Fig. 46.1
AP (a) radiograph of infected total knee, lateral (b) radiograph of knee after first stage resection and articulating spacer, and AP (c) x-ray of knee after second stage reimplantation
The survivorship of 96 knees treated with two-stage revision was reportedly 93.5 % at 5 years and 85 % at 10 years [15]. If reinfection recurs, it is possible to perform a second two-stage revision. The 2009 study reported on 18 patients with a failed two-stage revision undergoing a second two-stage revision. Infection was eradicated in 14 of 18 patients.
Two-stage exchange seems to be of advantage and more reproducible than the one-stage exchange. The success rate is about 90 %.
46.6 Spacers
Spacers are useful to stabilise or tension the soft tissues, potentially facilitate the second-stage procedure, and reduce bone loss between stages. Use of antibiotic-impregnated cement has greatly improved the chances of success in treatment of infected arthroplasties [16]. Antibiotics suitable for this purpose should be heat- stable, broad-spectrum, bactericidal at low concentrations, at low risk of allergy/delayed hypersensitivity, and available in powder form with low serum binding, which facilitates release from the spacer at high concentrations for prolonged periods.
High doses of antibiotic (6–8 g), delivered by hand-mixed cement, have been shown to be clinically safe. The use of a high dose is important for sustained elution of antibiotics at levels that are therapeutic for the pathogenic organisms during the first stage of two-stage exchange. Antibiotic elution from PMMA depends on the antibiotic dose, the combination of antibiotics used, and the type of cement [17]. The recommended doses of antibiotics are 2–5 times higher for therapeutic use than for prophylactic use [1]. Most antibiotics have a high initial release followed by a reduced, constant elution over the next several days. Low-dose antibiotic cement is indicated for prophylaxis. It is appropriate for the second stage of two-stage arthroplasty, where optimum mechanical characteristics of the cement are desired.
A higher dose of gentamicin or tobramycin will increase the amount of antibiotic initially released and prolong the duration of the bactericidal level of the antibiotic. However, higher doses of vancomycin may not increase the in vivo elution characteristics [18]. Tobramycin may synergistically increase the release of vancomycin in the cement mix by “passive opportunism” – a phenomenon where one antibiotic dissolves, resulting in increased porosity and increased elution of the other antibiotic. Tobramycin elutes better from Palacos cement (Heraeus Medical, Hanau, Germany; marketed by Zimmer Inc., Warsaw, IN) than from Simplex cement (Stryker, Kalamazoo, MI). Premixed antibiotic cements have a low dose of antibiotics [19]. Hand mixing without a vacuum results in increased porosity, which increases antibiotic elution.
Antibiotic spacers are either static and non-articulating or articulating. The maintenance of appropriate soft-tissue tension and joint range of motion may reduce the need for more extensile exposures at the second-stage reimplantation if articulating spacers are used [20]. A recent review of static and mobile spacers antibiotic-impregnated cement spacers used in two-stage exchange arthroplasty demonstrated similar success rates with either type of implant. There is an ongoing controversy over the optimal type of antibiotic spacer to use. Static spacers, first described by Cohen [20], were historically preformed in the shape of a hockey puck that was inserted loosely in the joint space after the cement was polymerised. This technique was associated with an inability to match the shape of the distal femur with the proximal tibia, spacer subluxation, wound breakdown, secondary bone loss, and erosion of quadriceps mechanism. This led to the development of the moulded arthrodesis block. In this technique cement is placed in the knee joint in a doughy state so that it conforms to the shape of the bone ends and stabilises the knee joint by interdigitation (Fig. 46.2a, b). Static spacers have infection eradication rates approximating 88 % [21–24]. Static spacers restrict knee movement between stages; distract and preserve the joint space; provide stability to the limb, with a concomitant reduction in inflammation; and give rest to the infected joint. The disadvantages of a static/nonmobile spacer include contracture of the extensor mechanism, collateral ligament shortening, arthrofibrosis, tibial and femoral bone loss (incidence of 60 %), and potential difficulty with secondary exposure for reimplantation.
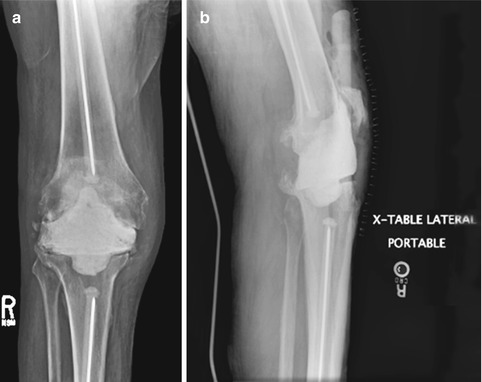
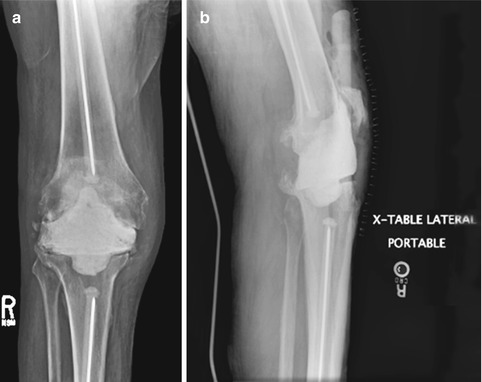
Fig. 46.2
AP (a) and lateral (b) radiographs after resection of knee with moulded arthrodesis block spacer with medullary dowels
Articulating spacers maintain joint motion between stages and cause less periarticular scarring resulting in easier surgical exposure at reimplantation. They also result in marginally better postoperative ROM and function compared with static spacers, though statistical significance is not reached. Infection eradication rates with articulating spacers approximate 92 % [20, 22, 25–30].
Articulating spacers can be metal-on-polyethylene (new components or recycled components) or cement-on-cement. Cement-on-cement articulating spacers can be prefabricated or manufactured in the operating room with cement moulds or can be handmade (Fig. 46.3a, b). A mobile spacer formed in the operating room is inexpensive and provides the option for adjustable antibiotic dosing. Articulating spacers reduce bone loss compared with static spacers. Problems with articulating spacers include risk of cement fracture, spacer dislocation, and potential problems with wound healing [17]. Disadvantages of mobile spacers formed in the operating room include additional time to construct, a limited number of sizes, and additional cost. The disadvantages of preformed mobile spacers include cost, limitation in sizes, antibiotic type, and antibiotic dose.
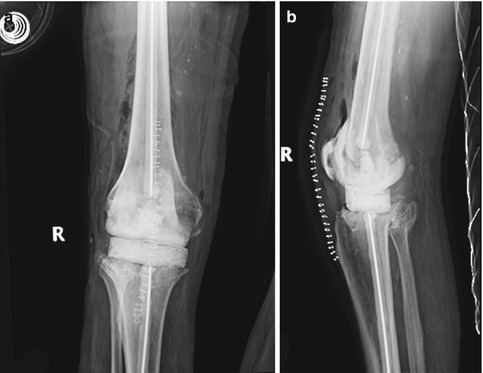
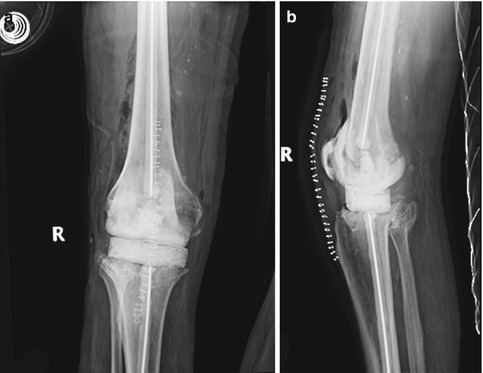
Fig. 46.3
AP (a) and lateral (b) radiographs after resection of knee with articulating cement spacer with medullary dowels
Cement-on-cement spacers [25, 26] have more surface area for antibiotic elution, though these are expensive, take more OR time, and are prone to cement fracture and formation of cement debris. Preformed cement spacers (Interspaced Knee, Exactest, Gainesville, and F) deliver a lower dose of a single antibiotic [14]. The prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) (Depuy, Warsaw, IN) includes a bicompartmental metal femoral component articulating with a polyethylene tibial component. This has a 91 % infection eradication rate but has not yet been approved by the US Food and Drug administration [27]. Metal-on-polyethylene spacers [22, 27–30] use a new or recycled femoral component and polyethylene insert for articulation (Fig. 46.4a, b). This provides an inexpensive articulation that can be custom fitted to each patient. However, there is a lower surface area for antibiotic elution compared with cement-on-cement spacers.
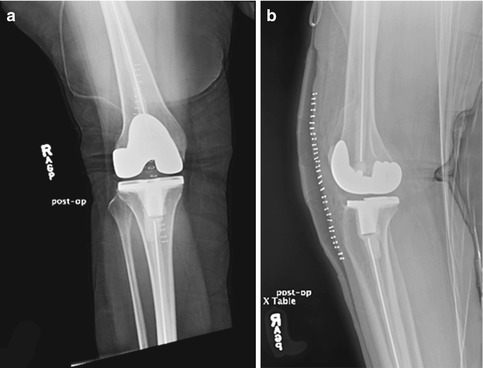
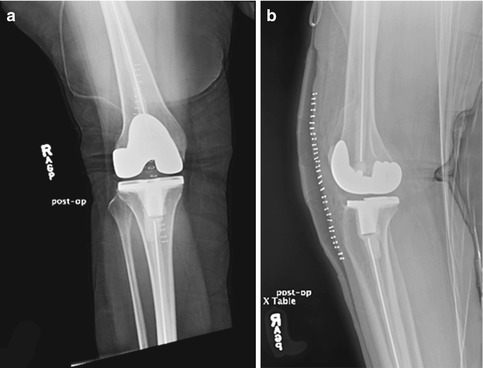
Fig. 46.4
AP (a) and lateral (b) radiographs after resection of knee with articulating new metal-on-polyethylene with medullary dowels
Mobile spacers seem to be of advantage compared with fixed spacers. Antibiotics of 6–8 g should be added to the cement. The recommended doses of antibiotics are 2–5 times higher for therapeutic use than for prophylactic use.
46.7 Resection Arthroplasty
Resection arthroplasty is removal of all components with aggressive debridement of all infected tissues without reimplantation of new components or spacers. Resection arthroplasty is suitable for low-demand patients after failure of other treatments in patients with polyarticular rheumatoid arthritis. The indications for resection arthroplasty are inadequate bone and soft tissues, recurrent infections particularly with drug-resistant organisms, and failure of multiple previous attempts at exchange arthroplasty in low-demand disabled patients. This eradicates infection at the cost of stability and function of the knee [30]. The success rate of eradication has been reported from 50 % to 89 % [31].
46.8 Arthrodesis
Arthrodesis has become less common in North America with the success of two-stage exchange arthroplasty. Arthrodesis is indicated in young, high-demand patients and those with deficient extensor mechanism, inadequate soft tissues for reimplantation, and multiple reinfections with highly resistant organisms. Disadvantages include persistent pain, functional limitation, and limb-length inequality. Mabry et al. [31] found that arthrodesis by intramedullary nailing has a union rate of 96 % compared with 67 % with external fixation. However, the risk of recurrent infection associated with IM nailing is 8.3 % compared with 4.9 % with external fixation. Infection eradication rates with arthrodesis approach 94 %, though the complication rate is also very high (40 %) [31]. Knee arthrodesis remains a reasonable salvage alternative for the difficult infected TKR, but complication rates are high (Figs. 46.5, 46.6 and 46.7).










