a neuroarthropathic ankle can usually be used not only for structural graft in the reconstruction but also to aid in the underlying biologic problems caused by the chronic glycosylation of tissue that typically accompanies Charcot disease. The technique is also useful in patients with underlying inflammatory arthropathy who usually have avascular, fibrotic, and osteoporotic bone due to chronic use of rheumatologic agents (2,3).
INDICATIONS AND CONTRAINDICATIONS
Indications
Degenerative ankle disease with bone loss due to erosive osteoarthritis, neuroarthropathy, or trauma
Avascular necrosis of the talar body and/or distal tibial metaphysis
Rheumatoid ankle disease with osteoporosis or requiring major deformity correction
Failed ankle fusion or conversion of ankle replacement to arthrodesis
Bridging of intercalated allograft or free autograft
Contraindications
The surgeon must balance the risks associated with increased surgical magnitude and surgical time with the risk of nonunion. The addition of the fibular onlay graft should be used selectively for cases that are at risk for nonunion with standard techniques and for salvage.
Active infection is a contraindication for internal fixation as described in this chapter, although this technique can be useful in achieving successful ankle arthrodesis in the presence of osteomyelitis when an external fixator is used for fixation.
PREOPERATIVE PLANNING
As this procedure is commonly done in patients with significant medical comorbidities and/or as revision surgery, a more thorough preoperative medical workup may be necessary.
Preoperative medical clearance should be obtained in patients with significant comorbidities.
Patients with diabetes mellitus should have adequate control of blood sugar to decrease the risks of infection and delayed healing.
The patient with rheumatoid arthritis deserves special attention. Consideration should be given to stopping or decreasing the use of nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, methotrexate, and other rheumatologic disease modifying agents (4). Cervical flexion and extension radiographs should be obtained if the patient is to be intubated as upper cervical instability is prevalent in these patients. Perioperative medical management with the patient’s rheumatologist is helpful.
In salvage cases and revision, it is important to establish the presence or absence of osteomyelitis preoperatively. Complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are helpful in determining whether infection is present. MRI can also be helpful, although chronic degenerative changes and neuroarthropathic bone can be difficult to differentiate from chronic osteomyelitis. MRI will be very nonspecific in this regard. We have found that nuclear imaging with technetium is particularly useful when combined with a labeled white blood cell scan in determining the presence or absence of osteomyelitis.
Anesthesia may be regional, general, or both. We typically use a popliteal and saphenous nerve block applied preoperatively in the patient holding area to aid in postoperative pain control. If the regional anesthetic is successful, this procedure can be done as an outpatient in otherwise healthy individuals.
Preoperative weight-bearing x-rays of the ankle and foot are obtained to delineate deformity and to document the condition of surrounding joints (Fig. 37.1).
SURGICAL TECHNIQUE
The patient is positioned supine on the operating table. We use a “bean bag” patient positioner to create a bump under the operative pelvis and position the leg with the neutral axis of the knee and tibial crest perpendicular to the floor. This is helpful in determining final alignment. A pneumatic
tourniquet is used around the thigh for hemostasis and is applied prior to prepping the extremity. The leg is prepped and draped with the knee exposed in the operative field. This is important for final positioning of the arthrodesis. We prefer covering the digits with an adhesive drape to minimize the possibility of contamination from the nails.
tourniquet is used around the thigh for hemostasis and is applied prior to prepping the extremity. The leg is prepped and draped with the knee exposed in the operative field. This is important for final positioning of the arthrodesis. We prefer covering the digits with an adhesive drape to minimize the possibility of contamination from the nails.
Anteromedial Approach: Joint Preparation
Skin incisions must respect previous surgical scars. We prefer an anteromedial exposure for preparation of the medial gutter and tibiotalar joint (Fig. 37.2). A separate lateral incision is used for preparation of the fibular onlay graft, which prevents undue tension on the soft tissue envelope and allows preparation of the tibiofibular syndesmosis and the lateral facet of the ankle. Often patients will have previous medial and lateral incisions from operative fracture treatment. In this case, the previous medial and lateral incisions will be used to expose the ankle mortise.
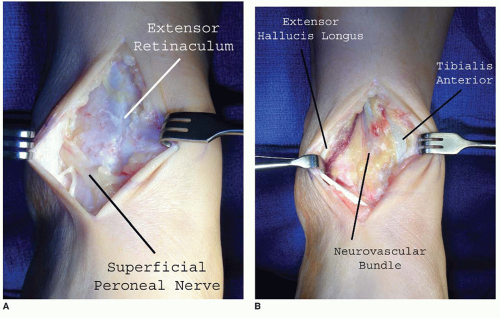
The anteromedial incision is made over the tibialis anterior tendon (Fig. 37.3). Care should be taken not to injure the superficial peroneal nerve laterally or the saphenous nerve medially, which may be identified in the subcutaneous tissue at this level. Careful preservation of the extensor retinaculum is important at this stage as repair of this structure is important during closure.
The superior extensor retinaculum is divided, and the interval between the tibialis anterior and extensor hallucis longus tendon is indentified. The deep peroneal nerve and anterior tibial artery are identified and retracted laterally with the extensor hallucis longus and extensor digitorum communis tendons. Army-Navy retractors are used for exposure of the ankle capsule.
Blunt dissection is done to expose the anterior ankle capsule medially and laterally. In cases where previous surgery has been done, the anterior neurovascular bundle may adhere to the ankle capsule and must be preserved. The ankle capsule is incised, and a subperiosteal dissection is done over the anterior tibia and medial malleolus. Hohmann retractors may be placed around the medial and lateral malleoli at this point. Often the deltoid ligament is contracted, and sharp release from the medial malleolus and talus is necessary to allow distraction of the joint.
Aggressive resection of anterior and medial osteophytes from the tibia and talus are done at this point (Fig. 37.4A and B). Adequate anterior decompression is necessary to avoid positioning
the ankle in plantarflexion. A Cobb elevator is passed over the talar dome and used to free the posterior ankle capsule and to break adhesions. The joint is then distracted with a laminar spreader to facilitate exposure of the articular surfaces (Fig. 37.4C).
The arthrodesis bed is prepared by removing any remaining articular cartilage, fibrous tissue, and a thin layer of subchondral bone. We prefer hand preparation of the arthrodesis bed with a chisel and osteotomes. Once cartilage and eburnated bone are removed, the bed is feathered by cutting alternating vertical and horizontal cuts in the surface with a sharp 5-mm chisel to expose the deeper cancellous bone to the fusion bed. While this can be time-consuming, it avoids the potential thermal necrosis that can occur with the motorized preparation of hard and sclerotic bone. A burr may be used, but the wound must be continuously irrigated and care must be taken not to heat the tissue, or the biology of the fusion site can be compromised. We prefer to leave the curvature of the articular surfaces intact, which maximizes bone contact and makes final positioning easier.
Lateral Approach: Fibular Onlay Graft
A second incision is made over the fibula anteriorly (Fig. 37.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree