Chapter 2 Anatomic Aberrations
Skeletal Abnormalities
Femur
Trochlear Dysplasia
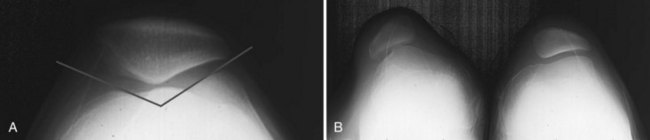
Trochlear dysplasia may be relatively subtle or more marked. Clinical manifestations depend not only on the extent of the dysplasia but also on other anatomic factors such as soft tissue tension. Symptoms may relate to chronic maltracking or frank dislocation. Pain related to the patellofemoral joint resulting from chronic patellar malalignment is typically manifested as an anterior knee ache when sitting with the knee flexed and as acute exacerbations during squatting, kneeling, and stair-climbing activities. On physical examination, crepitus from the patellofemoral joint, pain with patellar compression, and peripatellar tenderness may be noted. Specific radiologic criteria have been reported that define normal trochlear anatomy.8 The sulcus angle is defined on the Merchant view by the intersection of lines connecting the highest point of the femoral condyles to the deepest point of the femoral trochlea; the mean angle in normal knees is 130 to 137 degrees (range, 112 to 151 degrees).1,40 Significant differences in this angle have been reported in patients with recurrent patellar dislocation and chondromalacia patellae (Fig. 2-1).1 The lateral/medial trochlear ratio is the ratio between the segments joining the highest point of the femoral condyles to the deepest point of the trochlea. A ratio greater than 1.7 indicates trochlear dysplasia.8 If nonoperative treatment such as activity modification and physical therapy fails to relieve symptoms, lateral release and proximal realignment may be considered in patients with disabling symptoms and documented anatomic abnormalities. In carefully selected patients, 91% excellent and good results were achieved at intermediate-term follow-up by Insall et al.54 In a small group of pediatric patients with a severely dysplastic trochlea, successful results have been reported after a sulcus-creating procedure performed in conjunction with soft tissue realignment.9
Patella
Congenital Absence and Hypoplasia
Congenital absence of the patella and hypoplasia are extremely rare anomalies, especially as isolated findings.12,100 An association with other abnormalities has been reported, including ischiopubic malformations, and they have been described as part of the nail-patella syndrome (nail and patellar dysplasia, radial head subluxation and elbow malformation, renal abnormalities, and iliac horns).100,103 Other patellar dysplasias include duplication in the coronal and sagittal planes; in some cases, these abnormalities have been associated with multiple epiphyseal dysplasia.41,48,84,118
Bipartite Patella
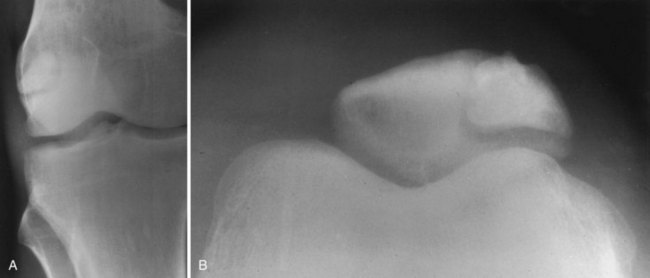
Anomalies of patellar development are relatively common, especially failure of accessory ossification centers to fuse, which can lead to bipartite, tripartite, and multipartite patellae (Fig. 2-2). Fragmentation of the patella has been noted in about 2% to 5% of knees. The bipartite type accounts for the majority of cases; approximately 50% of cases occur bilaterally.16,101,118 The Saupe classification describes three types of patellar fragmentation based on the location of the accessory ossification center: type 1 (5%) is located at the inferior pole, type 2 (20%) at the lateral margin, and type 3, the most frequent (75%), at the superolateral pole.16,101
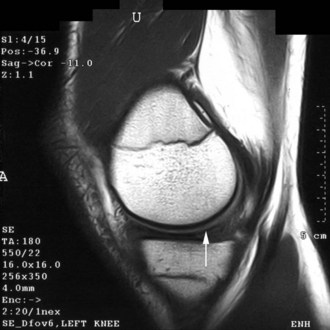
Most bipartite patellae represent incidental findings; only 13% are associated with symptoms. When pain develops, it may occur acutely after trauma or gradually.16,20,43,101,117 In the acute setting, a traumatic fracture must be ruled out. In such cases, the margins of the fracture fragments usually appear more ragged on plane radiographs, whereas the accessory fragments noted in atraumatic fragmentation tend to have sclerotic smooth margins. Magnetic resonance imaging (MRI) may be helpful in distinguishing incidental fragmentation because in these cases the accessory piece demonstrates low signal intensity without surrounding marrow edema (Fig. 2-3).101 Initial treatment may include activity modification, anti-inflammatory medication, and immobilization. In patients with persistent symptoms, successful excision of symptomatic fragments has been reported.16,43,101,117
Ligament Abnormalities
Anterior Cruciate Ligament
Congenital Absence
Congenital absence of the anterior cruciate ligament (ACL) is a rare anomaly that has been reported, in most circumstances, to occur in association with other knee abnormalities, including congenital knee dislocation, tibial dysplasia, congenital dislocation of the patella, femoral dysplasia, ring meniscus, discoid meniscus, absence of the meniscus, absence of the posterior cruciate ligament (PCL), and congenital leg length discrepancy.3,60,76,111 An association with other musculoskeletal abnormalities not limited to the knee has also been reported, with at least one other significant anomaly noted in each patient in one series.111 However, rare cases of isolated absence of the ACL have been reported in otherwise normal individuals.7 On physical examination, a positive anterior draw test and a 3+ Lachman test are common findings. Complex instability may also be noted; in one study, 25% of patients demonstrated medial and lateral translational instability.111 Therefore, it is evident that this patient population is not entirely analogous to the group that experiences traumatic ACL rupture. Radiographic features that have been associated with congenital absence of the ACL include hypoplasia of the lateral aspect of the tibial spine, hypoplasia of the lateral femoral condyle, a narrow or tight A-frame intercondylar notch, and hypoplasia of the medial part of the tibial plateau.60,111 Many patients with this anomaly are asymptomatic as children and do not complain of instability.60 Because the long-term consequences of this type of deficiency are unknown, the need for ligament reconstruction has not been clearly defined. In several series, asymptomatic patients have been treated by observation only with good short-term results.7,57,111
Other Abnormalities
An abnormal origin of the ACL has been described. Rather than the usual discrete origin, an origin extending completely between the anterior and posterior margins of the intercondylar notch was observed in a young child. Symptoms developed in this patient as a result of impingement of the abnormal ACL against the anterior portion of a discoid lateral meniscus at approximately 100 degrees of flexion.49
Posterior Cruciate Ligament
Abnormalities of the PCL are extremely rare. Congenital absence of the PCL has been reported in association with other congenital anomalies, including absence of the ACL, leg length discrepancies, and Larsen’s syndrome (multiple congenital dislocations of the elbows, knees, and hips and unusual facies).36,57,60 The multiple anomalies present in these patients typically result in positive anterior and posterior draw tests and posterolateral rotatory instability. In one patient, an anomaly of the PCL has been reported in association with congenital absence of the ACL. An anterior insertion of the PCL on the tibia was noted to compensate for the aplastic ACL.3
Meniscal Abnormalities
Anomalous Attachments
A variety of anomalous attachments of the medial meniscus have been described, including insertion of the anterior horn into the ACL, intercondylar notch, and infrapatellar fold and insertion of the posterior horn into the ACL.* Between 10.6% and 22.6% of all Asian patients undergoing arthroscopy were found to have anomalies of the anterior horn of the medial meniscus.78 In a large study of 953 arthroscopies, 103 (10.8%) knees did not demonstrate the normal attachment of the anterior horn of the medial meniscus onto the tibia. Four variants of the anterior horn were observed in this study: 51 (49.5%) had only an attachment to the lateral meniscus via the transverse intermeniscal ligament, 39 (37.9%) inserted into the ACL, 11 (10.7%) inserted into the coronary ligament, and 2 (1.9%) inserted into the infrapatellar synovial fold. In these patients, the abnormal anterior horn attachment rendered the anterior portion of the meniscus hypermobile, while the posterior body remained firmly attached. This aberration predisposed patients to symptomatic tears at the junction of the midbody and the posterior body as a result of accumulated stress.78 Successful arthroscopic resection of symptomatic anomalous insertions has been reported.97,102 In these cases, a stable, normal-appearing anterior horn was fashioned, which relieved the preoperative knee pain. In one case, symptoms appeared to be related to subluxation of the abnormal bundle under the femoral condyle with flexion.97 Nonetheless, other authors have reported good results after observation of incidentally discovered anomalies.13,59
Hypoplasia and Congenital Absence
The incidence of hypoplasia and congenital absence of the medial and lateral menisci is unknown. An association with other ipsilateral knee and generalized musculoskeletal anomalies, including congenital absence of the ACL, discoid lateral meniscus, thrombocytopenia–absent radius syndrome, and anomalous insertions of the popliteus tendon, has been reported in several cases.37,77,112,113 The association of simultaneous intra-articular anomalies in some cases is probably due to the common mesenchymal origin of several structures.13 Condensation of the menisci takes place at approximately 7 to 8 weeks of embryologic development and occurs in concert with the intra-articular cruciate ligaments.13,24,102
Discoid Meniscus
The first discoid meniscus was reported by Young in 1889.2,28,58,99 In an early report, Smillie104 described three variants: primitive, intermediate, and infantile. This classification reflected the belief that the menisci are discoid in a normal fetus and gradually assume an adult form through resorption of the central part; however, anatomic studies have suggested that this supposition is incorrect because discoid menisci do not occur during any part of routine development.24,58,62,93 Kaplan62 suggested that abnormal motion of the lateral menisci resulting from deficient peripheral attachments may cause a meniscus that is normal at birth to become discoid during development.14 However, this explanation does not satisfactorily account for the occurrence of discoid medial menisci. Rather than representing an arrest in normal development, discoid menisci are believed to be congenital anomalies.14,28
Medial
Discoid medial menisci are very rare phenomena. The first undisputed case was reported by Cave and Staples22 in 1941. Its incidence in the general population is reported to be approximately 0.06% to 0.3%.14,25,28,99 Discoid medial menisci may be asymptomatic, especially in children and adolescents. Meta-analysis has revealed that 65% of all patients with symptomatic discoid medial menisci were older than 18 years.28 The most common symptoms associated with a discoid medial meniscus are the same as those for a medial meniscal tear and include aching medial joint line pain, intermittent swelling, locking, weakness, instability, and an inability to extend the knee fully.14,28,58 On physical examination, a block to full extension, effusion, joint line tenderness, and a positive McMurray test may be noted.28
Radiographs of the involved knee are usually unremarkable; abnormalities are identified in less than 10% of patients with a discoid medial meniscus.28 Occasionally, medial joint space widening or deepening of the medial tibial hemiplateau has been observed but may be subtle.14,28 MRI is the best test for identifying discoid menisci. On sagittal views, the menisci should be monitored on serial images. Rather than the usual central tapering between the anterior and posterior horns as the image plane moves laterally toward the intercondylar notch, the horns remain in continuity (Fig. 2-4). Visualization of a continuous band of meniscus on more than three peripheral sagittal images indicates a discoid meniscus. In addition, on coronal images, an abnormally thick meniscus, which can extend into the notch, may be visualized.14
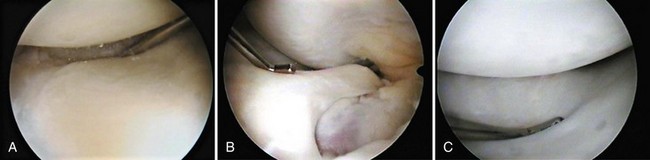
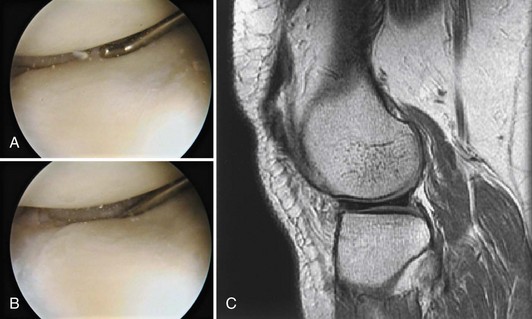
Because of the rarity of this phenomenon, its treatment has not been extensively reported. Several authors have suggested that incidentally discovered intact discoid menisci may be left intact.14,64 However, in these cases, the presence of central and inferior surface cleavage tears, which may be difficult to observe, should be excluded.25,99 In patients with intra-articular symptoms and no other abnormalities, discoid menisci should be very carefully examined for incomplete inferior or cleavage tears, because they may be missed if only the superior surface is examined (Fig. 2-5).
Successful short-term results of arthroscopic débridement with partial meniscectomy and contouring of discoid medial menisci have been reported.14,64 Because many symptomatic patients are initially seen as young adults, we attempt to fashion as nearly normal a functional meniscus in the hope of minimizing the long-term degenerative changes associated with meniscectomy.34
Lateral
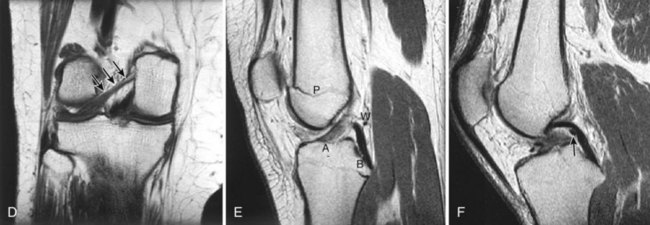
Discoid lateral menisci occur more frequently than on the medial side of the knee (Fig. 2-6). In the general population, the incidence has been reported to be approximately 1.4% to 15.5%, but certain races appear to have a higher incidence.29 Whereas a discoid lateral meniscus is thought to occur in less than 5% of white individuals, it has been identified in up to 16.6% of Asians.21,53 Washington et al identified three types of discoid lateral menisci based on the degree of coverage of the tibial plateau and the presence or absence of normal posterior attachments,116 including incomplete and complete discoid menisci, which have normal posterior tibial attachments via the coronary ligament, and the Wrisberg type, which lacks the usual posterior tibial attachment, with only one attachment posteriorly via the posterior meniscofemoral ligament (ligament of Wrisberg). Because the Wrisberg type often is not associated with a true discoid appearance, Neuschwander et al75 suggested that this anomaly be classified as a separate entity—the lateral meniscal variant with absence of the posterior coronary ligament. Although somewhat rare, discoid lateral menisci have been noted to occur in association with a number of other anomalies, including hypoplasia of the lateral femoral condyle, hypoplasia of the lateral tibial spine, a high fibular head, abnormal ACL attachment, and anomalous insertions of the medial meniscus.49,64
Patients may have symptoms related to a discoid lateral meniscus in childhood or middle age. The classic complaint of patients with a discoid meniscus is a snapping or popping knee.2,116 However, in one large series of 62 symptomatic patients, knee pain was the most common problem (89%); other frequent complaints at initial evaluation included the classic clunk or click (58%), swelling (48%), locking (27%), and giving way (19%).2 On physical examination, the pathognomonic clunk related to abnormal motion of the meniscus as the knee is brought into full extension was elicited in 39% of patients in the same study; other frequent findings included joint line tenderness (35%), effusion (19%), and locking (11%).2 Radiographic findings, including widening of the lateral joint line (8%), cupping of the lateral tibial plateau (5%), and sclerosis of the lateral tibial plateau (3%), were identified in a minority of patients.2 MRI can predictably identify discoid menisci and associated meniscal tears (Fig. 2-7). Treatment of incidentally identified intact complete and incomplete discoid lateral menisci is not thought to be necessary. However, as with medial discoid menisci, tears may be difficult to see and could be missed.45 In particular, inferior surface cleavage tears should be carefully excluded, especially in patients with intra-articular symptoms and no other identifiable lesions.
Treatment of symptomatic tears in both complete and incomplete types is somewhat controversial. Some authors reported successful results after compete meniscectomy, and in some studies, the results appear to surpass those achieved after partial meniscectomy and saucerization.53,116 Radiographic changes consistent with significant degenerative alterations in the lateral compartment after complete meniscectomy for discoid menisci in children have rarely been noted; this is believed to reflect possible adaptive changes of the knee and mechanical alignment.2,116 However, in one study, early degenerative changes were noted in three of eight patients at 17 years’ follow-up.116 Moreover, significant long-term consequences of meniscectomy have been documented in other circumstances.70 Concern regarding the potential for early degenerative disease has prompted many authors to advocate arthroscopic partial meniscectomy with salvage of the most functional remnant possible.11,29,30,45 Excellent short-term results have been reported with this strategy.11,29,30,83 We believe that even though the long-term outcome is not clear, the potential consequences associated with early degenerative arthritis in this young patient population make arthroscopic partial meniscectomy and saucerization with resection to a stable, well-contoured remnant the preferred treatment of symptomatic tears of complete- and incomplete-type discoid menisci.
Treatment of a Wrisberg-type discoid meniscus, which is inherently unstable because of lack of posterior tibial attachments, has traditionally involved complete meniscectomy. However, successful reattachment by suturing the posterior horn to the capsule has been reported, and in a small series of six patients treated in this manner, no clinical retears were noted at a mean of 32 months.75,92 If the long-term results are also successful, this treatment is again theoretically more appealing than complete meniscectomy when the long-term incidence of degenerative changes is not clear.
Other Structural Meniscal Anomalies
Extremely rare structural abnormalities have been reported, including ring-shaped lateral menisci and accessory lateral menisci that appear as a double-layered meniscus.4,32,65,76,109 When symptoms were believed to be related to these abnormalities, arthroscopic resection of the abnormal portion of the meniscus has proved successful.
Meniscofemoral Ligaments
The anterior and posterior meniscofemoral ligaments (of Humphry and Wrisberg, respectively) run between the posterior horn of the lateral meniscus and the intercondylar notch (Fig. 2-8). They embrace the PCL and are named for their location relative to the ligament. The presence of the anterior meniscofemoral ligament (of Humphry) is less consistent, with an incidence of 33% to 83% in anatomic studies; the posterior meniscofemoral ligament (of Wrisberg) is a more constant structure and is noted in 90% to 93% of the same specimens.87,115 Overall, 100% of the specimens had at least one of these ligaments. In other studies, one or the other of these meniscofemoral ligaments was identified in 71% to 94% of specimens.46,90,114 In general, the ligament of Wrisberg is more robust than the ligament of Humphry.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree