Anatomic Dissection of the First Metatarsophalangeal Joint for Hallux Valgus Surgery
John A. Ruch
Charles F. Peebles
Claire A. Sun
Repair of hallux valgus is a fundamental and time-honored area of foot surgery. Over the last 100 years, literally 100 or more different surgical procedures have been described for the correction of this basic foot deformity (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16). Each author has attempted to present a unique insight into the condition and to demonstrate a novel method of correction. Despite the multitude of techniques and procedures that have been promoted, one common denominator in the repair of hallux abducto valgus deformity remains: anatomy. The specific anatomy of the first metatarsophalangeal joint and these fundamental relationships provide a degree of commonality to all techniques and approaches for the surgical repair of the bunion deformity.
Although each patient must be evaluated individually, common elements contribute to the malalignment of the first metatarsophalangeal joint. A systematic dissection technique provides a method for assessment of the individual anatomic components of the first metatarsophalangeal joint and their contribution to the deformity of hallux abducto valgus. The technique of anatomic dissection provides a cornerstone for the intraoperative assessment and repair of the deformity.
RATIONALE
Although the term anatomic dissection is commonly accepted as a surgical philosophy for most podiatric surgeons, it actually encompasses all aspects of the surgical technique from incision placement to wound closure. The primary objectives of an anatomic approach in hallux valgus surgery include the surgeon’s ability to execute the procedure with control and consistency in the wide variety of anatomic variations encountered, to reduce complications, and to be able to identify and manage unique problems that may require special skills or techniques for a successful surgical repair.
An anatomic approach is employed in all key areas of the surgical technique:
Anatomic dissection
Incision placement
Tissue plane dissection
Preservation of blood and nerve supply, viability
Exposure
Individual anatomy assessment versus pathologic anatomy
Individual anatomic release and manipulation
Structural techniques, repair (osseous)
Muscle-tendon balance, soft tissue repair and periarticular balance
PRINCIPLES OF ANATOMIC DISSECTION
The underlying concept of anatomic dissection is the preservation of blood supply (and innervation) to the soft tissues during surgery. The incision placement is oriented parallel to and between any critical structures. The dissection of the subcutaneous tissues is the fundamental basis of anatomic dissection. The superficial soft tissues (those external to the deep fascia) must be reflected in a manner that preserves the skin and subcutaneous layers and avoids disruption of the laminar contact of these two layers and the linear structures they contain. This approach not only maintains the viability and healing potential of these tissues, but it also serves as the primary mechanism of establishing hemostasis of the surgical wound, whether the procedure is performed with or without a tourniquet. The primary control of bleeding both during and after the surgical procedure is most effectively accomplished with the anatomic dissection technique. This is key to reducing bleeding, hematoma, and edema. In addition to improved soft tissue healing, tissue plane dissection maintains a distinct separation of the superficial and deep tissues even after the healing process has occurred. Minimal scar and adhesion between the layers enhance delamination of tissue planes should revisional surgery become necessary.
Another critical function of the surgical dissection is exposure.
Whereas adequate exposure is usually related to the length of the incision, the exposure provided with anatomic dissection creates full visualization of all aspects of joint anatomy without excessive retraction or tension on the surrounding soft tissues. The “universal” dorsal medial incision allows for direct visualization of both medial and lateral aspects of the joint and their related components without the need for excessive retraction or a second incision.
Whereas adequate exposure is usually related to the length of the incision, the exposure provided with anatomic dissection creates full visualization of all aspects of joint anatomy without excessive retraction or tension on the surrounding soft tissues. The “universal” dorsal medial incision allows for direct visualization of both medial and lateral aspects of the joint and their related components without the need for excessive retraction or a second incision.
Full surgical exposure allows for critical evaluation of normal as well as pathologic anatomy around the first metatarsophalangeal joint. Direct visualization of the key anatomic components of the joint, especially within the intermetatarsal space, allows the surgeon to assess the structures influencing joint motion and facilitates the release, resection, or other manipulations of each of these structures.
The initial goals of the anatomic dissection process are to provide access to the surgical area, to establish hemostasis, to identify and release any significant soft tissue contracture, and to prepare for the “osseous” aspect of the surgical process. Once the structural aspect of hallux valgus repair has been performed, the procedure is completed with a repair and balancing of the periarticular soft tissue components. This includes refined capsulorrhaphy and tendon transfer techniques performed to establish a balance of function around the first metatarsophalangeal joint axis. This final repair process and the osseous realignment of the first ray are the keys to a successful and long-lasting surgical result.
PERIOPERATIVE ANESTHESIA
Before the actual incision, the perioperative area may be infiltrated with a local anesthetic agent. Hemostasis may be achieved without the use of a tourniquet by the addition of epinephrine to the solution. A common technique is to combine a short-acting and long-acting local anesthetic, usually equal volumes of lidocaine with epinephrine (1:100,000) and bupivacaine. This technique may be performed whether the patient is maintained under general anesthesia or with intravenous sedation. In addition to the augmentation of anesthesia, the epinephrine provides hemostasis through reduced capillary bleeding. Local infiltration of epinephrine-containing solutions has been shown to be safely used in combination with most modern general anesthetic techniques (17, 18, 19, 20, 21, 22, 23, 24, 25). This approach, along with the primary hemostasis established with anatomic dissection, allows the procedure to be performed without a tourniquet.
However, tourniquets represent an effective means of achieving hemostasis and are favored by many surgeons. Ankle, calf, and midthigh devices can be used safely when they are employed within commonly recognized guidelines (26, 27, 28, 29). Although complications may arise from the use of tourniquets, the incidence is low (30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43).
Complete anesthesia at the surgery site with the infiltration of local anesthetic also allows the patient to be maintained with a lower level of intravenous sedation or general anesthesia. This approach may reduce potential side effects from the narcotic and neuroleptic agents used in sedative and general anesthesia. Investigators have suggested that a preemptive effect may be obtained that would improve the patient’s postoperative course by decreasing pain (44,45).
INCISION
Strategic placement of the surgical incision can greatly enhance the surgeon’s ability to access adequately critical aspects or regions of the first metatarsophalangeal joint. Although the first metatarsophalangeal joint can be exposed through many different surgical approaches (46, 47, 48, 49, 50, 51, 52), a universal incision for hallux valgus surgery can be oriented along the dorsal medial aspect of the metatarsophalangeal joint and follows the angle of the primary deformity. The incision begins proximally about the midshaft level of the dorsal medial aspect of the metatarsal, extends distally to the dorsal medial aspect of the metatarsal head and ends just proximal to the hallux interphalangeal joint, medial to the extensor hallucis longus tendon. This primary incision should extend equidistant from the center of the metatarsal head to allow for ease of retraction in exposure of both the medial and lateral aspects of the metatarsophalangeal region. The incision usually lies between the extensor hallucis longus tendon and the dorsal medial neurovascular structures. The incision technique is usually controlled depth, to allow for separation of the dermis without violation of underlying subcutaneous vessels.
SUBCUTANEOUS DISSECTION
Manipulation of the subcutaneous layer is the key step in anatomic dissection. The subcutaneous layer is initially divided in the line of the primary skin incision and then is separated from the surface of the deep fascia around the dorsal, medial, and lateral aspects of the metatarsophalangeal joint. This enhances surgical hemostasis, preserves the viability of the surrounding tissues, and minimizes the risk of postoperative edema, hematoma, and other wound complications.
The subcutaneous layer, or superficial fascia, is actually composed of two tissue layers between which the cutaneous vessels and nerves traverse. The outer fatty layer, or panniculus adiposus, contains the venous tributaries and is attached to the deep fascia by a thin, membrane-like film (53). This membrane attachment creates the dissection plane to be followed when separating the superficial fascia from the deep fascia in anatomic dissection or tissue plane separation. Accurate and clean separation of the superficial fascia from the deep fascia preserves the cutaneous neurovascular structures.
Technique
With separation of the wound edges through the initial dermal incision, the subcutaneous tissues are visualized. Superficial
veins that cross the line of incision are clamped, cut, tied, or coagulated with electrocautery.
veins that cross the line of incision are clamped, cut, tied, or coagulated with electrocautery.
The technique of tissue plane dissection around the first metatarsophalangeal joint is best initiated over the dorsal aspect of the shaft of the proximal phalanx. At this point, the subcutaneous tissues are easily separated from the deep fascia or extensor retinaculum overlying the extensor hallucis tendon. It is not necessary to separate the subcutaneous layer throughout the entire length of the incision at this time.
The subcutaneous layer is separated down to the level of the deep fascia from the distal end of the incision proximally to the base of the proximal phalanx. A surgical sponge can be used to peel the subcutaneous tissues away from the medial and lateral aspects of the proximal phalanx without violation of the delicate deep fascial layer. This initial technique creates the primary division of the tissue layers, preserves the critical neurovascular structures within the subcutaneous tissues, and provides the “pocket” through which the rest of the dissection is performed.
Medial Subcutaneous Reflection
Reflection over the medial aspect of the joint capsule is initiated with insertion of the blunt end of the knife handle into the pocket at the medial aspect of the proximal phalanx. The knife handle is passed proximally between the tissue layers to separate the subcutaneous layer cleanly from the deep fascia and capsule over the medial aspect of the joint and more proximally along the shaft of the metatarsal. Dorsal attachments of the subcutaneous layer to the deep fascia may be released with scissors or a sharp knife, with care taken to avoid laceration of the linear course of the medial nerve and vascular structures.
Increased exposure of the plantar medial aspect of the joint capsule is usually accomplished with a side-to-side brushing stroke of the surgical knife that peels the subcutaneous tissues away from the inferior margins of the joint capsule and the course of the abductor hallucis tendon. Care must be taken to avoid laceration of the plantar medial neurovascular structures and the perforating capsular vein at the proximal and inferior aspect of the metatarsal neck. The clean separation of subcutaneous tissues from the deep fascia allows this surgical procedure to be performed with minimal bleeding even without the use of a tourniquet.
Lateral Subcutaneous Reflection
Dissection into the intermetatarsal space is initiated with a similar reflection of subcutaneous tissues away from the deep fascia over the lateral aspect of the metatarsophalangeal joint. A surgical sponge is again used to peel the superior level of subcutaneous tissues away from the deep fascia along the course of the extensor tendons. A deep pocket is initiated along the lateral aspect of the proximal phalanx with finger dissection. The surgeon can easily separate the subcutaneous tissues down to the inferior edge of the proximal phalanx and then palpate the fascial expansions that cross the proximal intermetatarsal space.
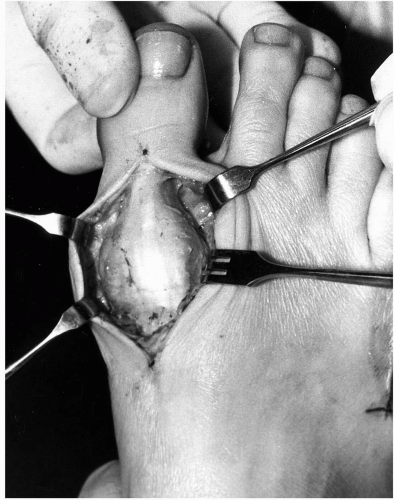 FIG. 1. Universal incision for hallux valgus repair: dorsal medial incision with subcutaneous reflection medially and laterally. |
Proximal dissection into the interspace is carried along the fascial plane to separate the subcutaneous tissues from lateral aspect of the metatarsophalangeal joint capsule (Fig. 1). A Weitlaner retractor is helpful for maintaining retraction. Metzenbaum scissors or another form of controlled dissection is used to separate the subcutaneous tissues gently from the lateral fascial surface. The subcutaneous dissection is carried to the floor of the intermetatarsal space, which is composed of a transverse structure consisting of either communicating fibers of the dorsal extensor retinaculi from the first and second metatarsophalangeal joint or a superficial portion of the deep transverse intermetatarsal ligament (54). This communicating expansion needs to be transected to expose the adductor tendon and other deep plantar lateral structures for manipulation or release. The deep portion of the transverse intermetatarsal ligament is preserved to maintain the sling mechanism and to stabilize the first ray segment (55).
Tissue plane dissection is made more difficult in patients who have undergone previous surgical procedures. In these instances, extension of the primary incision proximal or distal to the surgical scar allows one to initiate tissue plane dissection, which can be extended into the wound to restore normal tissue plane relationships.
FIRST INTERSPACE DISSECTION
Sequential Release of Plantar Lateral Contracture
Contracture of the plantar lateral structures of the metatarsophalangeal joint is one of the primary deforming forces of the great toe joint in hallux abducto valgus deformity and is largely responsible for the progressive nature of the condition. Failure to release this area of contracture adequately can lead to recurrence of deformity after surgical intervention. Therefore, the release of plantar lateral joint contracture is a primary component of hallux valgus correction.
Release of plantar lateral contracture can be accomplished by different surgical approaches (46, 47, 48, 49, 50, 51, 52). Weil (personal communication) addressed the lateral structures through an intraarticular technique consisting of tenotomy of the adductor tendon and sectioning of the lateral sesamoidal ligament. Tenotomy of the lateral head of the short flexor as well as release of the lateral collateral ligament may also be performed through this approach as needed. The advantage of this technique is that it avoids additional dissection into the intermetatarsal space.
Release of plantar lateral contracture by dissection into the intermetatarsal space provides direct exposure of the anatomic structures affected, the ability to perform tendon transfer techniques, and access for removal of the fibular sesamoid if necessary. The first objective of dissection in the intermetatarsal space is to provide direct visualization and specific identification of the individual anatomic structures of the deep intermetatarsal space. Joint motion is evaluated before and after release of individual anatomic structures in a controlled and sequential manner. The dissection is terminated once a free and congruous motion of the metatarsophalangeal joint is created.
The specific sequence of release to be performed in the first intermetatarsal space is as follows:
Adductor hallucis tendon
Fibular sesamoidal ligament
Tenotomy of the lateral head of the flexor hallucis brevis
Excision of the fibular sesamoid
The technique begins with release of the adductor tendon but progresses only as needed to release the contracture effectively and to allow unrestricted sagittal range of motion of the metatarsophalangeal joint. With each additional step in the release process is an increased potential for lateral instability. However, without these steps or other appropriate measures, lateral contracture may persist and may encourage recurrence of the hallux abducto valgus deformity. Therefore, the surgeon is attempting to recreate a more normal balance of the soft tissues at the joint level.
Release of the Adductor Tendon
The adductor tendon is the first of the deforming structures to be evaluated and released. Adequate exposure and an understanding of the anatomy allow the surgeon to perform the dissection in a deliberate manner without compromising the neurovascular or joint structures (56). Although some authors have questioned the safety of interspace dissection (57, 58, 59, 60), more current evidence supports the concept that this maneuver can be safely performed without significant disruption of vital blood supply (61, 62, 63, 64, 65, 66).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








