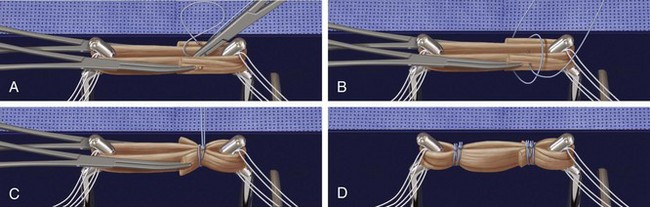
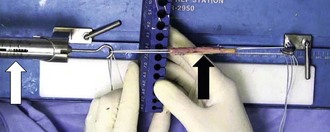
Chapter 79 An old orthopedic adage states, “The techniques that I use in the operating room now are different from the techniques I learned during my training.”1 Five years ago, all-inside ACL reconstruction using the no-incision technique involved use of transtibial drilling of the ACL femoral socket.2 Unfortunately, the transtibial technique for creating the ACL femoral socket is known to be a risk factor for anatomically mismatched posterior tibial tunnel placement and high anteromedial (AM) femoral tunnel placement.3–7 As a result, over the last 5 years some surgeons have transitioned to the AM portal technique for creating the ACL femoral tunnel.4,6,8,9–18 This technique, however, is not without associated potential pitfalls.4,8,9,12,13,15,16,19,20 In response to these concerns, in 2011 we recommended creating the ACL femoral socket with use of an outside-in technique as an alternative to the anatomic AM portal technique.3,5,14,15,21–23 Historically, the outside-in technique for creating the ACL femoral socket fell out of favor because of the requirement for two-incision technique involving a lateral muscle-splitting dissection at the distal femur.3,4,21,23 Recently, however, new technology including narrow-diameter guide pins that are transformed into retrograde drills14,15 allows for a “no-incision” outside-in technique to create the ACL femoral socket. The advantages of an outside-in technique for creating the femoral socket include the ability of the surgeon to operate in the comfortable and familiar position of 90 degrees of knee flexion (unlike the AM portal technique), independent placement the femoral socket in an anatomic position unconstrained from drilling through the tibial tunnel, and drilling of a longer socket than with the AM portal technique.15 In addition, outside-in drilling allows for measurement of the femoral interosseous distance before socket creation with use of standard, outside-in femoral guides and guide pin sleeves. Premeasurement of the socket depth is a safety feature of the outside-in technique because a short tunnel may necessitate that less graft tissue be contained within the femoral socket.24 The second important technical development that simplifies all-inside ACL reconstruction is the use of cannulas. Arthroscopic shoulder and hip surgeons have long understood the importance of cannulas for maintaining portals and preventing soft tissue from becoming intertwined in sutures. As a result, we recommend the use of a cannula in the AM arthroscopic instrumentation portal to prevent soft tissue interposition. Furthermore, we introduced a unique guide pin sleeve that transforms into a cannula to maintain access to the narrow-diameter guide pin tracks used to create all-inside sockets, allowing for suture passage and for later graft passage after ACL socket retroconstruction.1 • Graft preparation station and high-strength suture. High-strength sutures (FiberWire, Arthrex, Naples, FL) secure the graft in a loop. The loop is sewn in linkage with an ACL femoral TightRope adjustable graft loop (Arthrex) and with an ACL tibial reverse TightRope adjustable graft loop (Arthrex; Figs. 79-1 and 79-2). A graft preparation station facilitates suturing of the graft at a specific length (approximately 65 mm). After suturing, pretensioning of the graft construct results in an ultimate graft length of approximately 75 mm (Fig. 79-3). • FlipCutter. The FlipCutter (Arthrex) is a second-generation retrograde drill. The FlipCutter guide pin becomes a retrograde drill when a switch on the pin handle is flipped. The socket is created with clockwise drilling and retrograde pressure. After use, the FlipCutter retrograde drill is switched back into a guide pin and removed. The FlipCutter is 3.5 mm in diameter to allow for creation of the femoral (Figs. 79-4 and 79-5) and tibial socket (Figs. 79-6 and 79-7) through portal-sized stab incisions for a cosmetic all-inside technique.
All-Inside Anterior Cruciate Ligament GraftLink Technique
Second-Generation, No-Incision Anterior Cruciate Ligament Reconstruction
Surgical Technique
Special Equipment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


All-Inside Anterior Cruciate Ligament GraftLink Technique: Second-Generation, No-Incision Anterior Cruciate Ligament Reconstruction