Ankle Arthrodesis
Norman S. Turner
Ankle arthrodesis is commonly performed on patients with end-stage ankle arthritis. A solid ankle arthrodesis can provide a patient with a durable, pain-free, functional extremity, which enables them to be productive with work and active in low-impact sports such as biking, swimming, or golfing. However, as the arthrodesis is extended to the adjacent joints, the functional limitations increase.
Patients with end-stage arthritis are often treated nonsurgically with activity modification, anti-inflammatory medicines if tolerated, and bracing prior to considering surgery. When these treatments do not provide adequate pain relief, then surgical treatment is indicated. Ankle replacements can also be performed on appropriate patients with end-stage ankle arthritis.
INDICATIONS
Posttraumatic arthritis and rheumatoid arthritis are the most common cause of arthritis in the ankle.
It can also be seen in patients who have had long-standing pigmented, villonodular synovitis, or synovial chondromatosis.
Patients who have cartilage loss as a sequela of radiation, infection, or failed reconstruction of their ankle will be candidates for an arthrodesis.
An arthrodesis can be used in attempted limb salvage for patients who require significant resection of the ankle joint and is not reconstructable with other options.
In patients undergoing extensive tumor resection and reconstruction with allograft, an arthrodesis may be used as a salvage procedure.
CONTRAINDICATIONS
Ankle arthrodesis is contraindications in patients with poor vascular supply to their lower extremity. These patients should undergo a vascular workup and reconstruction if appropriate prior to the arthrodesis.
Patients with poor soft tissue around the ankle are a relative contraindication for an ankle arthrodesis and may require soft tissue coverage.
Acute infection is a contraindication to arthrodesis. However, this may be treated with a debridement and antibiotics; then, a staged arthrodesis if there is extensive arthritis is warranted.
In patients with minimal arthritis, an arthrodesis is not indicated and nonsurgical treatment should be utilized.
Prior to surgery, a medical examination in the elderly patient is recommended to optimize healing potential. Also, an evaluation by physical therapy prior to surgery can be beneficial in determining the patient’s ability to be nonweight-bearing after surgery and may aid in determining if placement in a nursing facility will be needed.
PREOPERATIVE PREPARATION
The evaluation of the patient begins with a complete history and physical exam. Occasionally, the patient will have minimal pain with extensive radiographic changes so identification of the painful joint must be made. The soft tissues around the ankle are evaluated for previous incisions or soft tissue reconstructions. This may affect the exposure and may affect the type of fixation that is planned.
Imaging
The alignment of the ankle is closely evaluated with both physical and radiographic exams. Radiographic analysis begins with weight-bearing anteroposterior and lateral views, as well as a mortise view. This enables the surgeon to determine the bone quality, deformity, and bony defects. These views are essential for preparation for surgery. This will assist in determining the amount of bone that needs to be resected. It will also help in preparation if bony reconstruction requires bone graft from either the iliac crest or the allograft. If there is a mild deformity, frequently, this can be corrected through the arthrodesis site. However, if there is a severe deformity, it may require other procedures to balance the foot.
Exposure Options
The exposure for the arthrodesis can be determined by the deformity. If there is a mild deformity, you may be able to precede with either an arthroscopic or minimally invasive procedure where small incisions are used to débride the joint surface and then percutaneous fixation is placed. However, if there is a significant deformity of >10 degrees of varus or valgus, then a transfibular approach is frequently used.
Fusion Options
Preoperative planning is critical in determining what type of fixation will be needed. The goal of the surgery is to have broad congruent surfaces that are compressed and rigidly fixed in an optimal position in order to provide the best chance of solid fusion. The fixation options include internal compression screws, plate and screw fixation, or external fixator. Occasionally, an intramedullary rod can be used. However, this requires the fusion of the subtalar joint as well as the ankle joint. External fixators can be used especially in patients with history of infection or when there is poor bone quality or soft tissues. The advantage of internal fixation in patients receiving chemotherapy is that you do not have the risks of pin site infection in an immunocompromised individual.
Informed Consent
Preoperative counseling is important to prepare the patient for realistic expectations of what an ankle arthrodesis will provide. It provides significant pain improvement but does not give them a normal extremity. It is important that a patient understands the risk of infection, nonunion, adjacent joint arthritis, and neurovascular complications. Also, preoperative counseling should include a detailed description of the postoperative course so that the patient understands the length of immobilization as well as use of walking aids and prepares appropriately.
TECHNIQUE
Position and Draping
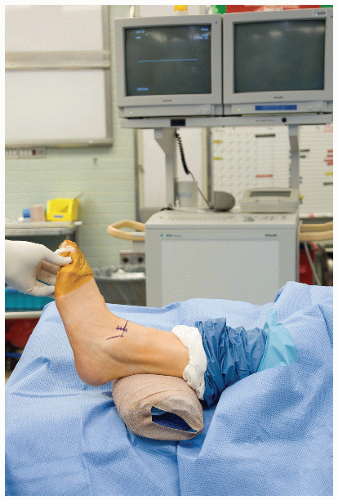
After general or spinal anesthetic, the patient is positioned on a radiolucent table in a supine position with a bump under the hip so that the foot is internally rotated and the toes are pointing toward the ceiling. A sterile tourniquet is placed on a thigh. The foot and ankle is prepped and draped in a standard fashion. The knee should be palpable. The patella and the tibial tubercle should be palpable in order to assist with positioning of the arthrodesis site (Fig. 24.1).
Incision and Exposure
If a minimal deformity is present, then a minimal exposure technique can be performed. In this technique, the foot is exsanguinated and the thigh tourniquet is inflated. A 2-cm incision is made just medial to the anterior tibial tendon with dissection through the skin and the subcutaneous tissue down the capsule (Figs. 24.2 and 24.3). The capsule is split longitudinally exposing the joint. A curved clamp can then be placed within the joint and palpated anterolaterally. An incision is made over the anterior lateral aspect of the ankle with dissection through the skin and the subcutaneous tissue. Careful dissection through the subcutaneous tissue is performed in order to identify and protect the superficial peroneal nerve branches. Dissection is then carried deep to the capsule (Fig. 24.4). The capsule incised longitudinally.
Through these two incisions, you have access to the ankle joint which is then prepared using osteotomes and curettes removing the remaining cartilage as well as the subchondral bone until cancellous-type bone is visualized. The joint surfaces are feathered with an osteotome to increase surface area. The contours of the surfaces are maintained to improve bony apposition. A laminar spreader placed within the joint from one incision enables you to have excellent visualization of the joint through the other incision and can assist with your preparation of the joint surfaces (Fig. 24.5).
After adequate preparation has been obtained, the foot is then positioned into neutral dorsiflexion, plantar flexion, slight external rotation, and 5 degrees of valgus. This can be held temporarily with a smooth Steinmann pin or can be held manually. Percutaneous large fragment cannulated screws are then placed. The alignment helps determine which screw is placed first. If the patient has a tendency toward varus, a lateral screw will be placed (Fig. 24.6). If the tendency is toward valgus, the medial screw will be placed first in order to optimize the alignment. Intraoperative imaging will verify the position, making sure the subtalar joint is not perforated, and then a partially threaded cannulated screw can be placed to obtain compression across the arthrodesis site (Fig. 24.7). A second pin is then placed percutaneously from the medial malleolus or the lateral tibial plafond into the talus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree