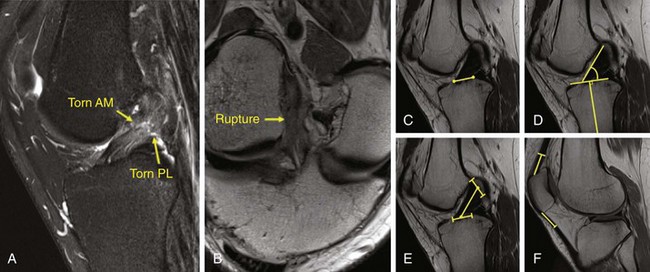
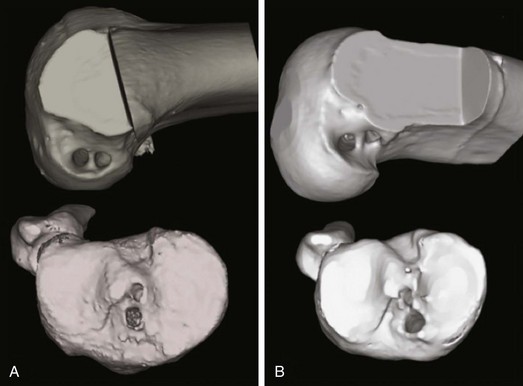
Chapter 77 Over the last two decades, single-bundle anterior cruciate ligament (ACL) reconstruction has largely been a successful operation.1 Many patients over the short term have been able to return to sports with an improvement in subjective instability of their knee. However, recent studies have also found that a subset of patients experience persistent subjective knee instability and therefore are not able to return to prior activity.2 Furthermore, long-term evaluation of patients suggests that osteoarthritic changes occur at the same rate as in knees that have not undergone surgery.3,4 For example, a recent randomized controlled trial found radiographic degenerative changes in 84% of the subjects 11 years after ACL reconstruction.5 Results such as this, presented in many other papers,3,4,6 have pushed the focus of ACL reconstruction toward an anatomic approach to more closely restore normal knee function and avoid long-term osteoarthritic changes. Anatomic reconstruction of the ACL is defined as the functional restoration of the ACL to its native dimensions, collagen orientation, and insertion sites.7 The aim of anatomic ACL reconstruction is to provide the patient with the greatest potential for a successful outcome. Four fundamental principles should be observed for achievement of this goal. The first is to carefully note the patient’s native anatomy. The second is to individualize each surgery with respect to the patient’s anatomy. The third is to place the tunnels and grafts in the center of the patient’s native footprints. The fourth is to reestablish knee biomechanics by tensioning the grafts to mimic the native ACL as closely as possible.8 The traditional anteromedial (AM)-based single-bundle ACL reconstruction was shown to successfully resist anteroposterior (AP) translation forces, but failed to correct rotational instability of the injured knee leading to abnormal knee kinematics.9,10 It is presumed that with this condition there is an altered wear pattern and subsequent premature evidence of osteoarthritis. Therefore, increasing efforts have been made during the past decade to restore normal knee kinematics. The “forgotten” posterolateral (PL) bundle, which plays an important role in both knee stability in extension and knee rotation in flexion, was found to be indispensable. Several studies have shown the clinical superiority of double-bundle (DB) reconstruction in restoring AP and rotational stability compared with the traditional single-bundle (SB) procedure.11–17 High-quality magnetic resonance imaging (MRI) is used to help identify the rupture pattern of the ACL and associated injuries. Special sequences such as oblique coronal and oblique sagittal views enhance ACL visualization (Fig. 77-1A and B) by cutting MRI sections in the same anatomic alignment as the ACL. MRI also plays a definitive role in preoperative planning for individualized surgery. Measurements of the tibial insertion site, ACL length, ACL inclination angle, and quadriceps and patellar tendon thickness on sagittal view are routinely employed to help determine reconstruction technique and graft choice (Fig. 77-1C to F). For example, DB reconstruction is indicated if the tibial insertion site measures more than 18 mm. An insertion site size less than 14 mm does not easily permit the drilling of two separate tunnels while a 2-mm bone bridge is maintained between them. In this scenario, an SB reconstruction would be the better option.18–20 In insertion sites between 14 and 18 mm, either an SB or a DB procedure can be performed. In revision surgeries, three-dimensional computed tomography (CT) scans prove invaluable in identifying previous tunnel placement and bony erosions in relation to the normal ACL insertion sites. Visualization of tunnel placement and anatomic changes aides in surgical planning—determining whether a new tunnel can be drilled, whether the old tunnels can be reused, or whether a two-stage procedure involving bone grafting should be performed instead8 (Fig. 77-2). Once the patient is under anesthesia, a thorough physical examination is conducted and the findings are compared with those of the contralateral extremity. Range of motion, results of Lachman, pivot shift, anterior and posterior drawer, and valgus and varus stress tests, and external and internal rotation at 30 and 90 degrees of knee flexion are documented. The patient is positioned supine on the operating table with the affected knee secured in a leg holder and bent over the end of the table in 90 degrees of flexion. The patient setup should allow at least 120 degrees of knee flexion and full extension (Fig. 77-3), as well as valgus and varus stress. A pneumatic cuff is positioned on the upper thigh of the injured limb and inflated to 250 to 350 mm Hg depending on the size of the patient’s limb and his or her mean arterial pressure. The contralateral limb is positioned in the high lithotomy position away from the surgical field. Care is taken to pad the nonoperative leg to avoid complications such as tourniquet effect or neurologic palsy.
Anatomic Anterior Cruciate Ligament Concept
Single- and Double-Bundle Anterior Cruciate Ligament Reconstruction
Preoperative Considerations
Imaging
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine