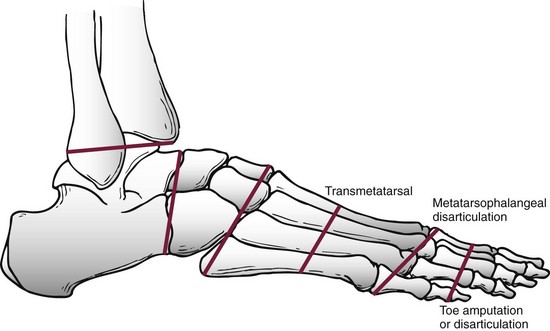
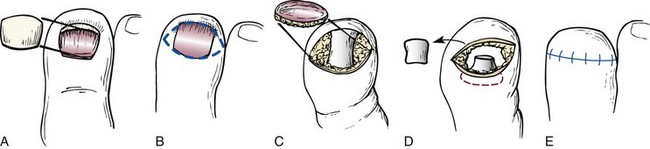
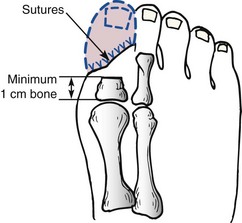
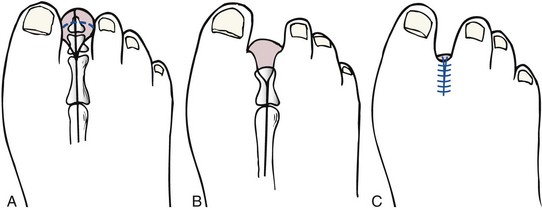
Chapter 28 SPECIFIC AMPUTATION LEVELS AND TECHNIQUES (Video Clips 1, 2, 3, and 130 Amputation of the Distal Toe and Nail Amputation of the Great Toe Through the Proximal Phalanx Base Metatarsophalangeal Disarticulation of the Great Toe Ray Amputation and Partial Forefoot Amputation All photographs in this chapter with the exception of Figure 28-24 are copyrighted by James W. Brodsky, MD. Once a decision to amputate has been made, a number of challenges remain. These include selection of the proper level of amputation (Fig. 28-1), methods of foot salvage to maximize function, proper surgical technique, postoperative management, and footwear modification and the use of prostheses. The many causes of partial or complete foot amputation include the following: 1. Diabetes (many diabetic patients also have peripheral vascular disease) 2. Peripheral vascular disease (in the absence of diabetes) 3. Trauma (most often lawnmower injuries and motorcycle trauma) 4. Chronic infection (primarily osteomyelitis) Amputation of part or all of the foot is correctly viewed as a procedure of last resort and reflects the surgeon’s proper desire to save the foot. The term foot salvage emphasizes the contemporary shift from complete to partial foot amputations. The goal is to convert many of the procedures that in the past would have been below-knee amputations to partial foot amputations and, in the process, to convert these patients to users of modified footwear rather than users of prosthetic limbs.53 The goals of an amputation are fundamentally greater in the patient who requires ablative surgery as a result of trauma than the goals in patients requiring amputation for diabetic foot problems. The diabetic patient or the patient with insensitivity, from any cause, needs to achieve a plantigrade foot with stable healing of the wounds and the lowest possible risk for future ulceration. The patient whose amputation is a result of trauma also needs an extremity that is not painful. This is compounded by an increased proclivity of traumatic amputations to develop symptomatic neuromas and complex regional pain syndrome (CRPS, reflex sympathetic dystrophy). The advantages and disadvantages, as always, are two sides of the same coin. The traumatic amputee is not subject to the same frequency of recurrent problems and multiple revisions of the amputation to a higher level (not to mention risk to the contralateral leg21) as a diabetic patient because the (presumably sensate) limb of the traumatic amputee has sufficient sensation to prevent neuropathic breakdown of the soft tissues. One of the major goals in amputation surgery of the foot is to salvage as much of the functioning foot as possible. The general principle holds true that preservation of a greater portion of the limb allows greater function. The classic experimental basis for limb preservation was documented in a study done at Rancho Los Amigos Hospital, which showed increasing energy costs of walking, as evidenced by greater oxygen consumption, in patients who had higher levels of amputation.54 The two qualifications of that principle are that the salvaged foot must achieve complete healing with a stable soft tissue envelope, and the foot must be sufficiently plantigrade to be functional. Although the use of tourniquets in amputation surgery has often been proscribed in the past, the experimental basis for this prohibition is lacking. A controlled, randomized trial of tourniquet use in foot amputations in diabetic and dysvascular nondiabetic patients demonstrated no difference in healing rates between patients with tourniquets and those who did not have tourniquets applied.6 In this series, the tourniquet was released once the amputated part was removed, before beginning the closure, to check for hemostasis and flap viability. Use of tourniquets requires three other considerations: the location, the type of tourniquet, and the presence of underlying vascular bypass grafts. For partial foot amputations, if a tourniquet is desired or needed, an Esmarch bandage just above the malleoli is safe and effective.6,7 For more proximal amputations, a thigh tourniquet is required and thus must be a pneumatic tourniquet. Although easy to use, thigh tourniquets can inhibit quadriceps function postoperatively, which may be a consideration in some patients. Surgeons are reluctant to place a tourniquet over this area in patients with vascular bypass grafts. If doubt exists about the viability of an area, the area can be preserved and observed and then further debrided at the next session in the operating room. Especially with an infected wound, the patient might require two or three sessions in the surgical suite: the first time for initial, aggressive debridement; the second time, if needed, for redebridement of residual areas of infection or necrosis after a period of intervening wound care; and definitive closure at that or a subsequent session. Occasionally, it is necessary to expand the middle step to more than one secondary debridement. After the debridements, the wound is usually left open to allow drainage and wound care. Surgical redebridement at intervals augments wound care until the wound is clean or has good granulation. In many cases, the focus of infection is sufficiently distal or localized that the debridement and closure can be done in a single session (see the discussion of surgical treatment of infection in Chapters 16 and 27). Failure to achieve primary or delayed primary closure in a large number of cases signifies poor decision-making. Leaving large gaping wounds to granulate inward as the main method of healing amputations, especially in diabetic patients, condemns the patient to an unnecessarily and very long recovery (Fig. 28-2). This technique often represents the surgeon’s failure to make a decision about the viability of the local tissue and the appropriate final level of healing. It is more effective and far more cost-effective, not to mention less debilitating to the patient, to establish an assessment of the vascularity and healing potential of the partial foot amputation wound and do a definitive procedure with good, viable local closure. If needed, the limb should first be revascularized by the vascular surgeon and then redebrided and eventually closed at the new level of viability. Allowing an entire amputation wound to granulate slowly is an extremely slow process. Large wounds that are left to granulate very often require skin grafting and produce an irregular scar or an invaginated skin surface. The process of wound contracture can be hindered by the shape of the wound and the amount of residual bone structure beneath. Delayed primary closure is valuable, even if it only achieves partial closure of the wound. It reduces the amount of coverage to be achieved and speeds healing. In such cases, the wound flaps adhere over part of the wound’s length, and a portion fails to close and continues to drain small amounts. This still reduces the morbidity because the residual wound that must be treated and that must granulate inward is still only a fraction of the original wound’s size.32 The validity of this concept has been reaffirmed by the advent of negative-pressure wound dressings.11,16,33,45 Bypass is the most common of these techniques. Balloon angioplasty is applicable primarily to discrete, well-localized (and usually proximal) occlusive lesions, which are relatively uncommon in diabetic patients and more common above the popliteal artery in nondiabetic vascular disease. In the nondiabetic patient, bypass usually takes the form of proximal bypass of a major occlusion at the iliac, femoral, or popliteal levels. In the dysvascular diabetic patient, similar proximal occlusions or stenoses occur and respond well to a vascular bypass. In addition, and very commonly, diffuse occlusions of the arteries distal to the trifurcation of the popliteal artery can occur in the lower part of the leg. Unlike in the nondiabetic patient, these are not discrete blockages but usually consist of atherosclerotic involvement diffusely through the vessel. Bypass done down to the level of the ankle may use in situ or reversed saphenous vein grafts. The emphasis should be on doing the revascularization before fashioning the final amputation flaps. Preferably, the final level of amputation is determined once maximum tissue perfusion has been achieved.8 The customary surgical techniques described here are basic guidelines, not absolute requisites, for successful amputations. No matter what the conscientious surgeon does, some amputations will fail and will need to be revised to a higher level. If every amputation heals primarily, the surgeon may be doing some amputations at too-proximal a level and not achieving enough salvaged cases from the feet. Often, several procedures and revisions are needed before the final result is obtained, and the revisions do not prejudice the quality of the ultimate result; rather, they make the attempt at foot salvage worthwhile.23,25,29 Healed amputations that result from revision procedures yield satisfactory results similar to those that heal after a single level of amputation. Once partial amputations of the foot heal, the reported rate of revision is as low as 10%, thus indicating that these function as definitive procedures. The surgeon uses imaging and laboratory data, clinical experience, and surgical judgment to select the level for partial foot amputation. A plethora of tests have been promulgated in the surgical and orthopaedic literature as the “best” method to determine the proper level of amputation. Most are based on statistical review of ultimate healing of the amputated limb and the correlation with predicted healing from the test. These procedures include arterial Doppler pressure measurements, fluorescein angiography, transcutaneous oxygen tension measurements, and xenon clearance.12,37,40,57 The most commonly used and widely available test is the arterial Doppler ultrasound. This is most useful as a guideline to general levels of perfusion and is the best initial screening test to determine whether the patient needs a vascular surgery consultation and an arteriogram. The Doppler ultrasound is painless, quick, and inexpensive and does not require extensive instrumentation. As discussed in the section on vascular evaluation in Chapter 27, the pulse-volume recordings (waveforms) are reliable indicators of perfusion, but ratios of ankle pressures to arm pressures can be unreliable, especially in the diabetic patient with noncompliant, calcified vessels that give falsely elevated pressures. For healing of distal amputations, the most reliable measures are toe pressures. A forefoot amputation is likely to heal with a toe pressure of 40 mm Hg or greater. Distal wound healing in the presence of toe pressures between 30 and 40 mm Hg is possible but less predictable.3 Some authors advocate transcutaneous oxygen measurements. These measurements are clearly much more cumbersome to perform than Doppler studies. The readings must be obtained in an environment of controlled temperature because they are temperature dependent, and they are time consuming to perform. On a practical level, an adequate number of readings cannot be done efficiently without multiple simultaneous probes. No equivalent to Doppler toe pressures exists; thus this technique does not offer information about healing of the most distal procedures. Recent studies have questioned the reliability of transcutaneous oxygen measurements.47 The real question is to what degree the surgeon finds a correlation of test results with wound edge bleeding at surgery and with the healing rate of amputation wounds in that particular institution. Other factors that affect healing include edema in the local tissues, systemic disease, and nutritional factors. Systemic factors include glycemic control in diabetic patients or vasculitis in patients with inflammatory arthritides. As noted in Chapter 27, simple indices of nutritional status can have a predictive value for wound healing after amputation.14 Of course, the adequacy of nutritional status is important to achieving healing. Published measures of this are the total lymphocyte count, which should be greater than 1500/µL; serum albumin 3.5 g/dL or greater; total protein 6.2 g/dL or higher; and hemoglobin greater than 11 g/dL. 1. The nail plate is removed (Fig. 28-3A). An elliptic incision is centered over the distal aspect of the distal phalanx, encircling the toenail plate. The incision must extend sufficiently proximally to include all of the proximal and lateral eponychial folds to prevent partial nail regrowth (Fig. 28-3B). 2. The dorsal soft tissue, nail plate, and eponychial folds are excised as a single full-thickness mass down to the bone, to expose the distal phalanx (Fig. 28-3C). 3. The distal phalanx is transected with a bone-cutting forceps or small saw, and the distal fragment is removed (Fig. 28-3D). Approximately one third to half the phalanx is removed, depending on the amount of soft tissue for coverage. 4. The skin flap is shaped to minimize medial and lateral dog-ears, although the tissue will shrink and reshape after healing. 5. A single interrupted layer of sutures is used to loosely approximate and evert the skin edges. A loose skin closure usually allows adequate drainage and usually obviates the need for a drain (Fig. 28-3E). Although it is technically easier to amputate the great toe through a metatarsophalangeal (MTP) disarticulation, there are potential advantages to saving the base of the proximal phalanx. The minimum length of the base to save is about 1 cm (Fig. 28-4). This recommendation is both intuitive and scientific. The benefits of preserving the base of the phalanx for the subsequent gait of the patient and the pattern of pressure under the foot have been demonstrated in plantar pressure studies with the pedobarograph. The intuitive basis is that by saving the base of the phalanx, the attachments, and thus the functions, of the plantar fascia and flexor hallucis brevis tendon are preserved, at least partially. The independent plantar flexion mechanism of the first ray is not entirely lost, and some of the weight-bearing function of the first ray may be preserved, possibly reducing the transfer of pressure to the second and third metatarsal heads (Video Clip 3 1. A curvilinear skin incision is used to encircle the dysvascular or infected area and to excise nonviable tissue. 2. The surgeon determines the length of the flaps required for closure of the wound. At the base of the phalanx, or at the MTP joint, viable flaps must be present to the level of the distal part of the proximal phalanx. 3. Often, sufficient skin is present on the dorsoplantar aspect or mediolateral aspect of the hallux to enable the development of fish-mouth flaps (an alternative is a racket-type incision) (Fig. 28-5). 4. A power saw is used to transect the proximal phalanx at its base, leaving a minimum of 1 cm length. Rough edges are beveled with a rongeur. 5. If the base of the phalanx has been preserved, at least one of the sesamoids must be saved because the sesamoid complex attachment to the phalangeal base is the key to the function of the phalanx if it is to aid in maintaining some weight-bearing function of the first metatarsal. 6. The flaps are approximated with full-thickness, interrupted sutures of a nonreactive monofilament. Routine dressing changes are continued until adequate healing has occurred. In concept, it would seem preferable not to allow weight-bearing postoperatively in order to protect the wound and the suture line from shearing forces that would pull the wound apart. In reality, many patients are not physically able to sustain non–weight bearing for the reasons elaborated in Chapter 27. A compromise is to allow weight bearing on the hindfoot only, but this is more difficult to achieve than it appears. The use of partial shoes that allow the forefoot to hang over the distal edge of the shoe increases the pressure on the heel and hindfoot. Once a great toe has been amputated, a custom-molded filler in the shoe helps to compensate for and diminish sliding of the foot inside the shoe (Fig. 28-6).15
Amputations of the Foot and Ankle
![]() )
)
General Considerations
Surgical Considerations
Tourniquets
Soft Tissue Preservation
Wound Closure
Vascular Reconstruction
Determination of Amputation Level
Other Factors Affecting Healing
Specific Amputation Levels and Techniques (Video Clip 130
![]() )
)
Amputation of the Distal Toe and Nail
Surgical Technique
Amputation of the Great Toe Through the Proximal Phalanx Base
![]() ).
).
Surgical Technique
Metatarsophalangeal Disarticulation of the Great Toe
Postoperative Care
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree