Chapter 3 Adult Neurogenic Communication Disorders
A complex array of communication disorders co-occur with the various physical and sensory deficits after many neurologic disorders seen by the physiatrist. As noted by Brookshire,12 the prefix neuro means “related to nerves or the nervous system,” while the suffix genic means “resulting from” or “caused by.” This chapter reviews the major acquired neurogenic communication disorders seen in adults as a result of a disturbance of the neurologic system.
Types of Communication Disorders Caused by Nervous System Pathology
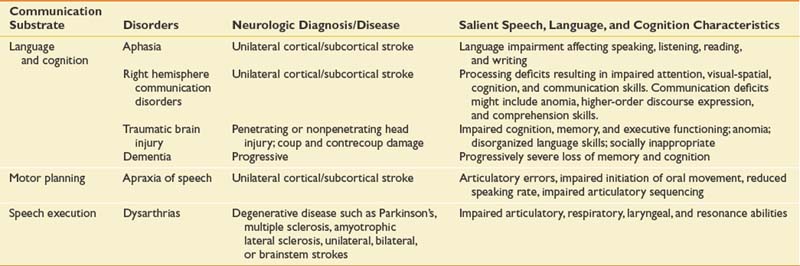
Cognitive-communicative disorders as a result of brain injury, disease, or pathology might include aphasia and related neurobehavioral disorders; communicative-cognitive disorders secondary to right hemisphere stroke, traumatic brain injury, and dementia; and the motor speech disorders including the dysarthrias and apraxia of speech. Table 3-1 presents the major neurogenic communication disorders, neurologic diagnosis or disease, and salient speech-language and cognitive characteristics.
Brain Plasticity and Neurorehabilitation
Research in the basic neurosciences over the past 30 years has provided strong evidence regarding the dynamic aspects of the brain to change. While most of the research to date has been in animal models, human translational studies have begun to emerge. The term brain plasticity refers to the capacity and resiliency of the brain to undergo structural and functional changes.19 The ability of the brain to adapt and restructure is particularly evident after injury and has important implications for rehabilitation and recovery of function. Ideally, the rehabilitation team will work collaboratively to determine the best intervention at the optimal time to take advantage of the brain’s malleability. For an individual patient this can include the selection of the type and intensity of behavioral treatment (the external stimulation). At times this might be paired with administration of adjunctive brain stimulation such as a neuropharmacologic agent, electrical cortical stimulation, and/or transcortical magnetic stimulation.
In animals, the type of the external stimulation has been shown to be very important. A large body of research demonstrates that the type of input affects brain reorganization.36,51,57 This has been termed use-dependent,51 or more recently learning-dependent, activity.57 This refers to the specificity of the experience after brain injury being critical in determining what brain and behavioral changes will occur. Nudo et al.57 found that motor maps are altered by motor skill acquisition versus repetitive use alone, and brain plasticity coincided with the reacquisition of motor skills in lesioned animals and the acquisition of new motor skills in intact animals. These data imply that at critical recovery periods in humans, restorative treatments should target the most complex behaviors that a patient can produce. It could be that focusing only on compensatory activities rather than restorative functions has costs in terms of ultimate recovery of function.
Neuromodulation can be done with certain pharmacologic agents. When paired with behavioral treatment, some agents, particularly those affecting the catecholamine system (dextroamphetamine, methylphenidate, levodopa), have been found to enhance outcome after both focal6,22,35,69 and diffuse46,71 cortical experimental injury. It should be noted that this does not extend to all behaviors.66 Explorations of pharmacologic modulation have been done in humans to facilitate recovery from poststroke deficits such as aphasia and hemiplegia30,65,77,78 and to enhance recovery of cognitive deficits subsequent to traumatic brain injury.38,81 Physiologic events after brain injury can complicate the timing for administration of various agents. Drugs that are effective in the very acute or subacute period after injury may be ineffective or even detrimental at later recovery periods.28 Our experiences and that of others are encouraging regarding the use of certain agents to accelerate recovery; however, not all clinical studies report positive findings.26,59
Aphasia and Related Neurobehavioral Disorders
Aphasia
Aphasia in adults occurs as a result of acquired brain damage to the language-dominant hemisphere, usually the left, and shares common neurophysiologic features with other stroke consequences. Chapey and Hallowell16 provide a straightforward definition: “Aphasia is an acquired communication disorder caused by brain damage, characterized by an impairment of language modalities: speaking, listening, reading, and writing; it is not the result of a sensory deficit, a general intellectual deficit, or a psychiatric disorder.” The language impairments can range from mild with some word-finding problems (anomic aphasia) to severe with very little ability to speak, understand, read, or write (global aphasia). In the United States today, more than 1 million people are living with aphasia,45 and 80,000 new patients with aphasia will be treated each year.56
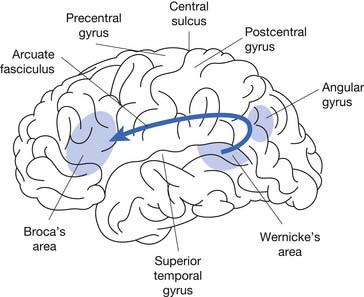
Since the time of Broca,11 aphasia has probably been the most studied neurogenic communication disorder. Because of the nature of the injury and the critical left hemisphere language association areas (Figure 3-1), aphasia has been classified in terms of the characteristics of the linguistic deficits and the location of the lesion.
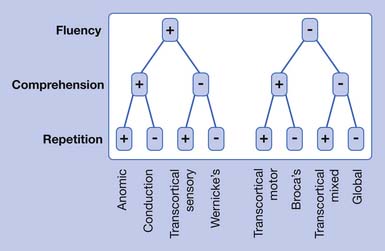
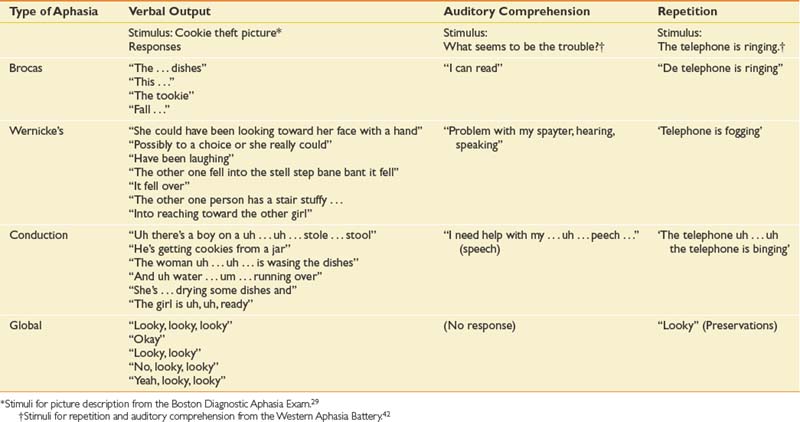
The traditional aphasia classification system9,43 is based on clusters of language symptoms and contrasts the characteristics of verbal output, auditory comprehension, and repetition ability (Table 3-2). This framework forms the basis for two of the most frequently employed formal assessments used by speech-language pathologists: the Boston Diagnostic Aphasia Exam29 and the Western Aphasia Battery.42
Table 3-2 The Aphasias: Comparisons of Verbal Output, Repetition, Auditory Comprehension, Associated Signs, and Region Affected
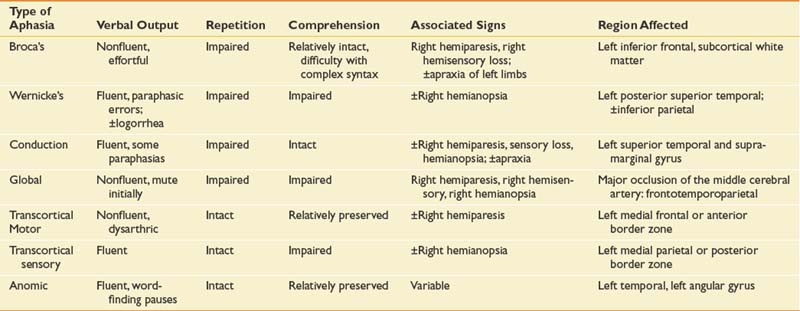
Modern imaging studies and research in psycholinguistics have shown limitations with the traditional classification scheme. In particular, the roles of Wernicke’s and Broca’s area are not as clear as they first appeared.18 A variety of other left hemisphere regions, both cortical and subcortical, have been found to be involved in language processing. While it is now recognized that the processing of language requires a large network of interacting brain areas, it is also the case that certain linguistic behaviors group together and are often predictable depending on the anterior or posterior location of the lesion. Anterior aphasias include Broca’s and transcortical motor aphasia. Posterior aphasias include Wernicke’s, conduction, and transcortical sensory aphasias. Global and anomic aphasias are not as localized. Aphasias limited to strictly subcortical pathology have also been described.55 Whether speech output is nonfluent versus fluent, the degree of auditory comprehension deficit, and the ability to repeat can be checked by the physiatrist at the bedside (Figure 3-2) to get an estimate of the type of aphasia.
Broca’s Aphasia
This classic nonfluent aphasia is characterized by effortful speech and misarticulations (see Table 3-3 for speech samples of the primary aphasia types). Verbal language (i.e., vocabulary and syntax) is restricted, resulting in anomia and reduced utterance length (i.e., typically one to four words in length). Auditory comprehension is impaired but relatively better than verbal language. The reading deficit in Broca’s aphasia resulting from frontal pathology is variable and is well described.9 Written language is usually as severely impaired as verbal language. Lesions causing Broca’s aphasia are most often in the left posterior inferior frontal cortex and underlying structures.
Wernicke’s Aphasia
In 1874, Karl Wernicke described an aphasia syndrome very different from Broca’s aphasia. Patients with Wernicke’s aphasia have fluent speech output with normal prosody (vocal pitch and stress) and close to normal grammar. However, their speech is filled with literal and verbal paraphasic errors. (Literal paraphasias are sound substitutions within a word; for example, “binging” for “ringing.” Semantic paraphasias are whole word substitutions; for example, “mother” for “sister.”) These paraphasias and other made-up words (neologisms) cause the speech of the Wernicke patient to be empty, although the sentence length can be normal. Another characteristic of speech output in Wernicke’s aphasia can be an inability to stop speaking (logorrhea) and press of speech (rapid, compressed utterances). Patients with Wernicke’s aphasia have severely impaired auditory comprehension, sometimes to the point of understanding no spoken language, and are often unaware of their own deficits.43
To be classified as Wernicke’s aphasia, there must be a repetition deficit. Wernicke’s aphasia usually occurs from damage to the left superior temporal region. It might also occur after damage in the inferior parietal cortex involving the supramarginal and angular gyri.43
Conduction Aphasia
Conduction aphasia is relatively uncommon and occurs in only about 10% of patients with aphasia. In this type of aphasia, the speech output is fluent (near-normal utterance length) but with considerable word-finding difficulties (anomia), relatively preserved auditory comprehension, and significant difficulty with verbal repetition. The speech of patients with conduction aphasia is characterized by literal paraphasias and numerous self-corrections as they search for the right word. This self-correction can cause the speech of the individual with conduction aphasia to have numerous pauses and filled pauses (“ah … a … ah … ah”). Reading and writing deficits are variable depending on the specific site of the lesion. Brain damage in conduction aphasia is in the left superior temporal area, the supramarginal gyrus of the parietal lobe, or both.
Global Aphasia
Patients with global aphasia have severe impairments in all language modalities (speaking, listening, reading, and writing). Global aphasia is characterized by severely impaired auditory comprehension and very limited speech output. Individuals with global aphasia produce few understandable utterances, and their speech is marked by perseverative utterances used repeatedly. It should not be overlooked, however, that many patients with global aphasia have some islands of spared intact function, and these must be found to utilize for communication. A type of global aphasia has been described with severe communication deficits but an absence of hemiplegia.75 Brain damage causing global aphasia is usually massive (frontotemporoparietal), caused by complete occlusion of the middle cerebral artery with dense right hemiplegia of both arm and leg.
Transcortical Motor Aphasia
Patients with transcortical motor aphasia have some similarities to those with Broca’s aphasia but with intact repetition. The transcortical aphasias refer to aphasias occurring from lesions in the border zone outside the perisylvian language areas. Individuals with transcortical motor aphasia have nonfluent, limited speech output that sometimes has a dysarthric quality. There are often long pauses between utterances. The patient with transcortical motor aphasia does not have as much difficulty with syntax as the patient with Broca-type aphasia. Auditory comprehension and reading comprehension are generally well preserved. Writing deficits can mirror those seen in spoken language. Transcortical motor aphasias occur as a result of occlusion of the anterior cerebral artery or damage to border zone areas in the frontal lobe superior or anterior to Broca’s area.43
Anomic Aphasia
Anomic aphasia can often be the residual of good recovery from other aphasia syndromes. Patients in the acute stage who are classified as having anomic aphasia have the best prognosis for recovery of any of the aphasias. The primary difficulty in anomic aphasia is word finding and naming. Speech output is fluent with numerous pauses, filled pauses, and circumlocutions (describing and/or defining a function of an object for which a name cannot be retrieved; for example, “you brush your teeth with it”). Verbal repetition, auditory comprehension, reading, and writing are relatively preserved. Although anomic aphasia is the least localized of all the aphasias, it often occurs from focal damage to left temporal and parietal areas.9
Crossed Aphasia
Rarely (incidence between 1% and 11%) a classic aphasia occurs in a strongly right-handed person from a lesion on the right side of the brain. When this occurs it is referred to as a crossed aphasia. The language characteristics in this case can be classic, paralleling the types of aphasias seen from left hemisphere lesions, with almost reversed mirror-image specialization of the two hemispheres.79 Other patients have anomalous hemispheric specialization with both language functions and visual spatial functions in the right hemisphere.2
Primary Progressive Aphasia
A specific primary progressive aphasia (PPA) is now recognized.21,44,50 This disorder blurs the lines between focal and diffuse disease. In contrast to aphasia caused by an acute event such as a stroke, PPA has an insidious onset. Although the family or patient might claim there was a specific event, careful history will reveal a progressive onset with the patient being aware of the language deficits before family members. The most frequent presenting complaint is word-finding difficulty. During the first 2 years, the patient with PPA often has symptoms that appear to be localized, similar to those of an aphasia subsequent to a stroke. After the early course of the disease, PPA usually progresses to dementia with the characteristic cognitive disorders of other dementias. A diagnosis of PPA requires a minimum 2-year history of language decline, relative sparing of other mental functions, independence in activities of daily living, a neurologic workup excluding other causes of aphasia, and a neuropsychological workup that supports the complaints.50
Management of Aphasia
Treatment by the speech-language pathologist is based on a careful assessment of all communication modalities: speaking, listening, reading, and writing. The patient’s deficit areas and relative strengths and weaknesses are determined. Assessments of both impairment and activity/participation levels are ideally done as defined by the World Health Organization.83 The focus of speech-language treatment in the acute and subacute recovery period is restoration of speech and language abilities, and treatment is individualized. Education and counseling with the family are also important.5
Numerous therapy approaches specific to the complex speech-language behaviors exhibited by patients with aphasia are available and have been demonstrated to be effective.23 Metaanalyses63,64 of the outcomes of therapy for aphasia have shown that language therapy for aphasia has a significant positive impact on recovery in the acute and chronic phases, and the amount of speech-language treatment is a critical factor for establishing effective and long-lasting improvements.7,10,17,52 Intensive aphasia therapy (on average 98 hours) appeared to be a requirement for positive outcomes,10,72 and shorter amounts of treatment (on average 44 hours or less) are not effective.7,10,73 Evidence-based practice is not the least expensive use of rehabilitation dollars but is the better investment of resources if significant improvement is expected.
Related Neurobehavioral Disorders
Often co-occurring with aphasia are a number of related neurobehavioral disorders, and it is important to differentiate them from the communication disorder. Only apraxia and agnosia are reviewed here. The physiatrist should consult a more detailed mental status examination such as Strub and Black70 and/or a neuropsychologist for a differential diagnosis of these higher-order motor and sensory processing disorders.
Apraxia
Apraxia is an acquired disorder of learned skilled, sequential motor movements that cannot be accounted for by elementary disturbances of strength, coordination, sensation, or lack of comprehension or attention.25 Apraxia is not a low-level motor disturbance but a deficit in motor planning that involves the integrative steps that precede skilled or learned movements.70 Apraxias occur more often as a result of left hemisphere lesions. Because adequate verbal comprehension is a prerequisite to valid praxis (motor integration needed for execution of complex learned movements) testing, it is important for the speech-language pathologist to be consulted regarding auditory comprehension abilities when a motor planning problem is suspected. It is also important that patients with a motor planning deficit not receive a diagnosis of comprehension difficulties, because the motor planning disorder prevents their making an adequate response to comprehension testing.
Ideamotor apraxia is the most common type of apraxia. Patients with this form of apraxia fail to perform previously learned motor acts accurately. Impairments can be seen in buccofacial, limb, or whole-body musculature. Ideational apraxia is a disturbance of complex motor planning of a higher order than is seen in ideamotor apraxia. It is a breakdown in the performance of a task that involves a series of related steps.70 Brief screening by commands can help the physiatrist to differentiate a motor planning disorder from a true language disorder (Table 3-4).
Table 3-4 Evaluation of Ideamotor Apraxia
| Commands | Errors |
|---|---|
| Buccofacial | |
| “Show me how to—”: | |
| 1. “Blow out a match.” | Difficulty giving short, controlled exhalation; saying “blow”; inhaling; difficulty maintaining appropriate mouth posture |
| 2. “Protrude your tongue.” | Inability to stick out tongue; tongue moving in mouth but tending to push against front teeth and not protruding |
| 3. “Drink through a straw.” | Inability to sustain a pucker; blowing instead of drawing through the straw; random mouthing movements |
| Limb | |
| “Show me how to—”: | |
| 1. “Salute.” | Hand over head; hand waving; improper position of hand |
| 2. “Use a toothbrush.” | Failure to show any proper grip; failure to open mouth; grossly missing the mouth; using finger to pick teeth; not allowing adequate distance for shaft of toothbrush; using the finger as a toothbrush |
| 3. “Flip a coin.” | Movements miming tossing the coin into the air with an open hand; supinating or pronating the hand as though turning a doorknob; flexing the arm without flipping thumb against finger |
| 4. “Hammer a nail.” | Moving hand back and forth horizontally; pounding with fist |
| 5. “Comb your hair.” | Using fingers as teeth of comb; smoothing the hair; making inexact hand movements |
| 6. “Snap your fingers.” | Extension of fingers with patting movements; tapping of finger on thumb; sliding finger off thumb with insufficient force |
| 7. “Kick a ball.” | Stamping foot; pushing foot along floor; moving foot laterally |
| 8. “Crush out a cigarette.” | Stamping foot; kicking foot on floor |
| Whole body | |
| “Show me how to—”: | |
| 1. “Stand like a boxer.” | Awkward arm position; hands at side |
| 2. “Swing a baseball bat.” | Difficulty in placing both hands together; chopping movements |
| 3. “Bow” (for a man) or “Curtsy” (for a woman) | Any inappropriate truncal movement |
(Modified from Strub RL, Black FW: The mental status examination in neurology, ed 4, Philadelphia, 2000, FA Davis, with permission of FA Davis.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree