It is most common in the second decade of life, associated with contact athletic activities.
Acromioclavicular (AC) dislocations represent 9% to 10% of acute traumatic injuries to the shoulder girdle.
It is more common in males (approximately 5:1).
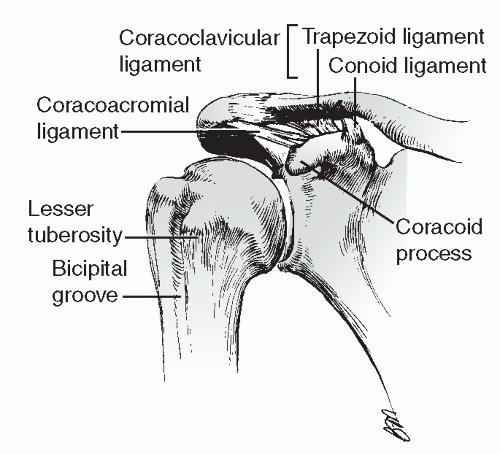
The AC joint is a diarthrodial joint, with fibrocartilage-covered articular surfaces, located between the lateral end of the clavicle and the medial acromion.
Inclination of the plane of the joint may be vertical or inclined medially 50 degrees.
The AC ligaments (anterior, posterior, superior, inferior) strengthen the thin capsule. Fibers of the deltoid and trapezius muscles blend with the superior AC ligament to strengthen the joint.
The AC joint has minimal mobility through a meniscoid, intraarticular disc that demonstrates an age-dependent degeneration until it is essentially nonfunctional beyond the fourth decade.
The horizontal stability of the AC joint is conferred by the AC ligaments, whereas the vertical stability is maintained by the coracoclavicular ligaments (conoid-medial, trapezoid-lateral).
Deltoid and trapezius fascial attachments reinforce the superior AC ligament contributing to vertical stability as a secondary stabilizer.
The average coracoclavicular distance is 1.1 to 1.3 cm.
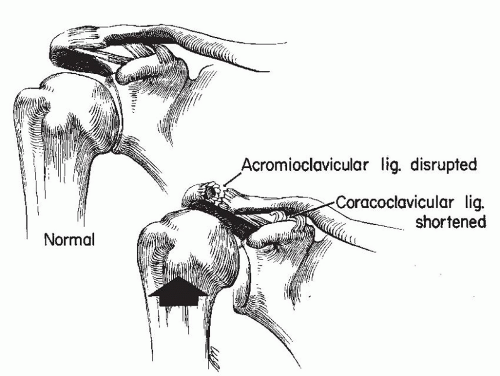
Direct: This is the most common mechanism, resulting from a fall onto the shoulder with the arm adducted, driving the acromion medial and inferior.
Indirect: This is caused by a fall onto an outstretched hand with force transmission through the humeral head and into the AC articulation (Fig. 12.2).
Fractures: clavicle, acromion process, and coracoid process
Pneumothorax or pulmonary contusion with type VI AC separations
The patient should be examined while in the standing or sitting position with the upper extremity in a dependent position, thus stressing the AC joint and emphasizing deformity.
The characteristic anatomic feature is a downward sag of the shoulder and arm.
A standard shoulder examination should be performed, including assessment of neurovascular status and possible associated upper extremity injuries. Inspection may reveal an apparent step-off deformity of the injured AC joint, with possible tenting of the skin overlying the distal clavicle. Range of shoulder motion may be limited by pain. Tenderness may be elicited over the AC joint.
A standard trauma series of the shoulder (anteroposterior [AP], scapular-Y, and axillary views) is usually sufficient for the recognition of AC injury. The Zanca view is taken with the x-ray beam in 10 to 15 degrees of cephalic tilt. This view allows better visualization of the distal clavicle.
Ligamentous injury to the coracoclavicular joints may be assessed via stress radiographs, in which weights (10 to 15 lb) are strapped to the wrists, and an AP radiograph is taken of both shoulders to compare coracoclavicular distances (difficult to do in the acute setting).
This injury is classified depending on the degree and direction of displacement of the distal clavicle (Table 12.1 and Fig. 12.3).
strengthening, and acceptance of deformity. Younger, more active patients with more severe degrees of displacement and laborers who use their upper extremity above the horizontal plane may benefit from operative stabilization. Repair is generally avoided in contact athletes because of the risk of reinjury.
TABLE 12.1 Classification of Acromioclavicular (AC) Joint Injury | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|