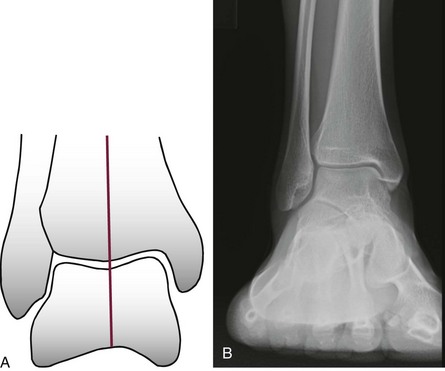
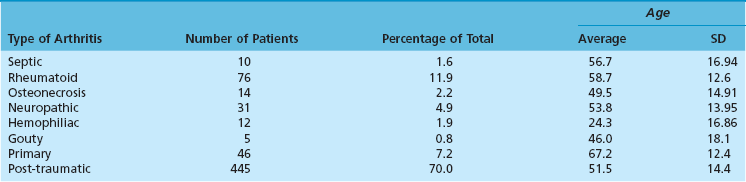
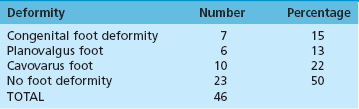
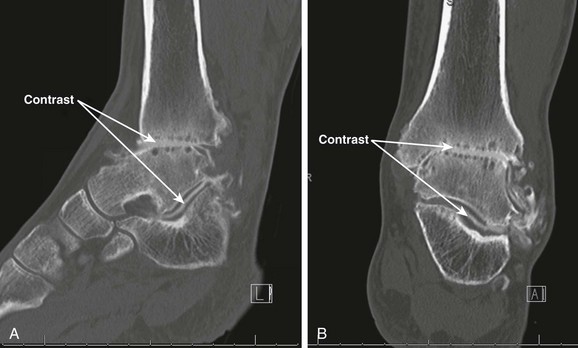
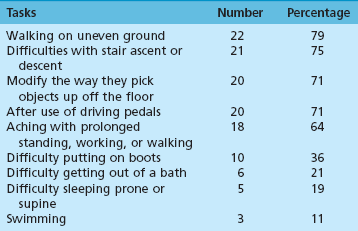
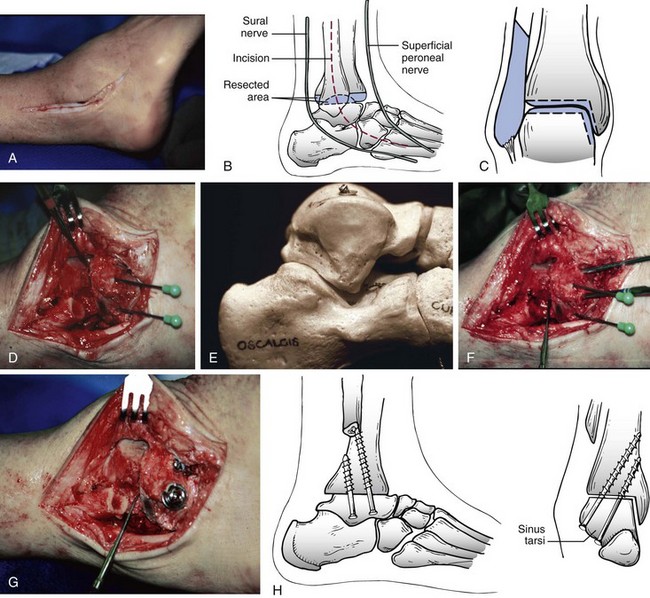
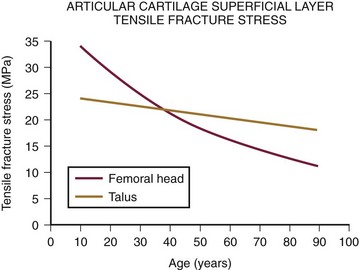
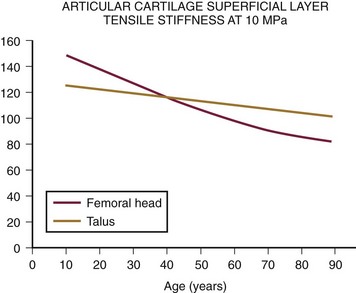
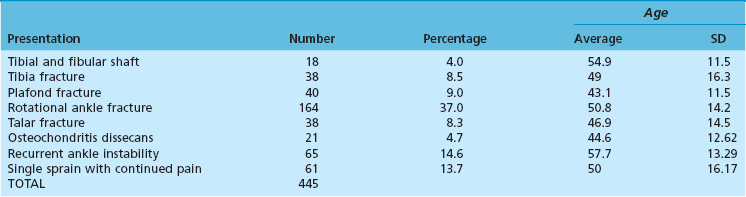
Chapter 21 UNIQUE CHARACTERISTICS OF THE ANKLE JOINT PREVALENCE OF ANKLE OSTEOARTHRITIS PATHOGENESIS OF ANKLE OSTEOARTHRITIS APPROACH TO THE PATIENT WITH ANKLE ARTHRITIS TREATMENT OF GLOBAL ANKLE ARTHRITIS In developed nations, physicians have noted a progressive increase in the incidence of disabling ankle arthritis, which may in part be due to the combined effects of the widespread use of life-protecting thoracoabdominal level airbag restraints and the general aging of the population.12 The increased incidence of painful posttraumatic ankle osteoarthritis has spurred interest in finding therapeutic solutions to this often disabling condition. The bony anatomy of the ankle joint determines the planes and ranges of joint motion and confers a high degree of stability and congruence when the joint is loaded. The three bones that form the ankle joint—the tibia, fibula, and talus—support three sets of opposing articular surfaces. The tibial medial malleolus and the medial facet of the talus form the medial articular surfaces, the fibular lateral malleolus and the talar lateral articular surface form the lateral articular surfaces, and the distal tibia and the superior dome of the talus form the central articular surfaces (Fig. 21-1). The distal tibial articular surface has a longitudinal convexity that matches a concavity on the surface of the talus. The center of matching convexity and concavity divides the tibiotalar articulation into the medial and lateral compartments for evaluation of ankle loading and degenerative changes (see Fig. 21-1). The distal tibia and the medial malleolus, together with the lateral malleolus, form the ankle mortise, which contains the talus. Firm anterior and posterior ligaments bind the distal tibia and fibula together to form the distal tibiofibular syndesmosis. Medial and lateral ligamentous complexes and the ankle joint capsule stabilize the relationship between the talus and the mortise. When loaded, the human ankle joint has a smaller area of contact between the opposing articular surfaces than the knee or hip. At 500 N of load, the contact area averages 350 mm2 for the ankle joint,7,57 compared with 1120 mm2 for the knee48 and 1100 mm2 for the hip.9 Although in vivo contact stress has not been measured in the ankle, the smaller contact area must make the normal peak contact stress higher in the ankle than in the knee or hip. Ankle joint articular cartilage differs from that of the knee and hip in thickness and tensile properties. The thickness of ankle articular cartilage ranges from less than 1 mm to slightly less than 2 mm.6 In contrast, some regions of articular cartilage in the hip or knee are more than 6 mm thick, and in most load-bearing areas, it is at least 3 mm thick.5 Work by Kempson54 shows that the tensile properties of ankle and hip articular cartilage differ and that these differences increase with age (Figs. 21-2 and 21-3). In particular, the tensile fracture stress and tensile stiffness of ankle articular cartilage deteriorate less rapidly with age than those of the hip.54 The tensile fracture stress of hip femoral articular cartilage is initially greater than that of talar articular cartilage. However, with age it declines exponentially in the hip but linearly in the ankle (see Fig. 21-2). As a result of these aging differences, ankle articular cartilage can withstand greater tensile loads than hip articular cartilage, beginning in middle age, and this difference increases with increasing age. Age-related changes in hip and ankle articular cartilage tensile stiffness follow a similar pattern (see Fig. 21-3). Figure 21-2 Femoral head and talus articular cartilage superficial layer tensile fracture stress versus age. Notice that the tensile fracture stress of ankle articular cartilage is greater beginning in middle age than the tensile fracture stress of femoral head articular cartilage and that the difference increases with increasing age. This illustration was developed from data reported by Kempson.54 (Graph courtesy Joseph A. Buckwalter, MD.) Figure 21-3 Femoral head and talus articular cartilage superficial layer tensile stiffness versus age. Notice that the tensile stiffness of ankle articular cartilage is greater beginning in middle age than the tensile fracture stress of femoral head articular cartilage and that the difference increases with increasing age. This illustration was developed from data reported by Kempson.54 MPa, megapascals. (Graph courtesy Joseph A. Buckwalter, MD.) Presumably, age-related declines in articular cartilage tensile properties result from progressive weakening of the collagen fibril network in articular cartilage. The cause of the age-related weakening of the articular cartilage matrix has not been explained, but age-related changes in collagen fibril structure and collagen cross-linking have been identified that might contribute to changes in matrix tensile properties.11,13 Kempson54 has suggested that these differences in tensile properties might explain the apparent vulnerability of the hip and knee to degenerative changes with increasing age and the relative resistance of the ankle to development of primary osteoarthritis. Ankle articular cartilage can differ from that of other joints in the expression of an enzyme that can degrade articular cartilage and in response to the catabolic cytokine interleukin-1 (IL-1). Chubinskaya and colleagues15 detected messenger ribonucleic acid (RNA) for neutrophil collagenase (matrix metalloproteinase-8 [MMP-8]) in chondrocytes of human knee articular cartilage but not in those of ankle articular cartilage. IL-1 inhibited proteoglycan synthesis by chondrocytes in knee articular cartilage more effectively than in those of ankle articular cartilage.47 The difference in the response to IL-1 between chondrocytes in knee and ankle articular cartilage appears to be due to a greater number of IL-1 receptors in the chondrocytes of knee articular cartilage. These observations need further study, but they suggest that metabolic differences exist between knee and ankle articular cartilage, which might help to explain the relative rarity of primary ankle osteoarthritis. Determining the prevalence of ankle osteoarthritis is more difficult than it might seem at first. As in other joints, the correlation between degenerative changes in the joint and the clinical syndrome of osteoarthritis is not consistent.28,106 In addition, it is extremely expensive and difficult to obtain and study unbiased samples of populations to determine the prevalence of osteoarthritis. For these reasons, studies of the prevalence of osteoarthritis by examination of autopsy specimens, evaluation of radiographs of populations of patients, and evaluation of patients presenting with symptomatic osteoarthritis have significant limitations. Meachim et al66–69 examined knee, shoulder, and ankle joints at autopsies performed on adults. They found full-thickness chondral defects in 1 of 20 ankle joints from people older than 70 years.66 Cartilage fibrillation was much more frequent than full-thickness defects in all joints. Huch et al47 resected 36 knees and 78 ankles from both limbs of 39 organ donors to evaluate the prevalence of ankle osteoarthritis. The joints were evaluated using a scale described by Collins.19 Grade 0 is normal gross appearance of a joint, grade 1 is fraying or fibrillation of the articular cartilage, grade 2 is fibrillation and fissuring of the cartilage and osteophytes, grade 3 is extensive fibrillation and fissuring with frequent osteophytes and 30% or less full-thickness chondral defects, and grade 4 is frequent osteophytes and greater than 30% full-thickness chondral defects. In these studies, grades 3 and 4 were defined as osteoarthritis, and grade 2 was defined as early osteoarthritis.47 However, the authors did not have information concerning possible symptoms associated with the joints studied, so it is not certain if the degenerative changes they identified were associated with clinical osteoarthritis. Using the Collins grading scale, Huch’s group found grade 3 and 4 degenerative changes in 5 of 78 (6%) ankle joints and in 9 of 36 (25%) knee joints (Fig. 21-4). Degenerative changes were most commonly found on the medial aspect of the ankle. Figure 21-4 Histogram showing the prevalence of ankle joint degeneration in autopsy studies reported by Huch and colleagues47 and Muehlman and colleagues.54 In these studies, the criteria for joint degeneration (osteoarthritis) were extensive articular cartilage fibrillation, osteophytes, and regions of full-thickness cartilage loss (Collins grades 3 and 4). Notice that joint degeneration was more than three times as common in the knee as in the ankle and that the prevalence of joint degeneration in the knee and the ankle increased with age. (Histogram courtesy Joseph A. Buckwalter, MD.) In another series of investigations, Muehlman et al74 examined seven joints, including the knee and ankle of both lower legs in 50 cadavers. The cadavers studied ranged in age from 36 to 94 years, with a mean age of 76 years. Sixty-six percent of the knee joints had grade 3 and 4 degenerative changes compared with 18% of the ankle joints (see Fig. 21-4). Ninety-five percent of the knees had grade 2, 3, or 4 degenerative changes compared with 76% of the ankles. The authors also observed that the medial compartments of both the knees and the ankles were more commonly involved than the lateral compartments. Radiographs often showed no evidence of degenerative changes, although direct examination of the joints showed regions of full-thickness cartilage erosion. Overall, the autopsy studies demonstrate that advanced degenerative changes are at least three times more prevalent in the knee than in the ankle and that the prevalence of degenerative changes in both joints increases with increasing age (see Fig. 21-4). Although epidemiologic studies based on radiographic evaluations document a striking increase with increasing age in the prevalence of degenerative changes of all joints, including those of the foot and ankle, the reported studies have not focused on ankle osteoarthritis. Radiographic studies of ankle joint degeneration have important limitations because there is no strong correlation between formation of osteophytes and development of clinical osteoarthritis106 and because it is difficult to evaluate the thickness of ankle articular cartilage, particularly on radiographs that were not performed in a standardized fashion. Furthermore, ankle radiographs often do not show signs of joint degeneration even when the ankle joint has regions of full-thickness erosion of articular cartilage.74 Attempts to evaluate the prevalence of ankle degeneration and osteoarthritis by plain radiographs alone therefore have limited value. Very few studies of the prevalence of osteoarthritis have included patients with ankle osteoarthritis. The available information suggests that knee osteoarthritis is 8 to 10 times more common than ankle osteoarthritis.22,47 Yet the best currently available estimates suggest that knee replacements are performed more often than ankle replacements and ankle fusions combined. These observations, combined with the data from autopsy studies showing that advanced knee joint degeneration is about three to five times more common than advanced ankle joint degeneration, suggest that surgical procedures are performed less often for patients with advanced ankle osteoarthritis than for those with advanced osteoarthritis of the knee. Clinical experience and published reports of the treatment of ankle osteoarthritis indicate that primary ankle osteoarthritis is rare and that posttraumatic arthritis, which develops after ankle fractures or ligamentous injury, is the most common cause of ankle osteoarthritis.26,44,91,94,110 Over a 13-year period in the senior author’s practice, 445 of 639 patients (70%) with Kellgren-Lawrence grade 3 and 4 ankle arthritis were posttraumatic cases, and only 46 (7.2%) had primary arthritis (Table 21-1).91 The most common causes of posttraumatic arthritis were rotational ankle fractures (37%) and recurrent ankle instability (15%) (Table 21-2). Curiously, 61 patients in this group gave a history of a single major ankle sprain that never healed completely. Of the 46 patients who were classified as having primary ankle osteoarthritis, 23 (59%) had clinically significant hindfoot malalignment, which emphasizes the intrinsic resistance of the ankle joint to primary articular degeneration and the relative rarity of primary osteoarthritis of the ankle (Table 21-3). Table 21-2 Posttraumatic Ankle Arthritis Patients in the Senior Author’s Practice over a 13-Year Period In a similar study, Valderrabano et al105 reviewed the etiology of symptomatic end-stage ankle arthritis for patients presenting to their clinic over a 10-year period. The results of their study were similar to ours in that they also showed that posttraumatic arthritis was the most common cause of end-stage ankle arthritis (78%). These authors also found that malleolar ankle fractures were the most common cause of posttraumatic arthritis (39%), followed by ligamentous injuries (16%) and pilon fractures (14%). Arthritis secondary to other causes was present in 13% of patients, whereas primary osteoarthritis occurred in only 9% of patients.105 The significant impact of knee and hip arthritis on patient function is well documented, and recent attempts have been made to better quantify the impact ankle arthritis has on the lives of patients. Several studies have established a baseline for the functional limitations on patients with end-stage arthritis of the ankle.2,39,98 Using different measures, all of these studies have shown that ankle arthritis severely impacts the lives of patients. Glazebrook et al39 used the Short Form-36 (SF-36) to prospectively compare patients with end-stage ankle to patients with end-stage hip arthritis. These authors showed that patients with ankle arthritis had SF-36 scores equivalent in severity to patients with end-stage hip arthritis and were two standard deviations below normal patients. Similarly, using the Musculoskeletal Functional Assessment (MFA), Agel et al2 showed that patients with ankle arthritis scored three times worse than normal patients. In a more recent study, Segal et al98 correlated the SF-36 and MFA scores with gait kinematics and step count. These authors found that patients with ankle arthritis had reduced function based on SF-36 and MFA scores. In addition, patients showed reduced ankle motion, ankle plantar flexion moment, peak ankle power absorbed, and peak ankle power generated in the affected limb when compared with the normal contralateral limb. Plain radiographs should be taken with the patient standing whenever possible. At our center, we have a standard minimum series of radiographs taken for patients with ankle problems. These include standing ankle lateral, anteroposterior, mortise, and hindfoot alignment views.89 The hindfoot alignment view is particularly important in situations where the heel is in varus or valgus and the ankle has coronal plane tilting (Fig. 21-5). If we are considering any surgery distal to the tibiotalar joint, we also obtain standing views of the entire foot. Figure 21-5 A, The hindfoot alignment view is taken with the patient standing on a platform, with the toes pointed straight ahead at the film plate. B, The x-ray beam is directed toward the ankle in a posterior to anterior direction, tilted 20 degrees caudad. The film is placed near the toes, also tilted 20 degrees, oriented exactly perpendicular to the beam.89 A line passing down the central longitudinal axis of the tibia should bisect the calcaneus. Advances in computed tomography (CT) have revolutionized ankle imaging. The total time for scanning has been reduced to 2 to 5 minutes compared with an average capture time of 20 minutes for MRI. As a result, CT images are much less susceptible to motion artifacts. The 4- and 16-slice helical units now capture anisotropic, 1-mm57 voxel-based data sets that can be postprocessed to show two- or three-dimensional renderings of any feature of interest (e.g., bone, tendons, cartilage). Intraarticular injection of contrast material before scanning can be used to enhance the accurate visualization of ankle articular features (Fig. 21-6).32 Computed tomography also has the large advantage over MRI of being able to work in an environment near retained hardware. CT arthrograms to delineate if a patient is suffering from global or focal tibiotalar arthritis or evaluate the condition of the subtalar joint have become a common adjunct to plain radiography at our center. Selective injections are used to help identify the source of pain for patients who have clinical or radiographic findings that suggest more than one focal source of pain.55 Before the injection, the patient is asked to perform activities that cause pain in the ankle (e.g., walk on uneven ground, walk up or down stairs, run). Diagnostic injections are done under fluoroscopic control. Contrast dye is first instilled to confirm the exact location of the injection. This is followed by injecting a local anesthetic. If the pain is not reduced by at least 75%, we look for a second source. In a study of foot and ankle fusion patients, Khoury et al55 reported that the reduction in pain after an intraarticular injection correlated to the response from surgery. A judiciously timed injection of the joint with steroids can help a patient enjoy an important life event (wedding, vacation). We do not like to give repeated injections of steroids because of the catabolic risks to soft tissues. Recently, there has been an increased interest in the use of injectable viscosupplementation for the treatment of ankle arthritis.* Review of the studies related to this subject show a large incidence of industry support and need to be interpreted with an understanding that this might introduce bias. Studies have shown an improvement in Ankle Osteoarthritis and American Orthopaedic Foot and Ankle Society (AOFAS) scores with hyaluronic acid injection; however, this improvement was no greater than control saline injection.18,24,88 Although the benefit of viscosupplementation beyond placebo effect is still controversial, there does not appear to be any significant adverse events associated with the injections.99,100,109 The authors do not routinely use hyaluronic acid injections for the conservative treatment of ankle arthritis unless there is a contraindication or need to delay surgery. In these situations, viscosupplementation is considered as an alternative to repetitive corticosteroid injections. The standard nonoperative treatment for end-stage ankle arthritis is mechanical unloading. A cane can be very helpful. If patients accept the cosmetic and functional limitations of an ankle–foot orthosis (AFO), they often obtain partial pain relief. We like to use an AFO that can be molded to the contour of the posterior calf muscles. This permits some unloading of the ankle. The two designs that appear to work best are a leather ankle lacer with an imbedded polypropylene shell for structural support or a calf lacer AFO.92 The former fits in a shoe; the latter requires metal drop locks fixed to a single shoe (Fig. 21-7). Adding a solid ankle cushion heel (SACH) and a rocker sole can help by further limiting ankle motion. However, ankle fusion is not entirely without problems. First, tibiotalar bone-bridging after attempted fusion surgery is not completely reliable, and reported rates of initial fusion range from 60% to 100%.* Second, initial pain relief can be elusive if other causes of pain are present or revealed by ankle fusion. Third, functional limitations are common, even with clinically successful fusions (Table 21-4).75 Fourth, shoe modifications may be needed to improve the transition from heel strike and toe-off, including use of a SACH or a rocker-bottom sole. Finally, accelerated degeneration of other foot joints, especially the subtalar and talonavicular joints, can occur after ankle fusion.17 This degeneration, in turn, can lead to further bracing or fusion surgery and must be considered when contemplating an ankle arthrodesis for a young patient. The desired position of the arthrodesis is as follows: 1. Alignment of the normal and abnormal limb is assessed to evaluate the degree of deformity. This is done by aligning the patella parallel to the operating table and observing the degree of rotation of the foot in relation to a perpendicular line from the patella. In this way, the surgeon can determine the degree of internal or external rotation of both the normal and the abnormal extremity. The advantage of this measurement approach is that it is relatively easy to check the alignment of the arthrodesis site at surgery. 2. A thigh tourniquet is applied, and a sandbag is placed under the ipsilateral hip to enhance the visibility of the lateral side of the foot and ankle. 3. The skin incision begins approximately 10 cm proximal to the tip of the fibula, is carried down over the shaft of the fibula, and then swings gently distally another 10 cm toward the base of the fourth metatarsal. Although this incision extends between nerves, with the sural nerve passing posteriorly and the superficial peroneal nerve passing anteriorly, the surgeon must be aware of an anterior branch of the sural nerve that might pass through the plane of the incision (Fig. 21-8A and 4. The skin flaps are developed to create a full-thickness flap along the skeletal plane. The periosteum is stripped from the fibula anteriorly and posteriorly, and the incision is carried on distally to expose the posterior facet of the subtalar joint and the sinus tarsi. 5. The dissection is carried across the anterior aspect of the tibia and ankle joint. With a periosteal elevator, the surgeon strips soft tissue from the distal end of the tibia, ankle joint, and proximal talar neck and then medially to the medial malleolus. Care is taken not to dissect distally over the neck of the talus to protect the blood supply into the talus. 6. The fibula is osteotomized approximately 2 cm proximal to the level of the ankle joint and beveled to relieve the sharp prominence (Fig. 21-8B). The distal portion of the fibula is removed by sharp and blunt dissection to expose the lateral aspect of the tibia and ankle joint as well as the posterior facet of the subtalar joint. As this is carried out, the peroneal tendons are reflected posteriorly. 7. An incision is made through the deep fascia along the posterior aspect of the distal tibia, which was exposed by the removal of the fibula. A periosteal elevator is gently moved medially across the posterior aspect of the tibia and then distally toward the calcaneus. This strips the soft tissues from the posterior aspect of the tibia and ankle joint. 8. Malleable retractors are placed anteriorly and posteriorly around the distal end of the tibia, exposing the anterolateral aspect of the ankle joint. 9. The initial cut for the arthrodesis is made in the distal part of the tibia with a sagittal saw, using a short, wide blade, and the cut is completed with a deep, wide blade. This cut is made as perpendicular as possible to the long axis of the tibia, and as little bone as possible is removed from the dome of the ankle joint. This cut is brought across the ankle joint and stops just where the curve of the medial malleolus begins (Fig. 21-8C). 10. A 4-cm incision is made over the anteromedial aspect of the medial malleolus over the ankle joint and swung slightly inferior around the malleolus to obtain adequate exposure of the tip of the malleolus. 11. The soft tissue is stripped anteriorly and then posteromedially around the tip of the medial malleolus, with care being taken to do as little damage to the deltoid ligament structure as possible. 12. The lateral intraarticular aspect of the medial malleolus is made visible, and the surgeon can see that the cut made in the distal tibia has not been completed. Using a 10-mm osteotome, the surgeon cuts along the lateral aspect of the medial malleolus. The articular cartilage is removed while starting to free up the initial cut that was made from the lateral side. Cutting along the lateral aspect of the medial malleolus decreases the possibility of fracturing it when mobilizing the initial cut in the distal tibia. 13. The tibial fragment is freed medially by placing a broad osteotome into the osteotomy site and gently levering it distally to break any remaining attachment to the medial malleolus, then removing it. Removal of this fragment has been facilitated by stripping the periosteum posteriorly before the cut and then making the cuts along the lateral aspect of the medial malleolus through the medial approach. Occasionally, if significant deformity exists, the entire distal end of the tibia is removed. When this is done, the tibia fragment must be split and removed in two pieces to prevent damage to the neurovascular bundle along the posteromedial corner of the joint. 14. The foot is now placed into the desired alignment in regard to dorsiflexion/plantar flexion and varus/valgus. The superior surface of the talar dome is identified through the lateral wound, and a cut removes 3 to 4 mm from the superior aspect of the talus. The cut must be made parallel to the one that has been made in the distal end of the tibia (Fig. 21-8C and D).
Ankle Arthritis
Unique Characteristics of the Ankle Joint
Anatomy and Motion
Articular Surface Contact Area
Articular Cartilage Thickness and Tensile Properties
Articular Cartilage Metabolism
Prevalence of Ankle Osteoarthritis
Autopsy Studies
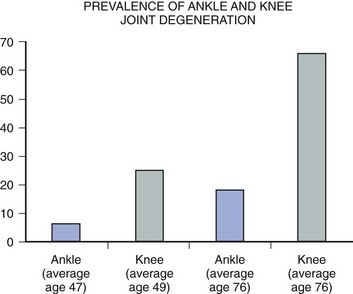
Radiographic Evaluations
Clinical Studies
Pathogenesis of Ankle Osteoarthritis
Impact of Ankle Arthritis
Approach to the Patient with Ankle Arthritis
Ankle Joint Imaging
Radiography

Computed Tomography
Selective Injections
Treatment of Global Ankle Arthritis
Conservative Treatment
Operative Treatment
Primary Ankle Fusion
Surgical Considerations
Open Ankle Arthrodesis
Position of Arthrodesis
 Dorsiflexion/plantar flexion: Neutral
Dorsiflexion/plantar flexion: Neutral
 Varus/valgus: 5 degrees of valgus
Varus/valgus: 5 degrees of valgus
 Rotation: Equal or slightly more externally rotated than the opposite extremity
Rotation: Equal or slightly more externally rotated than the opposite extremity
 Posterior displacement: Anterior aspect of the talar dome is brought to anterior aspect of tibia
Posterior displacement: Anterior aspect of the talar dome is brought to anterior aspect of tibia
Mann Technique
Preparation
Lateral Approach
![]() Video Clip 21).
Video Clip 21).
Medial Approach
Lateral Approach Revisited
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree