Chapter 7 A comprehensive treatment approach
Failure to respond to standard treatment approaches
Manipulation, mobilization and muscle energy techniques
Sacroiliac belts and compression shorts
Complementary forms of treatment
Medications and electrostimulation
Treatment of internal structures
Malalignment that fails to respond to treatment
Unnecessary investigations and treatment
1. may be putting him or her at increased risk of injury
2. may have precipitated the symptoms or caused an injury
3. may be perpetuating and/or aggravating the symptoms
4. may be slowing down or preventing recovery from an injury
5. may be preventing the person from advancing in their chosen line of work or sport.
This chapter first looks at the shortcomings of using standard treatment approaches for back pain caused by malalignment. It then outlines a logical and proven treatment programme. The need for the person’s day-to-day participation is emphasized, in order to increase the chances of achieving the best results quickly and help maintain improvements, especially in-between formal treatment sessions. The chapter concludes with a differential diagnosis of other conditions to consider, appropriate investigations and alternate treatment options should the recommended approach fail to achieve lasting realignment and resolution of symptoms and signs. It is a lead-in to Chapter 8 which looks at alternate manual therapy techniques and complementary treatment methods currently used to increase the chances of achieving lasting relief from the problems caused by malalignment and the ‘malalignment syndrome’.
Failure to respond to standard treatment approaches
Malalignment and the standard treatment of low back pain
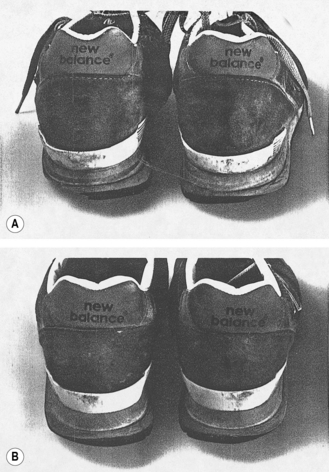
Examination 1 week after his last marathon attempt revealed ‘rotational malalignment’ with ‘anterior’ rotation of the right innominate. There was increased tone and tenderness to palpation in the left hip abductor muscle mass and the length of the iliotibial band down to its insertion (Fig. 3.41). On Ober’s test, passive left hip adduction was significantly restricted compared with that on the right (Fig. 3.44). Gait assessment showed that he pronated on the right and supinated on the left side. A pair of running shoes he had used for training in the preceding 6 months showed changes consistent with this weight-bearing pattern: the heel cup collapsed inward on the right and outward on the left (Fig. 7.1A).
Correction of the malalignment quickly resulted in a resolution of symptoms and signs, and allowed for an immediate return to a full training schedule. Symptoms did not recur during the next marathon 6 months later and he was able to finish the race. On reassessment shortly after, alignment had been maintained, and the left hip abductors and TFL/ITB were relaxed and non-tender. The heel cups of a new pair of running shoes of the same make still maintained a neutral (vertical), symmetrical position after a comparable 6 months of training (Fig. 7.1B).
The posterior pelvic tilt
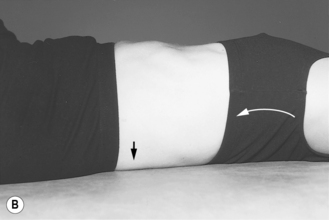
The posterior tilt consists of actively rotating the pelvic unit posteriorly while lying supine, in order to temporarily flatten the back and decrease or eliminate the lumbar lordosis (Fig. 7.2B). In someone who presents in alignment but suffers from mechanical back pain, the tilt may be helpful in that it decreases pressure on the lumbar facet joints, opens the foramina, relieves compression pain from the posterior parts of the vertebrae, and decreases pressure within the disc and any tendency of the disc to bulge anteriorly.
As we have seen, ‘rotational malalignment’ is often associated with sacral torsion, ‘locking’ of one or other SI joints, pelvic obliquity and a lateral lumbar convexity that reverses at the thoracolumbar junction to give rise to a thoracic curve convex in the opposite direction (Fig. 3.14). Spinal tenderness localizes primarily to the sites of increased stress: the lumbosacral and thoracolumbar junctions.
The posterior tilt aims to flatten the lumbar segment in one plane – the sagittal – in order to decrease the lordosis. This completely ignores the fact that, when malalignment is present, there will also be an accentuated lateral convexity of the lumbar segment to the right or left. In order to create that lumbar curve in the coronal (frontal) plane, the vertebrae must have undergone simultaneous axial rotation into the convexity and side-flexion into the concavity; in other words, simultaneous rotation around the vertical and sagittal axes with movement in the transverse and coronal (frontal) planes, respectively. A left lumbar convexity, for example, results from L1–L4 inclusive side-flexing to the right and rotating to the left, maximal at the apex (Figs 2.42, 4.6, 4.33). There will usually also be an element of extension, in keeping with a residual lumbar lordosis of varying degree (Fig. 3.14A). As a result, facet joint surfaces have been moved closer together on the right and separated on the left side (reverse of L5 findings shown in Fig. 2. 52B).
In someone presenting with malalignment, carrying out the posterior pelvic tilt may, therefore, actually cause more pain (Box 7.1).
Box 7.1 Factors that can cause the ‘posterior tilt’ to be painful
1. trying to flatten a curve in one plane (sagittal), ignoring the fact that the curve exists in two planes (sagittal and coronal) and that the individual vertebrae are rotated in three planes (sagittal, coronal and transverse)
2. further increasing stress on the points of curve reversal (thoracolumbar junction) and the twisted lumbosacral junction
3. increasing the tension on already tender posterior soft tissue structures (e.g. the supra- and interspinous ligaments, and thoracolumbar myofascia) by changing their length-tension ratio
4. stretching the tender posterior pelvic ligaments (e.g. iliolumbar)
5. aggravating the facet joint irritation that results with vertebral rotation by increasing the:
1. tender posterior pelvic ligaments (especially those crossing the posterior SI joint (Fig. 2.5)
2. tender PSIS, ischial tuberosity (sacrotuberous insertion, biceps femoris origin; Fig. 2.6), coccyx, coccygeal spicule (see Ch. 4 and Fig. 4.44)
3. protuberant, and particularly stiff, unyielding spinous processes of:
Traction
Traction is unlikely to straighten the curvatures of the spine if these are:
1. part of a compensatory scoliosis, with segmental vertebral rotation in opposing directions (lumbar, thoracic and cervical) attributable to an ‘upslip’ or ‘rotational malalignment’
2. caused by the rotational displacement of one or more isolated vertebrae.
1. increasing stress on sites of curve reversal and vertebral rotational displacement
2. further increasing the tension in myofascial and ligamentous structures already tensed-up because of ‘facilitation’, skewing of length-tension ratios and other changes attributable to the malalignment.
1. achieving some relaxation through the ‘contract–relax’ mechanism (see Ch. 8)
2. opening up the spaces between the vertebrae and facet joints to relieve compression, reactive muscle tightening and any irritation of exiting nerve roots
3. minimizing or abolishing strain in muscles that have been ‘facilitated’.
Extension exercises and back extensor strengthening
Extension of the back while lying prone, maximal in the ‘cobra’ position (Fig. 7.3), can increase the pressure on facet joint surfaces that are already approximated on one side by vertebral rotation in conjunction with malalignment (Fig. 2.52B). Back extension also causes further stress on the particularly stiff sites of curve reversal, where the adjacent vertebrae rotate in opposite directions (Fig. 3.14B,C).
This is not to say, however, that one cannot have a person do exercises for the back extensor muscles. Given the frequent involvement of these muscles (e.g. reflex spasm, tenderness, disuse weakness and wasting), a stretching and strengthening programme should be part of rehabilitation – provided a core strengthening programme is well underway to ensure pelvic and spine stability (Figs 7.25–7.29) and alignment is starting to be maintained. Any arching of the back should continue to be limited to the pain-free zone to avoid triggering reflex muscle spasm. A contraction of these muscles, done in a way that avoids excessive back extension, can be initiated in the prone position simply by:
1. extending only the head and neck (no more than 2–3 cm off the surface at first; Fig. 7.4A), progressing to also lifting the shoulders at the same time (Fig. 7.4B)
2. alternately raising the straight right and left leg 1–2 cm off the surface (Fig. 7.4C), and eventually both legs simultaneously:

Fig. 7.25 Exercises: one leg extension with co-contraction of the inner pelvic muscle unit.
(Courtesy of Lee 1999.)

Fig. 7.28 Strengthening of one leg extensor in four-point kneeling with a balance challenge on a shuttle MVP.
(Courtesy of Lee 1999.)

Fig. 7.29 Strengthening of the lateral system with co-contraction of the inner unit on a FITTER.
(Courtesy of Lee 1999.)
The emphasis is on frequent repetition of contractions that are brief to start with: holding to a slow count of 1 or 2 is adequate, followed by relaxation to allow for a maximum inflow of blood and clearance of waste (Fig. 7.4E).
Sit-ups
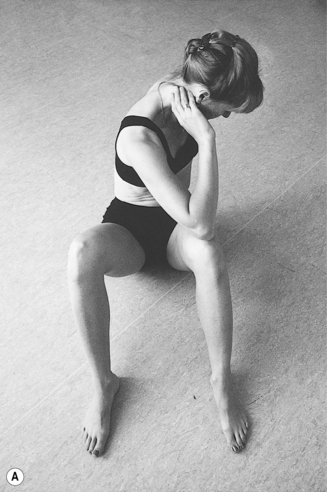
There seems to be some obsession in our society with doing a sit-up from supine-lying to vertical and, ultimately, perfecting the ‘abdominal crunch’ by touching the nose or the right and left elbow alternately to the opposite knee (Fig. 7.5). Most patients presenting with back pain, whether it be on the basis of malalignment or some other cause, are likely to run into grief with these manoeuvres. Pain often increases as the neck and trunk pass the upright (vertical) position:
1. coming up into sitting leaning slightly forward, at which point the posterior cervical and thoracic paravertebrals and erector spinae, especially, are activated to prevent the trunk from falling forward
2. going back into supine-lying, at which point the anterior neck muscles (e.g. paravertebrals, scalenes and sternocleidomastoid) contract to prevent the head from falling backward.
2. a recurrence of malalignment because of the repeated torsion of trunk and pelvis.
The intent is to strengthen the abdominal muscles, especially:
In someone with severe back pain, a good contraction primarily of rectus abdominis can be initiated simply by raising the head and neck while lying supine (Fig. 7.6A), then progressing to raising the shoulders just 2–3 cm off the surface (Fig. 7.6B) and possibly incorporating graduated straight-leg raises (especially if activating the neck and shoulder girdle muscles causes discomfort, as it might in someone following a ‘whiplash’ injury). Similar to attempts at strengthening the back extensors, the contractions should initially be of short duration, with the muscles being completely relaxed in-between contraction, carried out within the zone of comfort and avoiding triggering any discomfort or outright pain at all costs. Instructions are for an initial set of 10 contractions daily, increasing to two and then three sets as strength and endurance improve. At that point, either the duration of the contraction and/or the degree of trunk flexion can gradually be increased, following the progression outlined above for the back extensors.



Fig. 7.6 Graduated abdominal muscle strengthening. Simultaneously drawing the umbilicus toward the plinth and tightening up the muscles around the rectum will ensure a strengthening not only of rectus abdominis, but also transversus abdominis and the pelvic floor muscles (see Figs 2.31B, 2.53). (A) Initially only the head is lifted off the plinth. (B) The shoulders clear the plinth, along with the head. (C) Both heels are just clearing the plinth (with the legs held straight).
It cannot be stressed enough that strengthening of the above muscles must be preceded by strengthening of the ‘inner’ and ‘outer’ core and by efforts at realignment, both of which are an intricate part of the overall treatment programme for the ‘malalignment syndrome’ and will be discussed in that context later (Figs 2.28–2.40, 7.25–7.29).
Always consider the possibility of an underlying problem of malalignment when:
Manipulation, mobilization and muscle energy techniques
1. instability of one or both SI joints, the pubic symphysis and/or one or more lumbar vertebrae attributable to impaired ‘form’ and ‘force’ closure or neural control (see Ch. 2)
2. a generalized joint hypermobility (e.g. Ehler-Danlos syndrome)
3. persistently increased tension or actual spasm of muscles that are in a position to cause malalignment to recur.
In addition to the muscle energy technique (MET) and traction, which are the main approaches to realignment discussed in this book, there are numerous other manual therapy techniques that find application in the treatment of malalignment – a number of these are discussed in Chapter 8. They range from the high-velocity, low-amplitude (HVLA) manipulations traditionally associated with chiropractic, the long-lever, low-velocity (LLLV) osteopathic techniques to re-establish joint play and the seemingly more gentle methods (e.g. craniosacral release, zero-balancing, NUCCA technique) which are now being embraced by many chiropractors, osteopaths, physicians and physiotherapists alike because they may be more successful in achieving long-term correction.
1. The myofascial tissue on the concave side of a curve in the spine is put in a relaxed position and will shorten with time (Fig. 2.60). When the curve is decreased or eliminated with realignment, excessive tension in these contracted structures will exert a unilateral force on the vertebrae that can result in a recurrence of the malalignment, unless realignment is combined with a graduated stretching programme to help them regain their normal length.
2. The persistence of a trigger point in the right quadratus lumborum after realignment may perpetuate a general increase in tension in that muscle and cause the recurrence of a ‘right upslip’ (Fig. 2.62).
3. Mobilization may effectively correct the malalignment of the pelvis initially caused by an L1 rotation with resultant ‘facilitation’ of iliopsoas on one side and ‘inhibition’ on the other. The pelvic malalignment is, however, more likely to recur if the L1 rotation, and any persistent asymmetry of tension in right compared with left iliopsoas, is not also attended to after realignment of the pelvis.
This 37-year-old female runner presented with symptoms of cervicogenic brachialgia in a left C6 and C7 dermatome referral pattern and frequent headaches following a fall down a flight of stairs. On initial examination, the cervical spine range of motion was reduced in all planes of movement, the deltoid muscle weak (4/5) but the neurological screen otherwise unremarkable. In addition to a postural scoliosis, there was evidence of ‘anterior’ rotation of the left innominate and vertebral rotational displacement at the C2/3, C6/7 and T11/12 levels. Surface electromyography (SEMG) showed increased paravertebral muscle activity readings (the light bars in Fig. 7.7) throughout the spine, worse on the left than the right and at the levels noted to have rotated (e.g. C6/7 and T11), also the lumbosacral region. These SEMG findings were consistent with postural compensation and a reactive increase in paravertebral muscle tension throughout the back.
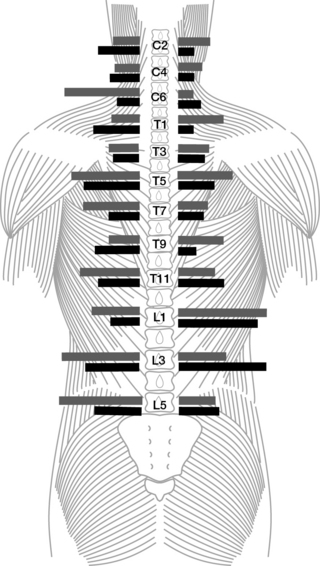
Fig. 7.7 A surface electromyograph of the paravertebral muscles to detect the tension level (see ‘Case History 7.2’). The light horizontal bars indicate the findings after injury; note the asymmetry and the large number of levels showing an increase in activity. The dark horizontal bars denote the findings after 3 months of treatment, including manual therapy. The asymmetry has significantly decreased in the cervical and thoracic levels, and there are now fewer levels showing increased activity (persisting mainly in the lumbar region).
(Redrawn courtesy of D.J. McCallum, unpublished data 1999.)
After three months of therapy aimed at mobilizing the pelvis and spine and relaxing the paravertebral muscles, the frequency of headaches had significantly decreased and she was otherwise asymptomatic. The neurological screen was now unremarkable. Repeat SEMG (the black bars in Fig. 7.7) still showed some higher readings, now localizing to the left C2–C4 and T7, right L1 and L3 levels, probably indicative of an ongoing attempt to compensate for the changing postural pattern. The muscle tension overall was, however, significantly reduced and more symmetrical than that recorded initially.
Techniques for correction of ‘rotational malalignment’
In most cases, pain can be avoided by a minor modification of the technique being used; often this amounts to no more than simply changing the position (e.g. decreasing the angle of hip and knee flexion; Figs 7.9B, 7.9Ei,ii, 7.13E,F).

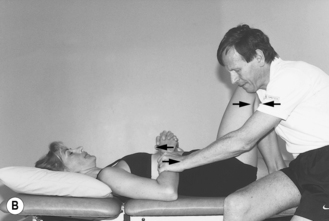
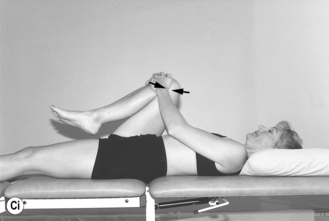
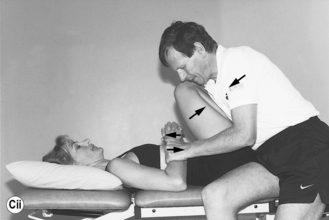
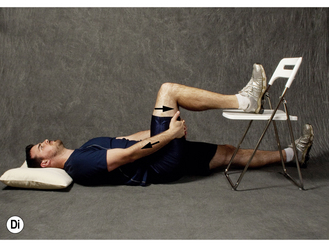
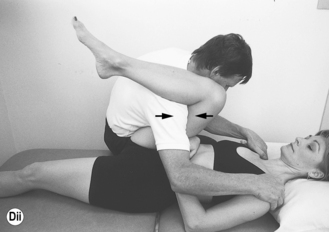


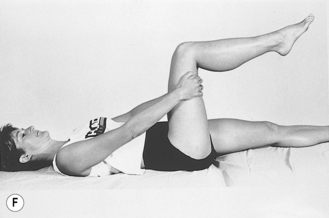
Fig. 7.9 Muscle energy technique for the correction of right innominate ‘anterior’ rotation: using gluteus maximus by blocking attempted right hip extension. (A) One-person technique. (B) Two-person technique. (C) To take up any slack as the hip extensors relax on repeated resisted contraction, gradually increase the hip flexion angle (compare to (A) and (B), respectively), provided that this does not cause or aggravate pain. (D) To modify the technique for a painful knee (e.g. osteoarthritis, patellofemoral compartment syndrome), decrease the knee flexion angle: (i) one-person technique – leg resting on chair; (ii) two-person technique – leg resting on assistant’s shoulder. (E) Modified technique resisting hip extension: (i) one-person (note: knee resting over pillow in some flexion, to keep hamstrings relaxed); (ii) pre- or post-partum. (F) Incorrect technique: the effectiveness of a resisted hip extensor contraction is decreased by simultaneous quadriceps contraction, seen here keeping the knee in 90 degrees flexion – the lower leg is held unsupported up in mid-air by rectus femoris which is also capable of exerting a simultaneous, counterproductive anterior rotational force on the innominate bone (see Figs 2.46 C, 2.59, 7.12).
Sometimes, however, a patient has such generalized discomfort and soft tissue tenderness that one just cannot use a certain approach, such as the ‘muscle energy technique’ (MET), during the initial stages of treatment. In that case, an even more gentle and less ‘invasive’ method, one that requires less effort on the part of the patient or involves working at sites distal to where pelvic and spine instability and pain are most severe, may be more appropriate (e.g. craniosacral release or the NUCCA technique; see Ch. 8). One can then try reintroducing MET, possibly in conjunction with some of the complementary methods of treatment at a later date, once the patient’s condition has started to improve. However, the ‘more gentle’ techniques of realignment, or even just limiting initial treatment to core muscle strengthening may fail, especially if there is a problem such as soft tissue or joint inflammation and pain, or joint instability secondary to ligament laxity or joint degeneration. In that case, attempts at trying to achieve stability and realignment may have to be discontinued until the inflammation has settled down and/or the ligaments have been strengthened (see ‘anti-inflammatories’ and ‘prolotherapy’, below) to allow the patient to finally get on with a progressive core strengthening, realignment and postural retraining programme.
Muscle Energy Technique (MET)
Right innominate: ‘anterior’ rotation
A resisted active contraction of the right gluteus maximus can be harnessed to create a posterior rotational force on the right innominate in order to correct the ‘anterior’ rotation (Figs 2.5B, 2.36, 2.37, 7.8Ai). Essentially, gluteus maximus originates from the posterior iliac crest, along the posterior gluteal line, and inserts primarily into the greater trochanter (Figs 2.5B, 7.8Ai,ii). One of its actions is to extend the hip joint when the thigh is free to move (Fig. 7.8Aiii). However, by resisting right hip extension, and hence any movement of the femur, one effectively reverses the muscle origin and insertion (Fig. 7.8C). Gluteus maximus will now exert a posterior rotational force on the right innominate, which is still free to move. The person attempts to extend the hip but this movement is prevented by having him or her:
1. hold on to the thigh or shin, with the hip and knee flexed (Figs 7.8C,D, 7.9)
2. push against another person or an object that serves to provide the resistance needed (Figs 7.8, 7.9).
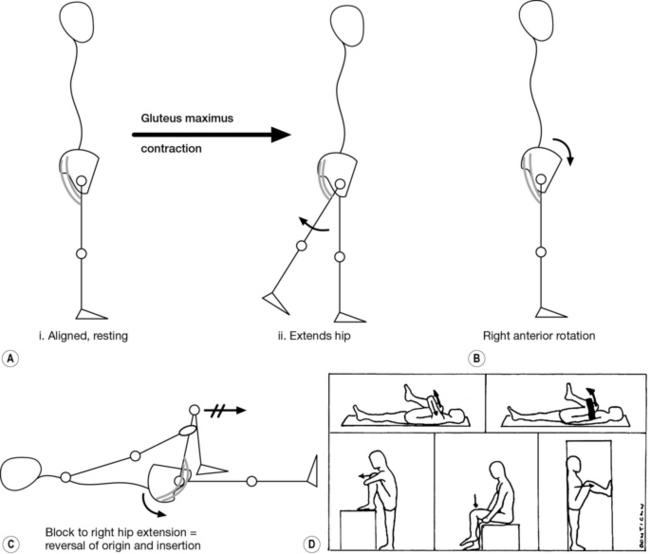
Fig. 7.8 Muscle energy technique to correct a ‘rotational malalignment’. (A-C) The biomechanics of using gluteus maximus (Fig. 2.5B) to correct a right innominate ‘anterior’ rotation (B). (A) The muscle acts as a hip extensor when the leg is free to move. (C) Blocking right hip extension reverses the muscle origin and insertion, creating a posterior rotational force on the innominate. (D) Muscle energy techniques can be used in a variety of positions
(Courtesy of DonTigny 1997.)
Following each contraction, a muscle usually relaxes and will lengthen a bit more. In the case of gluteus maximus, one can take up the slack each time by letting the thigh drop down toward the person’s chest and, if tolerated, even toward the opposite shoulder (given that gluteus maximus is oriented somewhat diagonally across the buttock) before attempting the next resisted contraction (Fig. 7.9C). The repeated contraction and relaxation of gluteus maximus in this manner will successfully correct an ‘anterior’ rotation in 80-90% of people. For those who have pain on knee flexion (e.g. aggravation of osteoarthritic pain; patello-femoral syndrome), the procedure can be modified by supporting the lower leg (calf) on the assistant’s shoulder or on a chair to decrease the knee flexion angle (Fig. 7.9D). Similarly, if there is hip or groin pain, one may find a position of comfort either by abducting or adducting the femur slightly or by decreasing the hip flexion angle.
Left innominate: ‘posterior’ rotation
Iliacus
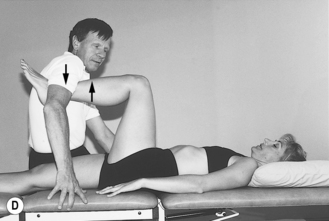
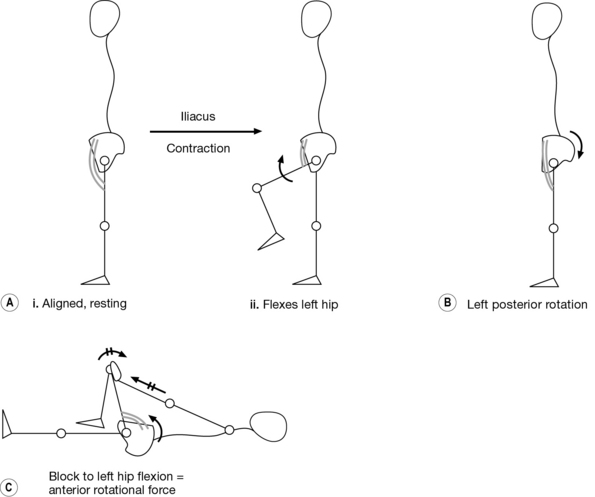
Iliacus originates primarily from the anterior iliac crest and upper iliac fossa, inserting into the tendon of psoas major and directly into the lesser trochanter (Figs 2.46B,C, 4.2, 7.10A). If the thigh is free to move, the primary action of iliacus is to flex the hip joint (Fig. 7.10Aii). By resisting left hip flexion, one effectively reverses the origin and insertion and creates a force that will rotate the left innominate anteriorly (Fig. 7.10C). When sitting or lying supine, the person attempts to flex the hip, but any movement is again blocked.
One-person technique
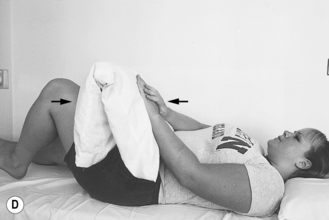
1. the counterforce is provided by the arms/overlapping hands pushing against the anterior aspect of the left thigh (Figs 7.10C, 7.11A,B)
2. the elbows are preferably locked in extension so that, when lying supine, the force goes straight up to the shoulder girdle and through to the surface he or she is lying on
Two-person technique
An assistant provides the resistance needed to prevent any movement on attempted hip flexion (Fig. 7.11B,C,F).
Rectus femoris
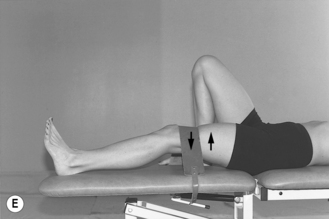
Rectus femoris originates from the anterior inferior iliac spine and anterior rim of the acetabulum; it inserts indirectly into the tibial tubercle by way of the patellar tendon (Figs 2.46 C, 2.59, 7.12Ai). It is the only muscle of the quadriceps complex that crosses both the hip and knee joint so that, in addition to extending the knee, it can also flex the hip joint when the knee is in full extension (Fig. 7.12Aii, Cii). This muscle can, therefore, be effectively used to create an anterior rotational force on the ‘posteriorly’ rotated left innominate (Fig. 7.12B) by:
1. blocking attempted extension of the left knee when that knee is flexed (Fig. 7.12 Ci)
2. blocking attempted left hip flexion when that knee is straight (which actually also engages iliacus; Fig. 7.12Cii).
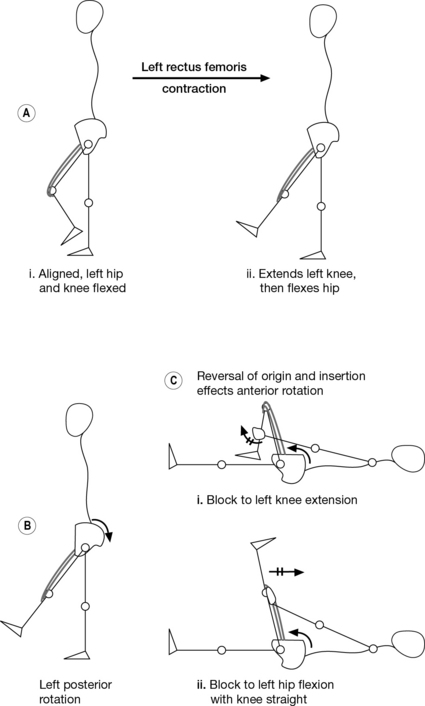
Fig. 7.12 Muscle energy technique: the biomechanics of using left rectus femoris for the correction of a left innominate ‘posterior’ rotation. (A) The muscle originates from the anterior inferior iliac spine on the innominate and inserts into the tibial tubercle (see Figs 2.46 C, 2.59). (B) It acts as a knee extensor when extension can occur (e.g. non-weight-bearing. (Ci) Blocking knee extension reverses the origin and insertion, creating an anterior rotational force on the innominate. (Cii) Blocking hip flexion when the knee is extended will also engage rectus femoris.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree