Chapter 34 All-Inside Arthroscopic Meniscal Repair
The concept of meniscal repair was first described by Annandale in 1885.5 It is well established that the meniscus contributes several key functions to the knee, including joint stability,38 shock absorption and load transmission,17 proprioception,20 and articular cartilage nutrition.24 Furthermore, the long-term consequences of total meniscectomy include the predictable development of degenerative joint changes.2,3,18,23 Meniscal repair is therefore preferred to meniscectomy whenever feasible.
Indications for All-Inside Meniscal Repair
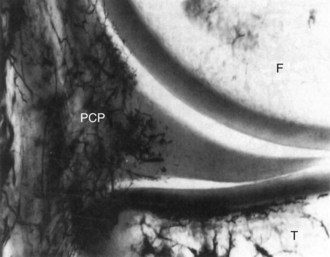
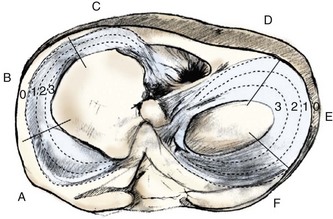
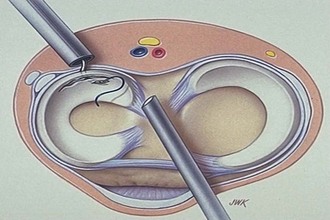
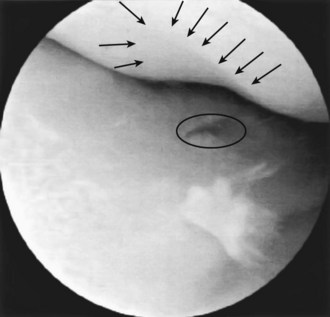
The basic prerequisites for inside-out meniscal repairs also apply to all-inside repairs. Not all meniscal tears are amenable to repair and several factors must be considered to determine repair suitability and healing potential. Although magnetic resonance imaging (MRI) may aid in predicting repair versus meniscectomy, the final determination of repair suitability is often made during arthroscopy. Meniscal tissue is relatively avascular. Only the peripheral 10% to 30% of the meniscus is vascularized, supplied by the medial and lateral genicular arteries6 (Fig. 34-1). The remaining meniscus receives its nutrition through synovial fluid diffusion. The popliteal hiatus also creates a relatively hypovascular area in the posterior lateral meniscus. DeHaven19 classified tears in the peripheral 3 mm as vascular (also referred to as the red-red zone), those more than 5 mm from the meniscocapsular junction as avascular (white-white zone), and those in between as variable (red-white zone). Based on the blood supply pattern, tears in the vascular periphery of the meniscus have the best ability to heal, whereas tears in the central white-white zone demonstrate poorer healing rates and are less amenable to repair31 (Fig. 34-2).
In addition to location, meniscal tear orientation and complexity must also be considered. Longitudinal vertical tears, bucket handle tears, and meniscocapsular separations are most amenable to repair (Fig. 34-3). Although radial tears were previously a contraindication to repair, some of these tears may also be repaired successfully, but this remains somewhat controversial. Conversely, tears with increasing complexity may be better managed with partial meniscectomy. These include degenerative tears and tears with horizontal cleavage planes or multiple flaps.48 Oblique undersurface tears can also be problematic because they often extend from the vascular to avascular zone.
Patient factors also play a substantial role in determining appropriate indications for meniscal repair. It is well known that meniscal repair is more successful in the setting of concurrent anterior cruciate ligament (ACL) reconstruction. All-inside techniques may be particularly indicated in this setting, as opposed to isolated repairs. Furthermore, meniscal healing rates are typically lower in an ACL-deficient knee,29 and repair may be contraindicated if the ACL is not also reconstructed. Patient age and tear chronicity are other important variables. Older patients with chronic degenerative tears are better served with partial meniscectomy. Finally, meniscal repair requires a patient willing to comply with a prolonged rehabilitation course as opposed to resection.
Techniques
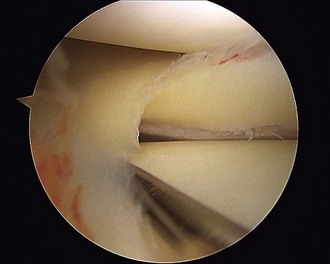
All-inside repairs were first introduced in 1991 and have subsequently been developed in successive generations of improvements in device and technique.53 With each of these devices, an intact meniscal rim is required to anchor the repair device. Therefore, meniscocapsular separations are preferentially repaired with an alternate technique (Fig. 34-4). Anterior horn tears are also a relative contraindication because of difficulty in accessing the tear with these techniques.
First-Generation All-Inside Repairs
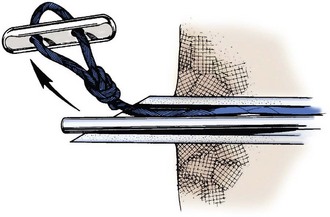
The first generation of all-inside repairs was described by Morgan43 in 1991 and used curved suture hooks through accessory posterior portals to pass sutures across the tear. Sutures were then retrieved and tied arthroscopically (Fig. 34-5). The technique was technically demanding and continued to place the neurovascular structures at risk. It was subsequently abandoned with the development of second-generation repairs.
Second-Generation All-Inside Repairs
The second generation of all-inside meniscal repairs introduced the concept of technique-specific devices placed across the tear and anchored peripherally. The prototype of this generation was the T-Fix (Smith & Nephew, Andover, Mass; Fig. 34-6). The T-Fix consisted of a polyethylene bar with attached no. 2-0 braided polyester suture that was deployed through a sharp needle or cannula to capture the peripheral meniscus or capsule. Adjacent sutures were then secured with arthroscopic knots pushed onto the meniscal surface. This generation was a significant advance because meniscal repair was now achievable through standard anterior arthroscopic portals without the need for accessory incisions and with minimal risk to neurovascular structures when performed properly. The device confirmed that it was possible and safe to repair the meniscus by deploying an anchor across the tear and into the periphery of the meniscus and capsule. However, the need for arthroscopic knots, with potential chondral abrasion and the inability to tension the knots after placement, were technical drawbacks of the device. Early results were encouraging, with short-term success rates of 80% to 90%.11,22 Despite the early results, the desire for a simpler device with improved compression across the meniscal repair led to the development of third-generation devices.
Third-Generation All-Inside Repairs
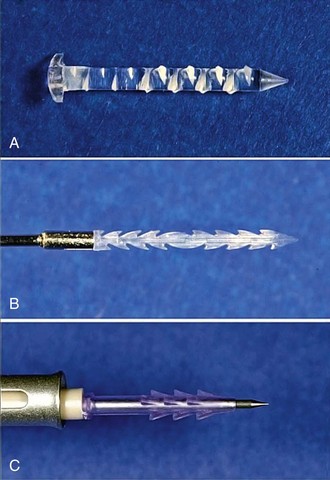
The third generation consisted of the development of bioabsorbable meniscal repair devices including arrows, screws, darts, and staples (Fig. 34-7). Most of these devices are composed of the rigid poly-L-lactic-acid (PLLA), which retains its strength for up to 12 months and requires 2 to 3 years or longer to resorb completely. The most commonly used device was the Meniscal Arrow (ConMed Linvatec, Largo, Fla) because of its ease of insertion and early success rates. The current version of the meniscal arrow (Contour Meniscus Arrow and ConMed Linvatec, Largo, Fla) has a low-profile head and is barbed along the entire length of the implant shaft to improve fixation strength. It is composed of a faster resorbing self-reinforced copolymer, 80L/20D,L PLA, which retains its strength for up to 24 weeks and then gradually resorbs. When seating the arrow across the meniscal tear, it is important to indent the head of the arrow into the meniscus to reduce the risk of chondral damage. One prospective, randomized study used second-look arthroscopy to assess healing rates of 91% with the arrow versus 75% with horizontal mattress suture repairs.1 Unfortunately, these results did not prove durable. Another study with the Meniscus Arrow revealed a 90.6% success rate at 2 years in patients undergoing concurrent ACL reconstruction.27 However, these results deteriorated significantly at longer term follow-up, with a success rate of only 71.4% at 6 years in the same group of patients.37 Other studies have documented similar deterioration of results.21,49 Kurzweil and colleagues36 reported an overall failure rate of 28% with the Meniscus Arrow at average follow-up of 54 months. Furthermore, in isolated meniscal repairs without concurrent ACL reconstruction, the failure rate was a striking 42%. Yet another study reported a failure rate of 41% at 4.7 years.26
Numerous device-specific complications have also been reported with the Meniscus Arrow, including transient synovitis, inflammatory reaction, cyst formation, device failure, device migration, and chondral damage (Fig. 34-8).*
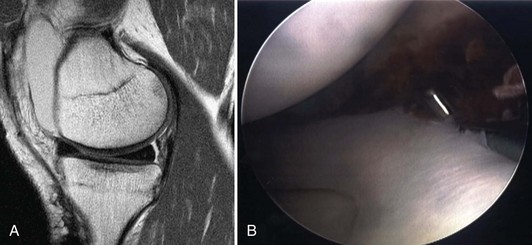
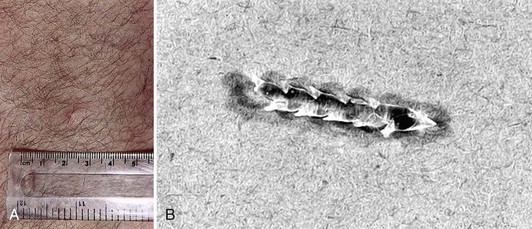
Chondral damage is a potential complication with any of the rigid third-generation devices (Fig. 34-9). If these devices are placed too proudly or loosen or migrate prior to dissolving, significant chondral damage can result, which often consists of grooving of the adjacent femoral condyle.36 Because of the deterioration of results and numerous complications, the rigid third-generation devices have generally fallen out of favor.
Fourth-Generation All-Inside Repairs
The FasT-Fix, first introduced in 2001, is composed of two 5-mm suture anchors connected by a no. 0 nonabsorbable polyester suture with a pretied slip knot (Fig. 34-10). A newer version of the FasT-Fix (Ultra FasT-Fix) consists of polyetheretherketone (PEEK) anchors with ultra–high-molecular-weight polyethylene (UHMWPE) sutures (Ultrabraid) to improve strength and ease of use. It is also available with absorbable PLLA anchors. A depth-limiting sleeve on the inserter may be precut to any desired length, with 12 to 13 mm generally considered a sufficient length that is also safe to the neurovascular structures.42 The curved or straight inserter, with both anchors loaded, is introduced into the joint and advanced across the tear. After deploying the first anchor, the needle inserter is withdrawn from the meniscus, but maintained in the joint. The second anchor is advanced to the tip of the inserter, which is then advanced across the meniscus a second time and deployed. The anchors and resultant suture bridge may be placed in a vertical or horizontal mattress configuration, simulating inside-out suture repairs. The pretied slip knot is advanced with a push-pull technique to apply variable compression across the tear. The suture is then cut or, alternatively, may be left in place until all devices are placed to allow for retensioning. One of the primary advantages of the FasT-Fix is the ability to place a suture-based device in a vertical mattress configuration (Fig. 34-11). Unfortunately, the device can be difficult to place posteriorly and misfires, device breakage, anchor pull-out, and tangled sutures are not uncommon (Fig. 34-12).
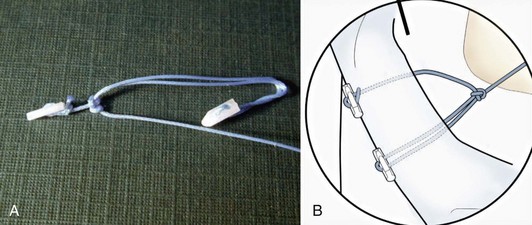
Figure 34-10 The FasT-Fix all-inside meniscal repair device is composed of two suture anchors connected by a pretied slip knot.
(A from Barber FA, Schroeder FA, Oro FB, et al: FasT-Fix meniscal repair: mid-term results. Arthroscopy 24:1342–1348, 2008; B from Smith & Nephew: Meniscal repair with FasT-fix suture system. Smith & Nephew Endoscopy, Andover, Mass, 2008.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree