Fig. 3.1
Medial view of the knee: attachment sites (Redrawn from Bonasia et al. [13]). AT adductor tubercle, ME medial epicondyle, sMCL superficial medial collateral ligament, MPFL medial patellofemoral ligament, POL posterior oblique ligament, MF meniscofemoral ligament, MT meniscotibial ligament
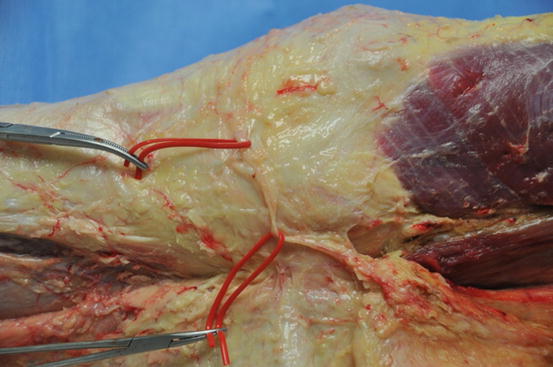
Fig. 3.2
Saphenous nerve and infrapatellar branch of the saphenous nerve
The sMCL (Figs. 3.1 and 3.3) has 1 femoral and 2 tibial attachments (proximal and distal). The femoral attachment has an oval shape and is located 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. The proximal tibial attachment is primarily to soft tissues, mainly to the anterior arm of the semimembranosus tendon. The distal tibial attachment of the sMCL is just anterior to the posteromedial crest of the tibia. The average distance of the proximal tibial attachment is 12.2 mm from the tibial joint line. The average distance of the distal tibial attachment is 94.8 mm from the femoral attachment and 61.2 mm from the tibial joint line. The average distance from the distal tibial attachment to proximal tibial attachment is 49.2 mm [15].
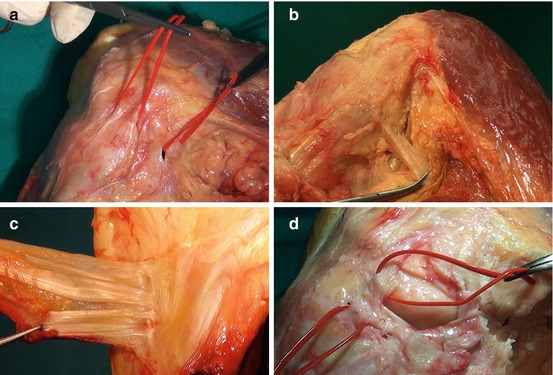
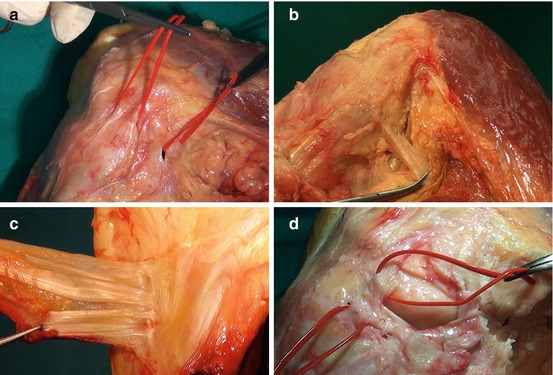
Fig. 3.3
Anatomy of the medial side of the knee. (a) sMCL (left loop) and POL (right loop). (b) Semimembranosus tendon (held by the Kelly clamp). (c) Distal sMCL insertion (after detachment of the pes anserinus). (d) dMCL with meniscofemoral (proximal loop) and meniscotibial (distal loop) ligaments
The dMCL (Figs. 3.1 and 3.3) is a thickening of the medial joint capsule. The dMCL consists of the meniscofemoral (MF) and meniscotibial (MT) ligaments. The MF ligament is longer than the MT ligament and its attachment is located 15.1 mm posterior and distal to the medial epicondyle. The MT ligament is shorter and thicker and attaches just distal (3.2 mm average) to the cartilage of the medial tibial plateau [15].
The posterior oblique ligament (POL) consists of three fascial attachments (Figs. 3.1 and 3.3): superficial, central (tibial), and capsular. The three attachments course off the distal aspect of the semimembranosus tendon mainly, but also off the medial meniscus, posteromedial tibia, and medial head of the gastrocnemius. On the average, the POL attaches on the femur 7.7 mm distal and 6.4 mm posterior to the adductor tubercle and 1.4 mm distal and 2.9 mm anterior to the gastrocnemius tubercle [15].
3.7 Repair Technique
Examination under anesthesia is performed to completely assess the injury. Arthroscopy can be used to rule out any other associated lesions and determine the site of the dMCL injury. In the acute setting, arthroscopy should be performed quickly and with gravity inflow, to minimize fluid extravasation. A hockey stick (or longitudinal) incision is made from the medial proximal tibia to the medial femoral epicondyle, curving posteriorly in line with the intermuscular septum. For isolated distal or proximal detachment repair, a more limited approach can be used. In the case of combined treatment of acute complete MCL tear and an ACL tear, exposure of the MCL is easier if approached through a separate medial incision as opposed to extending the tibial incision for the ACL reconstruction. Attention should be paid to preserve the saphenous nerve (Fig. 3.2). The crural and sartorial fascia is incised longitudinally. Hematoma is removed. The injured structures are then identified [16].
The injured structures are identified and should be repaired from the deepest structure outward. A peripheral tear of the medial meniscus is commonly seen and repaired with an open technique (Fig. 3.4) [16]. A meniscofemoral ligament tear can be directly repaired using sutures alone or suture anchors (Fig. 3.5). Suture anchor fixation is preferred for meniscotibial ligament tear. If injured, the POL is repaired by direct suture back to the femur. Repair of the deep structures is completed with the knee held in varus and full extension [16].
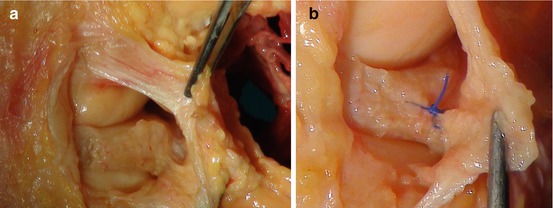
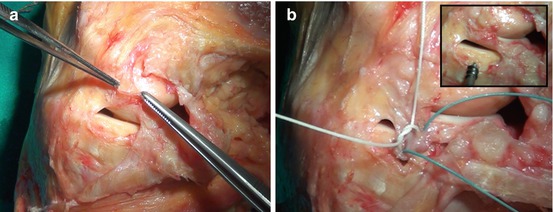
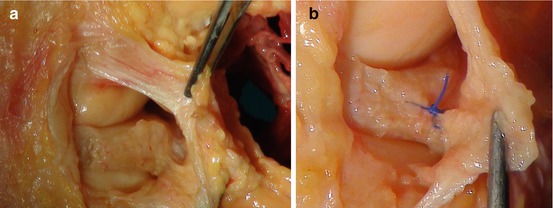
Fig. 3.4
(a) Capsular detachment of the medial meniscus. (b) Repair of the capsular detachment with an open technique
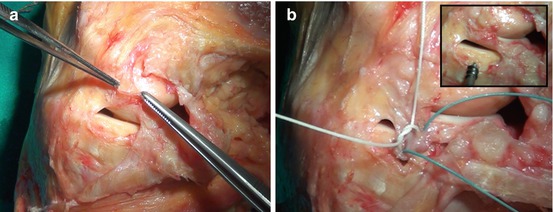
Fig. 3.5
Repair technique. (a, b) A meniscotibial ligament tear repaired with suture anchor fixation
Femoral avulsion of the sMCL (Fig. 3.6) leaves the best tissue for repair using suture anchors, staples, or a screw/washer. However, repair in this location is associated with postoperative stiffness, more than in other locations [17]. This is due to the great importance of the femoral isometric point of the sMCL. It is difficult to attach the sMCL back to the femoral isometric point, due to soft tissue retraction. Acute complete avulsions off of the tibia can be repaired, using either suture anchors or staples [16].
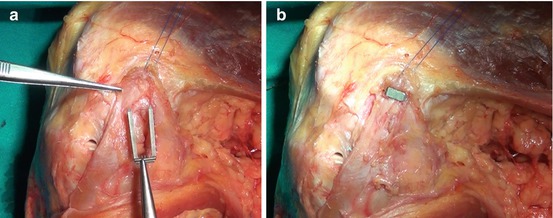
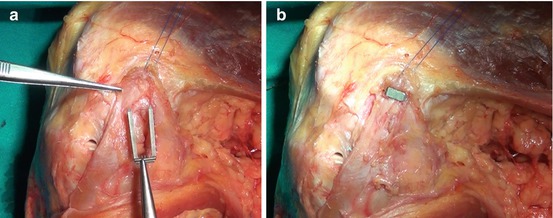
Fig. 3.6
Repair technique. (a, b) Femoral avulsion of the sMCL repaired using Richard’s staples
The semimembranosus portion of the POL can be repaired with interrupted absorbable sutures and sutured to the posterior border of the MCL in a pants-over-vest fashion. Occasionally, mid-substance and tibial-sided injuries require augmentation, due to the poor soft tissue quality. The sMCL is fixed at 30° of knee flexion [16]. Finally, the tourniquet is deflated and inspection and control of potential excessive bleeding from the inferior medial geniculate artery and its branches is performed. A compressive dressing is applied postoperatively.
Postoperatively, the patient is kept in a hinged knee brace with protected weight bearing. Passive range of motion from 0 to 90° is begun immediately. Hyperextension and flexion over 90° should be avoided during the first 2 weeks. Isometric and closed kinetic chain strengthening are allowed immediately. Full range of motion is allowed 2 weeks after surgery, and full weight bearing is allowed 6 weeks after surgery. Return to sports is generally allowed 6 months after surgery.
3.8 Results
Good results have been reported for the conservative treatment of grade I and II MCL complex tears [18, 19].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








