All-Inside Anterior Cruciate Ligament Reconstruction: Graft-Link
James H. Lubowitz
Understanding “all-inside” (AI) anterior cruciate ligament (ACL) reconstruction or “Graft-Link” requires historical tribute to earlier surgical pioneers.
Historically, surgical treatment of rupture of the ACL has evolved from open repair, to open reconstruction (with or without augmentation), to “2-incision” technique, to arthroscopic or endoscopic “1-incision” technique, and as described in this chapter, to AI ACL technique. AI ACL reconstruction was first described in 1995 by Morgan et al. (1, 2) Unfortunately, the Morgan technique was “often associated with technical difficulties (3)” or, in the words of Morgan himself, “was technically demanding, which limited its popularity (4).” The specific technical challenge involved creating a tibial socket through a high anteromedial (AM) portal, a technique unfamiliar to most practicing arthroscopic surgeons.
The solution, a description of AI ACL using a more familiar transtibial approach, was published by the chapter author in 2006 (5). However, AI ACL technique has continued to evolve, and in 2011, Lubowitz, Ahmad, and Anderson published, “All-inside anterior cruciate ligament Graft-Link technique: second-generation, no-incision anterior cruciate ligament reconstruction (6).”
The reason for the evolution is manifold, but primarily a result of better understanding of ACL anatomy, as well as evolution of surgical instruments and graft fixation implants.
With regard to anatomy, as described by Lubowitz et al. (6), “Transtibial technique for creating the ACL femoral socket is known to be a risk factor for anatomically mismatched posterior tibial tunnel placement and high AM femoral tunnel placement (7, 8, 9, 10 and 11). Thus … some surgeons made the transition to the AM portal technique for creating the ACL femoral tunnel (8, 10, 12, 13, 14, 15, 16, 17, 18, 19, 20 and 21), yet this technique is associated with potential pitfalls (8, 12, 13, 16, 17, 18, 19, 20, 21, 22 and 23). Therefore, in 2011, while AM portal technique is anatomic (and may be used as an alternative for AI ACL Graft-Link technique), we recommend as an alternative, creating the ACL femoral socket using outside-in technique (7, 9, 18, 24, 25, 26 and 27).”
AI ACL ADVANTAGES
Outside-in technique for creating the ACL femoral socket fell out of favor because the requirement for a lateral, distal, femoral, muscle splitting dissection results in a more invasive “2-incision” technique (7, 8, 24, 27). However, new technology, specifically narrow diameter guide pins that may be transformed into retrograde drills,(18, 25) allows “no-incision” outside-in techniques for creating the ACL femoral socket. Advantages of outside-in technique for creating the ACL femoral socket are that it is performed in the comfortable and familiar 90° knee flexion position (unlike AM portal technique); it is unconstrained, allowing independent, anatomic positioning of the femoral socket (unlike transtibial technique for drilling the femoral socket); and it may result in a longer socket (compared with AM portal technique) (18). In addition, outside-in drilling allows measurement of femoral interosseous distance prior to socket creation, using standard, outside-in femoral guides and guide pin sleeves. Premeasurement is a safety feature of the outside-in technique because a short distance may require that less graft tissue is contained within the femoral socket (28).
In addition to retrograde drilling pins, two additional technical developments simplify AI ACL reconstruction. The first development represents an evolution of cortical suspensory fixation button devices. First-generation cortical suspensory fixation buttons have fixed length graft loops, whereas second-generation cortical suspensory fixation buttons have graft loops that are adjustable in length, such that after the button flips and becomes fixed on the cortex, the graft loop may be tightened, pulling the graft in to the socket in a manner that completely fills the socket with graft substance. Furthermore, first-generation cortical suspensory fixation buttons were designed for femoral fixation, whereas second-generation adjustable graft loop buttons are effective for tibial (as well as femoral) fixation. Finally, second-generation adjustable graft loop buttons are unique in that when the graft loop is tightened, graft tension increases. Thus, for the first time, ACL surgeons may increase graft tension after the graft is fixed.
The second technical development that simplifies AI ACL reconstruction is the use of cannulas. Arthroscopic shoulder and hip surgeons have long understood the importance of cannulas for maintaining portals and preventing soft tissue from becoming intertwined in sutures. First, we recommend a cannula in the AM arthroscopic instrumentation portal to prevent soft tissue interposition. Second, we introduce a unique guide pin sleeve, which transforms into a cannula and maintains access to the narrow diameter guide pin tracks used to create AI sockets, allowing suture passage, and later graft passage, after ACL socket retroconstruction (6).
CLINICAL EVALUATION
With regard to patient history, physical evaluation, imaging, classification and decision-making algorithms, AI ACL Graft-Link is not unique. Thus, the focus of this chapter will be on surgical technique, as described below. Of course, with any new surgical technique, patient education and appropriate informed consent with regard to risks, benefits, alternatives, and surgical and nonsurgical treatment options are of particular importance.
TREATMENT
With regard to the indications for nonoperative versus operative treatment of ACL rupture and with regard to the timing of ACL surgery, AI ACL Graft-Link is not unique. Thus, the focus of this chapter will be on the surgical technique, as described below.
SURGICAL TECHNIQUE
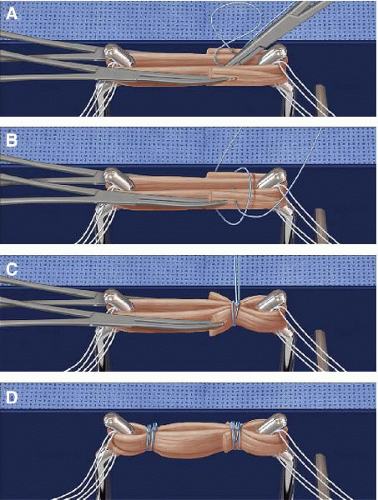
No-tunnel, AI socket ACL reconstruction using Graft-Link requires learning new graft preparation, socket creation, and graft fixation techniques. Graft preparation requires consideration of no-incision cosmesis when selecting graft sourceensuring that graft length (GL) is less than the sum of socket lengths (SLs) plus intra-articular graft distance so that the graft will not bottom out in the sockets during final graft tensioning, and learning the graft-link preparation technique. Femoral and tibial socket creation is with second-generation retrodrilling guide pins. Femoral and tibial fixation is with second-generation cortical suspensory fixation devices with pull sutures tensioning an adjustable graft loop.
Special Equipment
Graft Preparation Station and High Strength Suture
High strength sutures (Fiberwire, Arthrex Inc., Naples, FL) secure the graft in a loop.
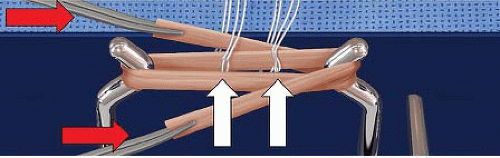
The loop is sewn in linkage with an ACL femoral tightrope adjustable graft loop (Arthrex) and an ACL tibial reverse tightrope adjustable graft loop (Figs. 72.1 and 72.2).
A graft preparation station facilitates suturing the graft at a specific length (approximately 65 mm). After suturing, pretensioning of the graft construct results in an ultimate GL of approximately 75 mm (Fig. 72.3).
Flipcutter
Flipcutter (Arthrex) is a second-generation retrograde drill. The Flipcutter guide pin becomes a retrograde drill by flipping a switch on the pin handle. Then, after socket creation with clockwise drilling and retrograde pressure, the Flipcutter retrograde drill is switched back into a guide pin and removed.
The Flipcutter is 3.5 mm in diameter allowing femoral (Figs. 72.4 and 72.5) and tibial socket (Figs. 72.6 and 72.7) creation through portal-sized “stab-incisions” for cosmetic AI technique.
Flipcutter Guide Pin Sleeve
Flipcutter is drilled through a unique graduated-tip guide pin sleeve. The tip of the drill sleeve is “stepped,” with a 7-mm length narrow tip. The tip of the cannula is tapped into the distal lateral femoral cortex over the Flipcutter, and subsequently, into the proximal AM tibial metaphysis. When the tip is advanced to the 7-mm mark, it reaches palpable resistance to further tip advancement, because during the retrograde socket formation, the Flipcutter is withdrawn until it stops at the tip of the metal guide pin sleeve. In addition, laser marks on the guide pin sleeve allow observation of the 7-mm tap in distance. The 7-mm sleeve protects and preserves a 7-mm cortical bridge (resulting in sockets, not full tunnels on both the femoral and tibial graft sites). Cortical preservation is required for cortical suspensory fixation using a second-generation adjustable graft loop (Figs. 72.4 to 72.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree