All-Inside Double-Bundle Anterior Cruciate Ligament Reconstruction
Patrick A. Smith
All-inside anterior cruciate ligament (ACL) reconstruction refers to a specialized technique where blind sockets as opposed to full tunnels are made for graft placement with the approach on the tibia representing the major change relative to traditional ACL reconstruction. It has been described as a “no-tunnel” procedure (1, 2). Touted patient advantages include less postoperative pain, cosmesis, easier rehabilitation particularly relative to return of motion, and less postoperative supervised physical therapy.
This technique is based on use of the proprietary RetroCutter (Arthrex) for creation of the tibial socket. The femoral socket is generally created through the anteromedial (AM) portal, but can easily be made from a lateral approach through the proprietary FlipCutter (Arthrex). Fixation options are flexible on the femoral side with Retro-Screw (Arthrex) aperture fixation classically utilized on the tibia. Initially described for single-bundle ACL reconstruction (1), the all-inside approach is easily adaptable for double-bundle ACL reconstruction with the “all-inside × 2” procedure to be described in this chapter (2). All-inside is also a very useful method for revision ACL reconstruction. The all-inside technique is unique and a valuable surgical skill to have as an ACL surgeon, particularly relative to potential patient advantages due to the very nature of it being such a minimally invasive approach.
CLINICAL EVALUATION
There is never any substitute for a thorough history and physical examination. The classic history of an acute noncontact deceleration or twisting mechanism of injury with or without a “pop” and joint swelling with limitation of knee extension should be considered an ACL tear until proven otherwise, especially in a young female basketball or soccer player. Chronically, patients present with the complaint of giving way instability, typically related to their sports activity usually associated with some joint swelling.
From the examination standpoint, the Lachman test is easy to perform even with an acute injury, and is very sensitive for an ACL tear. However, the key is the presence of the pivot shift diagnostic for rotational instability of the knee, which is the primary indication for surgical reconstruction. Acutely, the Losee test is better tolerated by the patient.
Plain X-rays are very important and represent the simplest and most cost-effective ancillary imaging study to rule out any associated bony pathology. MRI is helpful acutely to assess for significant bone bruising, which would influence the need for protective weight bearing, and also is helpful delineating associated medial and/or lateral ligamentous injury. Meniscal integrity can be assessed on MRI although certainly MRI is far from perfect in that regard. In the chronic setting, MRI is not as important as X-ray.
TREATMENT DECISION MAKING
The decision for ACL reconstruction is made with considerable patient input. First and foremost, if a patient is active in a sport where rotational joint loads are common, reconstruction should be done. If a patient experiences giving way instability with activities of daily living even though they are not active in sports, surgery is appropriate, especially if one has an associated meniscus tear. Surgical rationale is to prevent future instability, and thereby both improve one functionally and prevent abnormal shear stresses on the joint to preserve the menisci and joint surfaces. There really is no age limit for ACL reconstruction, as long as X-rays show no advanced degenerative change. The patient must be committed and motivated for the necessary postoperative rehabilitation program. Plus, the patient needs to also accept the initial restraint necessary before returning to sports activity to minimize stress on their ACL graft until muscle mass is built up sufficiently, and adequate time has passed to allow for biologic graft remodeling and incorporation.
If one has minimal laxity relative to just a pivot glide on examination and does not participate in cutting/pivoting sports activity, conservative treatment emphasizing rehabilitation for muscle strengthening about the involved
knee and hip with use of a functional ACL brace for any stressful activity can sometimes be successful. Generally, in this scenario, a partial ACL tear is present, but this is not that common.
knee and hip with use of a functional ACL brace for any stressful activity can sometimes be successful. Generally, in this scenario, a partial ACL tear is present, but this is not that common.
Relative to surgical timing, there is no “set” time as individuals react to this injury differently, but rather my decision to proceed with surgery is based on examination criteria of full knee extension with a good quadriceps contraction, minimal effusion, and flexion >120°. In the acute ACL tear setting, initiation of “prehab” with the help of a physical therapist to get the knee ready for surgery can be very helpful.
SURGICAL TECHNIQUES—SINGLE- VERSUS DOUBLE-BUNDLE ACL RECONSTRUCTION
Single-bundle reconstruction drilling the femoral socket transtibially can increase the potential for tunnel mismatch and “vertical graft” placement, which less than optimally controls the pivot shift. Another concern is long-term follow-up studies have shown a rather high incidence of arthritic development after ACL reconstruction (3).
Multiple anatomic dissection studies have shown the presence of distinct anteromedial (AM) and posterolateral (PL) bundles of the ACL, and biomechanical studies have shown different tensioning patterns for these main bundles (4, 5). Experimentally, it has also been shown the double-bundle construct better restores ACL biomechanics, particularly rotational stability compared with single-bundle reconstruction (6). The questions to be answered with the double-bundle approach is whether it will both improve overall joint stability and minimize later arthritic development to justify the increased complexity of the procedure. Stability with two grafts should be potentially enhanced by the overall strength of the construct primarily due to increased surface area for tendon to bone healing (7). Theoretically with the inherent different tensioning patterns with the two bundles, there may be load sharing with the double-bundle construct to both optimize knee kinematics and graft healing/incorporation in the process. So far, short-term clinical studies have shown slight improvement over single-bundle comparisons with KT-1000 testing but not with patient outcomes (8, 9). Another variable is the recent change with single-bundle reconstruction actually stimulated by the interest in double bundle moving the femoral socket position more laterally on the femur with a central tibial tunnel to try and “capture” part of both the AM and the PL bundle origins and insertions, which may improve single-bundle outcomes. One of the problems compromising true objective stability evaluation of double versus single bundle is the lack of a rotational stability testing device. Nonetheless, double-bundle ACL reconstruction has merit as a technique to possibly better patient outcomes through restoration of more normal knee anatomy and kinematics.
Double-bundle ACL reconstruction has been described numerous ways. Most commonly it is done through two full tibial tunnels with two femoral sockets sometimes created transtibially. Others have chosen to “manipulate” a single-bundle ACL reconstruction into a double-bundle construct by splitting the graft generally with the fixation device used on the femur or tibia. The all-inside double-bundle technique is uniquely different done through two femoral sockets and two tibial sockets, and has several potential advantages beginning with the patient relative to ease of recovery, as well as for the surgeon from the technical standpoint in performing the procedure, and also possibly biologically in terms of graft healing and incorporation.
ALL-INSIDE RATIONALE/ADVANTAGES
Patient advantages with the all-inside approach relate particularly to it being a minimally invasive “no-tunnel” technique because sockets are also created on the tibial side reaming from inside the joint through use of the RetroCutter (1, 2). Correspondingly, this necessitates just a small tibial incision for placement of the 3-mm RetroCutter guide pin resulting in less dissection over the sensitive periosteum of the proximal tibia helping to minimize postoperative discomfort. Preliminary data from a prospective level one randomized study comparing postoperative pain with a full-tibial tunnel versus an all-inside tibial socket with soft tissue allograft ACL reconstructions has shown significantly less pain with VAS grading from the first postoperative day through two years for the all-inside cohort compared with the endoscopic group. Mean percocet use the first week after surgery was 27.9 for the all-inside patients and 33.2 for the endoscopic patients. (Lubowitz, Smith and Schwartzberg, unpublished study.) Another patient advantage is that clinically, patients with all-inside ACL reconstructions either single or double bundle, seem to get back range of motion much quicker after surgery and need less supervised physical therapy.
From the surgeon perspective, creating tibial sockets with the RetroCutter allows optimal placement on the tibia without any guesswork as to position, compared with any outside-in tunnel technique requiring an aiming guide, which could visually be less precise, and this is particularly important when the tibial footprint is small. More importantly, the retrograde cut tibial socket has been shown by CT analysis to have much less aperture bone disruption than an outside-in antegrade full tunnel, which thereby minimizes the chance for coalescence or fracturing between the two tibial sockets versus two full tunnels (10). This risk is even made less with use of aperture RetroScrew fixation beginning with the PL bundle, which further buttresses the PL tibial socket from the AM tibial socket. Also, the retrograde sockets have smoother walls to enhance fixation stability and possibly graft healing and incorporation. Finally,
follow-up X-rays at 1 year following all-inside single-bundle ACL reconstruction have not shown tunnel widening even with use of allografts, which likely is attributable to less synovial egress with the sockets as opposed to traditional full tunnels, especially on the tibial side where RetroScrew aperture fixation also helps to seal the joint (11).
follow-up X-rays at 1 year following all-inside single-bundle ACL reconstruction have not shown tunnel widening even with use of allografts, which likely is attributable to less synovial egress with the sockets as opposed to traditional full tunnels, especially on the tibial side where RetroScrew aperture fixation also helps to seal the joint (11).
Another surgeon advantage with the all-inside approach relates to drilling the femoral sockets through the AM portal, avoiding the inherent problems with transtibial femoral drilling (12, 13). This serves to optimize femoral socket placement especially critical with double-bundle reconstruction. Furthermore, the versatility of the all-inside technique is exemplified by the ease of performing a “two-incision” equivalent procedure by drilling the femoral sockets from “outside-in.” Specifically, the new FlipCutter device, which is a guide pin that converts after placement to a reamer, can easily be drilled from the lateral cortex of the femur into the notch area via an aiming guide to create the either AM or PL femoral sockets, if one prefers that particular approach. Also, the FlipCutter has a tibial guide, so it can be used to drill the tibial sockets as well, comparable to the RetroCutter.
Additionally, the all-inside approach is very versatile relative to the issues of graft choice, femoral and tibial fixation, and graft tensioning, as surgeons have different preferences and beliefs as to what works best for them. Therefore, the all-inside double-bundle procedure can be customized in many ways for the surgeon, but yet still maintain its most important quality relative to being minimally invasive for the patient.
Biologically, there is the theoretic possibility that the all-Inside sockets especially on the tibial side may trap more hematoma and potential growth factors after surgery to help with graft incorporation compared with full tunnels. The analogy would be that of a “potted plant” referring to the graft end surrounded in the dead end bone socket. Plus, the all-inside approach is inherently bone preserving, which is an innate advantage with surgery about the knee joint.
GRAFT CHOICE FOR ALL-INSIDE DOUBLE BUNDLE
All-inside double-bundle ACL reconstruction is very flexible relative to graft choice. One option is for autogenous hamstring autografts harvested through a mini-popliteal incision initially described by Franz and Ulbrich (14). This is a very minimally invasive and cosmetic approach. One advantage of all-inside ACL reconstruction is the grafts are not as long, so if the semitendinosis harvested length is approximately 280 mm, it can be used for both grafts, which are doubled. If the semitendinosis is not that long, then the gracilis is harvested easily through the mini-popliteal approach. Usually the semitendinosis is 6 to 7 mm in diameter doubled, and is used for the AM bundle with the gracilis 5 to 6 mm doubled, for the PL bundle.
My graft choice for the contact athlete is a bit different. Here for the AM bundle, I use a middle third patellar tendon graft harvested with bone only off the tibia, peeling the patellar tendon off the patella for length. The bone plug is 8 × 20 mm and the tendon width is 10 to 11 mm. A doubled autogenous semitendinosis is used for the PL bundle and usually is 6 to 7 mm in diameter.
Allograft tissue can also be utilized. Two soft tissue grafts generally 6 to 7 mm doubled each work well, or a patellar tendon allograft with one soft tissue allograft is a good combination. I have also done “hybrid” reconstructions where I utilize usually a patellar tendon allograft for the AM bundle with an autogenous semitendinosis for the PL bundle, especially for revision cases.
FIXATION OPTIONS ALL-INSIDE DOUBLE BUNDLE
Fixation options are flexible on the femoral side, and depend in part on graft choice as well as surgeon preference. I favor TightRope (Arthrex) suspensory femoral fixation when I use either autogenous hamstring or soft tissue allografts. The TightRope device consists of a 12 × 3 mm button with an attached blue # 2 FiberWire (Arthrex) passing suture and a special white # 2 FiberWire shortening suture. The special shortening suture is actually a continuous #2 FiberWire suture spliced on itself creating a loop that tightens around the graft for “fingertrap” fixation providing four points of fixation as the shortening sutures are tightened “hoisting” the graft in the socket against the button on the femoral cortex (Fig. 73.1). I prefer the RT or reverse tension TightRope with the shortening sutures extraarticular on the femoral side where the button is flipped, as opposed to a regular TightRope where the shortening sutures are pulled intraarticularly. Strength of fixation is excellent, and since the length of both the AM and particularly the PL sockets are shorter by drilling them more transversely through the AM portal, the button fixation is closer to the end of the graft. Therefore, the so-called “bungee” effect should be less than would be the case when suspensory ends up far from the joint line well away from the end of the graft. Length of the graft in the femoral socket is not an issue with the AM bundle as this intraosseous distance is always a decent length-approximately 40 to 50 mm. However, the PL intraosseous distance can be short approximately 30 to 35 mm due to its position, which in turn limits how deep the socket can be drilled, and yet still preserve the lateral cortex for TightRope button fixation. Therefore, I always ensure that there is at least 15 mm of graft in the femoral socket with experimental evidence suggesting that should be adequate for bundle strength (15). If though the PL socket is too short to accommodate TightRope fixation relative to potentially not enough graft in the socket, I will then fixate with a bioabsorbable interference screw. Conceivably, one could choose to use interference screw fixation for the both AM and PL bundles on the femoral side with soft tissue grafts. In contact athletes, an absorbable interference screw is used to fix the patellar bone plug on the femur for the AM bundle, and a Tightrope for the semitendinosis for the PL bundle.
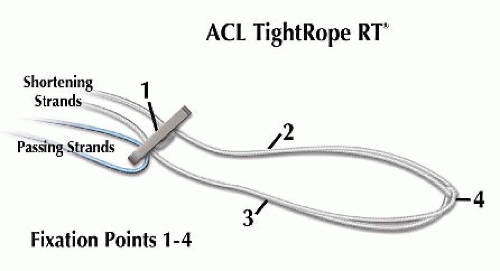 FIGURE 73.1. Schematic of ACL TightRope RT used for suspensory femoral fixation of AM and PL bundle soft tissue grafts, illustrating four points of fixation from the loop. |
On the tibial side, Retroscrew aperture fixation is preferred, but tying the graft sutures over a titanium button here for suspensory fixation can be done with use of a tensioning device.
SURGICAL TECHNIQUE
All-Inside × 2
The procedure is termed “all-inside × 2” to reflect the basic approach of doing an all-inside single-bundle reconstruction for the PL bundle, and then repeating the exact same steps for AM bundle reconstruction. So once one has mastered all-inside single-bundle reconstruction particularly with use of the RetroCutter, “all-inside × 2” is a reasonable progression to a double-bundle construct.
As an overview, both femoral sockets are first prepared drilling through the AM portal in hyperflexion. Next, the PL tibial socket is created with the RetroCutter. The PL bundle is passed and fixed on the femur, and then secured on the tibia with a RetroScrew at the aperture in full extension. Next, the AM tibial socket is created with the RetroCutter. The AM bundle is then passed into the femur and fixed on the tibial side using a RetroScrew at approximately 30° of flexion.
Notably, this sequence of passing and fixing the PL bundle first has been shown recently biomechanically to be superior than creating both tibial sockets, and then passing and fixing the PL bundle (16). This validates what has been done clinically with the “all-inside × 2” approach the past couple of years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








