Amputations
Robert P. Taylor
James L. Bouchard
Linnie V. Rabjohn
Lower extremity amputation (LEA) is one of the oldest known surgical procedures. Hippocrates wrote and described amputation surgical principles in 385 bc (1). Approximately 82,000 nontraumatic lower limb amputations are performed yearly in people with diabetes, which represents 60% of nontraumatic lower limb amputations done in the United States (2). Most LEAs are performed for ischemic disease of the lower extremity. Lower limb amputations accounted for 97% of all dysvascular limb loss. Of that 97%, 25.8% were performed at the aboveknee level, 27.6% at the below-knee level, and 42.8% involving numerous other levels (3,4). Of those dysvascular amputations, 15% to 28% of patients undergo contralateral limb amputations within 3 years, and elderly persons who undergo amputations have a 50% survival rate the first 3 years (1).
While amputation surgery is performed to remove nonviable or diseased tissue, it requires no less preoperative planning than any complex reconstructive surgical procedure, and fundamental surgical principles such as proper tissue handling, hemostasis, and appropriate closure techniques must be employed.
Partial foot or complete foot amputations offer several benefits over more proximal levels of amputation. One of the primary benefits of distal amputations is the decreased oxygen consumption required for ambulation. Studies clearly show that oxygen consumption increases as the amputation is performed more proximally. Therefore, the greater the amount of limb preserved, the less the energy required by the patient postoperatively for ambulation (5,6 and 7). It is the authors’ opinion that these findings help explain the astonishing shortened life span of patients after a proximal amputation. Therefore, to salvage a portion of the foot or the entire leg may provide a better prognosis in relation to the patient’s life span and quality of life. The benefit of foot preservation also includes the ability to stand and walk for short distances without an orthotic or prosthetic device, and for those who have a preexisting contralateral limb amputation, the ability to transfer with less effort (8). This can be very important in an emergent situation and also significantly increases the independence of the patients, allowing them to perform activities of daily living such bathing and using the restroom without aid.
Several medical advancements have significantly improved the outcome and prognosis of distal LEAs. The first advancement involves the ability to assess various wound healing parameters that help the surgeon accurately predict the success of distal amputations at various levels. These assessments include the patient’s vascular, nutritional, and medical status. Many of these parameters can be positively influenced preoperatively to increase the patient’s healing potential following the amputation. These parameters will be later discussed in the preoperative evaluation section. Another advancement involves the improvements in wound care and the availability and refinements of wound healing products such as bioengineered tissues and appliances such as wound vacuum systems. These products allow more distal amputations to be considered that otherwise would have required more proximal amputations to provide tissue coverage for closure. Finally, advancements in the materials, methods, and techniques used to manufacture prosthetic devices have provided improved functional outcome for the amputee (9).
PREOPERATIVE PATIENT ASSESSMENT
On presentation, the initial step in the patient assessment is an overall exam to determine if infection or sepsis is present. Septic patients require emergent incision and drainage and obtaining of cultures of the infected foot. The patient should be medically stabilized, and an infectious disease consultation should be obtained. In the septic patient, the definitive level of amputation may not be performed as the initial procedure. Septic patients often require multiple débridements, and the definitive level of amputation is not considered until all diseased or nonviable tissue has been removed (10).
Prior to amputation, appropriate consultations should also be obtained to optimize the patient’s medical status, maximize nutrition, control diabetes if present, and control the specific infecting organism as well (11).
Imaging studies should include plain film radiographs, CT scans, or MR imaging to assess the extent of diseased, infected, and nonviable tissue involved. This information will form the foundation for surgical planning to help ensure that the surgical margins are clear of devitalized and infected tissue.
The ability of the patient to heal must also be assessed. The patient’s healing capacity can be assessed by basic indices that were described by Dickaut and Pinzur et al, which are modifications of the original work by Wagner (9,12). From a nutritional and immunologic competence standpoint, the two most commonly used indices are total lymphocyte count and albumin level. Generally, a patient is felt to be deficient, with regards to the needed immune and/or nutritional levels to adequately promote healing, with a total lymphocyte count of less than 1,500/µ/L and an albumin level of less than 3.0 mg/24 hours (9,10). A total lymphocyte count of less than 1,500/µ/L indicates immune deficiency and increases the possibility of infection. A serum albumin level of 3.5 g/dL or less indicates malnutrition and diminished ability to heal the wound (1). A total protein level of 6.0 g/dL or higher is required to assure a minimum level of tissue nutrition. None of the indices should be used singly as indicators of nutritional status. Serum prealbumin levels should be considered in all patients with a borderline or questionable nutritional competence. Normal prealbumin levels range from 6 to 35 mg/dL. Levels under 10 mg/dL are indicative of moderate to severe nutritional deficiency. The prealbumin level is not generally influenced by external factors; therefore, it provides an accurate representation of nutritional status.
The prealbumin level can also be used to monitor the effect of dietary supplementation. All patients not meeting these minimum guidelines should receive a consultation with a dietician and undergo nutritional supplementation in the form of multivitamins and hyperalimentation of protein-rich foods (9).
The prealbumin level can also be used to monitor the effect of dietary supplementation. All patients not meeting these minimum guidelines should receive a consultation with a dietician and undergo nutritional supplementation in the form of multivitamins and hyperalimentation of protein-rich foods (9).
Other useful laboratory studies include C-reactive protein and hemoglobin levels. Increased C-reactive protein levels can be an indicator of infection, and a hemoglobin level greater than 10 g/dL is necessary for oxygenated blood for wound healing.
The presence of ischemia must always be evaluated and revascularization considered when possible (13). The leading indication for limb amputation in the United States is peripheral vascular disease (PVD) (1). In the patient with vascular disease, preservation of limb length must be balanced with wound healing ability and the potential for ambulation. A vascular surgery evaluation should be obtained when clinical signs and symptoms of PVD are present to determine the feasibility of vascular reconstruction in the hopes of maintaining limb length (1).
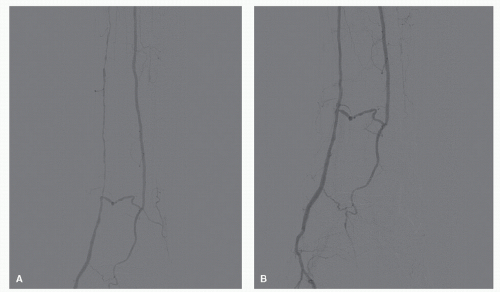
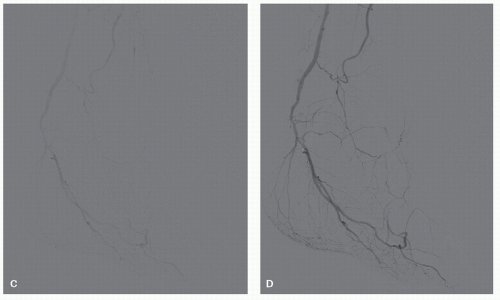
Poor vascular status distally has been a primary reason for many transtibial or transfemoral amputations; however, recent advancements in cardiovascular surgery and intervention offers the ability to improve the vascularity of the limb distally with minimally invasive procedures that can be done on patients who are not viable medical candidates for invasive vascular reconstruction (Fig. 71.1).
Doppler ultrasonography is used to measure arterial pressure. The area on the graph under the waveform is a measure of the flow. In approximately 15% of patients with PVD, the results are falsely elevated because of the noncompressibility of the calcified extremity arteries. Doppler ultrasonography has been used in the past to predict wound healing. A minimum measurement of 70 mm Hg is believed to be necessary for wound healing.
Ischemic index is another measurement used to help determine healing potential. This index is the ratio of the Doppler pressure at the level being tested to the brachial systolic pressure. An ischemic index of 0.5 or greater at the surgical level is necessary to support wound healing. An ankle-brachial index is the ischemic index at the ankle level and is believed to be the best indicator for assessing adequate inflow to the ischemic limb. An index that is lower than 0.45 often indicates that incisions distal to the ankle may not heal.
Transcutaneous oxygen pressure measurement is a noninvasive test that assesses the partial pressure of oxygen diffusing through the skin. This can be applied to any area of intact skin and records the oxygen-delivering capacity of the vascular system. Many believe this to be the most reliable and sensitive test for wound healing (14,15). Values greater than 40 mm Hg indicate acceptable wound healing potential. Values less than 20 mm Hg indicate poor healing potential. Pressure may be falsely low in areas of edema, cellulitis, and venous stasis changes (1).
SURGICAL PRINCIPLES AND PREOPERATIVE PLANNING
Extent of diseased tissue, assessment of the patient’s healing potential, changes in functional anatomy as a result of the amputation, and the patient’s socioeconomic responsibilities are all addressed in preoperative surgical planning to determine which level of amputation offers the patient the best overall prognosis. If these parameters are not considered and properly addressed, the patient can be left with a limb that is continuously prone to ulceration and infection or is not shaped well to accommodate an orthotic or prosthetic device. The complications of ulceration, infection, and deformity have caused many
surgeons to move to more proximal transtibial or transfemoral amputations and abandon partial foot or foot amputations.
surgeons to move to more proximal transtibial or transfemoral amputations and abandon partial foot or foot amputations.
The primary objective of LEA surgery should be to remove all diseased tissue while maintaining a functional stump (16). The benefits of preserving a portion of the foot include the ability to stand and walk for short distances without an orthotic or prosthetic device, and for those who have a preexisting contralateral limb amputation, the ability to transfer with less effort and requiring less oxygen consumption with activities (8).
FUNCTIONAL ANATOMIC CONSIDERATIONS
When performing a partial foot amputation, certain biomechanical tenets must be considered. The greatest length possible should be preserved in the foot. If the foot is shortened through amputation, the musculature responsible for dorsiflexion and plantarflexion must be rebalanced to compensate for the shorter lever arm acting on the triceps surae. If a resultant equinus is present, the surgeon should perform a tendo Achilles lengthening or tenotomy (17,18). If the amputation is performed at the level of the Lisfranc joint or at a more proximal level, there will be disruption of the primary inverters and everters of the foot and balance between these should be reestablished (11).
TECHNIQUE
INCISION PLACEMENT AND TISSUE HANDLING
Several considerations must be addressed when determining the appropriate incision placement for the definitive amputation. First and foremost, all diseased tissue must be removed until the remaining surface appears to be clear and viable (10). When able, the weight-bearing areas should be covered with healthy skin that is specifically adapted for weight-bearing (11). The surgeon should plan incisions parallel to the relaxed skin tension lines if possible. Anatomic dissection and proper tissue handling is essential in preventing wound complications (18).
HEMOSTASIS
A tourniquet can be placed on the limb prophylactically and used on a discretionary basis (1). The use of a tourniquet up until the wound is closed has not been shown to have a detrimental effect on healing following surgery (10). Blood vessels should be cauterized or ligated; however, efforts should be made to limit the amount of absorbable suture utilized in the wound. Frequent lavage with cool saline and positioning the patient in a slight Trendelenburg may assist with hemostasis (18).
CARTILAGE REMOVAL
Amputation surgeons differ on their opinions regarding removing cartilage at the level of amputation versus leaving it intact. Those that choose to remove the cartilage claim getting down to bleeding surface of bone leads to a significant improvement in tissue healing (17). Definitive reasons for removal of cartilage include the presence of gout, dysvascular cartilage, or infection. Those that prefer leaving the cartilage intact claim the cartilage and subchondral bone serve as a barrier to infection. Another cited advantage to leaving the cartilage intact is that it allows shear mobility of the soft tissues over the bone, and breakdown of the tissue is less apt to occur (10).
WOUND CLOSURE
If a wound is closed after débridement, a nonreactive material such as monofilament suture should be used, with no tension
placed on the wound edges (18). The surgeon should avoid inversion of the skin margins to help prevent delayed healing or wound dehiscence. The optimal skin closure should be end-to-end skin closure with direct approximation of the skin margins of the wound and slight eversion of the skin margins. Sutures that are too tight and too few in number are also potential causes of delayed healing that may lead to wound dehiscence (18).
placed on the wound edges (18). The surgeon should avoid inversion of the skin margins to help prevent delayed healing or wound dehiscence. The optimal skin closure should be end-to-end skin closure with direct approximation of the skin margins of the wound and slight eversion of the skin margins. Sutures that are too tight and too few in number are also potential causes of delayed healing that may lead to wound dehiscence (18).
In partial foot amputations, the foot may need to be débrided multiple times prior to wound closure until the wound is clean. Once the surgeon is convinced the wound is clean, a delayed primary closure can be performed. When in doubt, the surgeon should leave the wound open (18). Delayed primary closure significantly shortens healing time that otherwise without closure may take many months of granulation and wound contracture. Delayed primary closures can often be done under local anesthetic. The cost and potential morbidity of an additional procedure can be significantly offset by the reduction in healing time. Even if the wound cannot be closed entirely, converting a large open wound to a small open wound offers the same benefit (10).
Split-thickness skin grafting may be used to complete wound coverage or decrease tension on the wound closure while maintaining limb length. When placed over soft tissue, these grafts can function quite well; however, often these skin-grafted areas do not tolerate the axial and shear stresses within the prosthesis and may require removal at a later date (1).
POSTOPERATIVE MANAGEMENT
With any foot amputation, it is very important that meticulous attention is given to the initial and subsequent postoperative bandages that are applied after the amputation. It is the authors’ experience that many complications involving the operative wound as well as new wounds are caused when the initial dressing or subsequent dressing changes are not applied carefully. Improper bandaging may significantly increase healing time as well as produce severely delayed or nonhealing wounds over poorly vascularized areas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree