Fig. 34.1
A detailed history and thorough clinical examination to differentiate and identify the different causes for recurrent or persistent problems after TKR
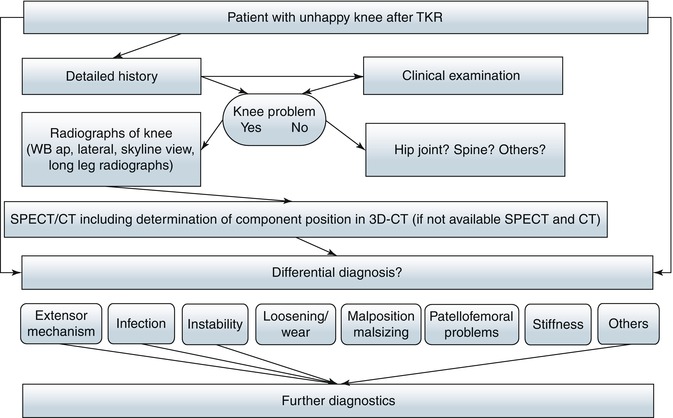
Fig. 34.2
Proposed diagnostic algorithm for patients with clinical symptoms after TKR including SPECT/CT as primary diagnostics
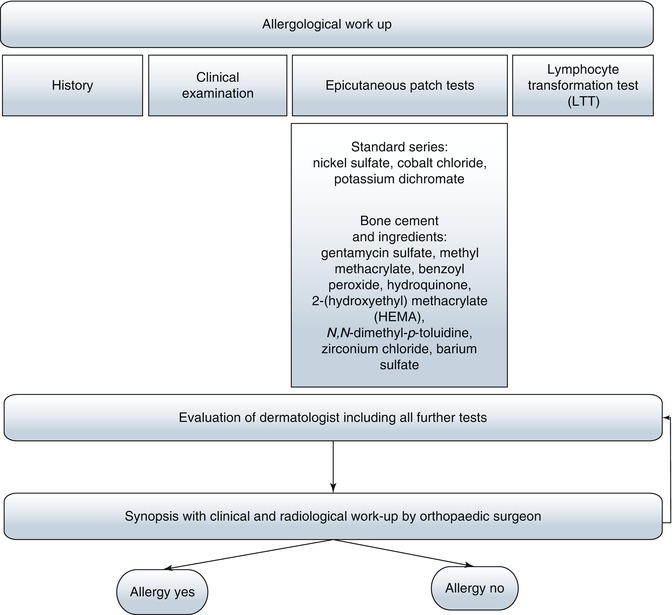
Fig. 34.3
Recommended additional allergological workup
Fig. 34.4
Recommended additional workup in case of suspected infection
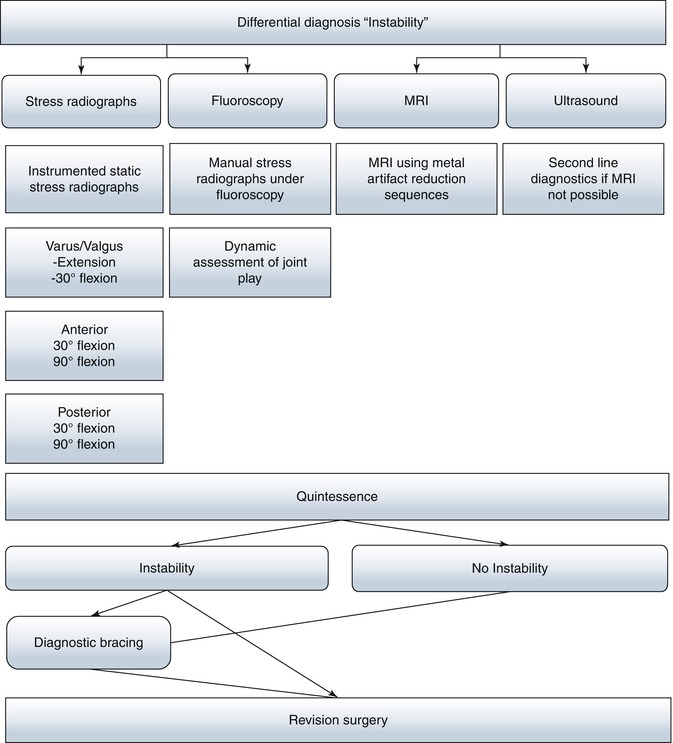
Fig. 34.5
Recommended additional workup in case of suspected instability
An optimal diagnostic algorithm should be based on medical history, thorough clinical examination, microbiological workup and detailed imaging analysis. It should be able to identify all causes and not only the most common ones.
Every patient presenting to our specialised knee clinic undergoes a standardised diagnostic workup including a detailed medical history and thorough clinical examination. Its role in the establishment of the optimal diagnosis and cause of the patient’s problems cannot be overestimated. Clearly, in most of cases, it allows one to differentiate between extra-articular and intra-articular causes and points toward the most common causes (Fig. 34.1).
For detailed information on history taking and clinical examination, see Tables 34.1 and 34.2 and Chaps. 25 and 35. Standardised conventional radiographs (anterior-posterior and lateral weight bearing) are mandatory and help to identify frank component malposition, polyethylene wear, component over- or undersizing, component overhang, notching, overstuffing or gross loosening [15, 26, 40, 45]. However, radiographs are not very sensitive due to their dependency on a “perfect” projection [26].
Table 34.1
Key questions for a detailed patient history in symptomatic patients after TKR
What is the most prominent problem – pain, stiffness, stability, swelling |
|---|
Pain |
Character and type of pain (sharp, dull, tingling, burning, etc.) |
Intensity |
Location and radiation |
Onset (early versus intermediate versus late following primary TKR) Early pain may indicate an acute infection, prosthetic malalignment or soft tissue impingement. Pain occurring over the long term is more likely to be caused by component loosening, polyethylene wear, ligamentous instability, stress fracture or late haematogenous infection |
Duration (how long does the pain last) |
Factors that aggravate or relieve the pain, e.g. weight bearing, climbing up and down the stairs |
Activity related versus pain at rest |
Pain related to activity rather than rest suggests instability, irritation of the soft tissues, loosening or mechanical impingement. Pain at rest may be caused by infection or a neuroma if made worse by contact with clothes |
Pain after TKR different from before TKR? |
Former surgical or outpatient reports |
Type and design of the TKR (primary versus revision TKR, cruciate retaining versus cruciate substituting, non-constrained versus semi-constrained versus hinged TKR, cemented versus uncemented, size of TKR, bearings, company’s name and TKR type) |
Was the original indication for the primary surgery correct? |
Pain in other joints? |
Medication |
Detailed pain and medication history |
Patient’s psychological well-being pre– and post–surgery |
Assessment of anxiety, depression, self-efficacy, somatization, pain intolerance |
Table 34.2
Key points of clinical examination in symptomatic patients after TKR (always compare to preoperative status!)
Inspection (always in comparison to contralateral side) |
Assessment of gait pattern |
Limping |
Coronal, sagittal and rotational alignment of leg |
Thrusting while walking on heel and toes indicating instability |
Position of patella (patella alta or baja?) |
Scars (hypertrophy, dehiscence, tethering, fat necrosis) |
Erythema or hematoma |
Swelling/effusion |
Discharge |
Loss of hair, discoloration (complex regional pain syndrome) |
Clinical examination |
Palpation of all knee structures including bony references, collaterals, patellar tendon, quadriceps tendon, etc. |
Integrity of extensor mechanism (palpation and active clinical examination, straight leg raise) |
Tenderness (joint line, peripatellar, patellofemoral, collaterals, posterior, medial, lateral) |
Play of patellofemoral joint (overstuffing – pain in particular is worse between 30° and 60° knee flexion, instability) |
Patellar tracking during flexion-extension and rotation |
Neurological assessment (hypersensitivity, hyposensitivity, hyperalgesia, Tinel sign) |
Vascular status |
Active and passive range of motion (hyperextension, fixed flexion deformity, extensor lag) |
Stability testing (varus-valgus in extension and 30° flexion, anterior-posterior in 90° flexion and 30° flexion, mismatch of flexion and extension gap) |
Examination of other joints (hip, ankle, spine) |
Whole-leg radiographs are necessary for assessment of the mechanical and anatomical knee axes [15, 45]. On patella skyline views and lateral radiographs, patella maltracking, overstuffing of the patellofemoral joint, a patella fracture or a patella baja or alta position is assessed (see Chap. 28). Stress radiographs in comparison to the contralateral side or fluoroscopy (see Chap. 32) are performed in suspicion of instability or impingement [17, 38].
Conventional radiographs (anterior-posterior and lateral weight bearing) are the primary imaging modality.
Dealing with patients in pain after TKR is challenging, and we believe that one has to use the best available diagnostic imaging modalities. Hence, we have chosen SPECT/CT in our hospital as a standard imaging modality in these challenging patients [25–29, 51, 52] (see Chap. 37). The diagnostic benefits of SPECT/CT, combining mechanical, structural and biological information, clearly outweigh the radiation dose burden to the patient, which is in our protocol 2–3 mSv [25–29, 51, 52]. It is our opinion that there is no place for conventional bone scintigraphy or SPECT alone [25–29, 50–52]. Only if there is no SPECT/CT available, should one use these conventional, purely nuclear medicine imaging techniques. Currently we only have limited experience with arthro-SPECT/CT, but it could, in the future, be an important adjunct in exceptional cases.
SPECT/CT has replaced bone scans and CT alone as a diagnostic tool in unhappy patients after TKR. If not available, CT and SPECT should be done.
CT, either as part of SPECT/CT or alone, should be used to accurately assess femoral and tibial TKR component position (varus-valgus, flexion-extension, internal rotation-external rotation) [25, 26]. The determination of TKR component position should be performed on 3D-CT as this is the only accurate method available [25, 26].
Currently, the use of MRI is limited due to metal artefacts caused by the metal components of the TKR. It is only used in studies, and it is indicated in exceptional cases [23, 42]. In particular, it currently does not significantly add to the evaluation of the bone prosthesis interface, which is crucial in the process of loosening diagnostics [23, 42]. However, this might change in the future.
Ultrasound could help to identify instability, impingement and extensor mechanism problems but is rarely used [12].
Currently MRI and ultrasound are adjuncts of diagnostics in exceptional cases.
Arthroscopic assessment of the knee should be performed in exceptional cases in which low-grade infection, impingement and patella clunk syndrome are suspected [4, 11, 13, 22, 34, 37, 55]. It has also been used to assess the degree of polyethylene wear [37].
In suspicion of an infection erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and blood leukocyte levels need to be determined [3, 31]. However, laboratory parameters are often nonspecific [33]. Blood leukocyte counts are not elevated in most patients with infected prostheses [33]. Sedimentation rates are abnormal in patients with infection, but this finding may also be seen in uninfected patients, limiting the value of the test [33]. Joint aspiration or, in selected cases, arthroscopy is performed to obtain tissue or synovial fluid samples for culturing and microbiological testing [44]. Multiple aspirates from different areas within the joint increase the diagnostic confidence [44]. Aspiration only makes sense in an antibiotic-free interval of at least 2 weeks. The colour and viscosity of the synovial fluid must be noted. The aspirate should undergo Gram staining, leukocyte cell count and both anaerobic and aerobic culture. Leukocyte levels >1,100/mm3 and 64 % polymorph cells indicate an infectious problem [44]. When taking tissue samples, at least five should be obtained for microbiology and one for histology [44]. In addition, we recommend an anti-granulocyte or white blood cell scintigraphy if available as SPECT/CT [19, 21, 35, 36]. The diagnosis of an infection should never be based only on laboratory findings. Moreover, it is a combination of clinical, serological and imaging findings.
Diagnosis of infection should never be based only on laboratory findings.
FDG-PET is not part of our algorithm, as it is not commonly available for us and it does not show any benefit in terms of diagnostic sensitivity or specificity detecting infection after TKR. However, in the future it could be useful in this clinical scenario [47].
Finally, all information obtained is analysed and weighted by the orthopaedic surgeon, and one or several diagnoses are established. Establishment of the correct diagnosis is like a mosaic picture. Here the clinical picture is formed by a number of diagnostic parts. The treatment is then individually tailored to each patient.
All information obtained is analysed and weighted by the orthopaedic surgeon. Establishment of the correct diagnosis is like a mosaic picture. Here the clinical picture is formed by a number of diagnostic parts. The treatment is then individually tailored to each patient.
In summary, the algorithm presented is used in our specialised knee clinic. It has stood the test of time and does help to standardise diagnostics and subsequent treatment of patients with problems after TKR. This algorithm should be adapted to local hospital conditions. A better and more accurate identification of the patient’s cause of the problems will improve the patient’s outcome after revision surgery or nonsurgical treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








