Impulse-Based Neural Mechanisms
Nonimpulse-Based Neural Mechanisms
Chiropractic theory maintains that subluxation and adjustment/manipulation have important physiologic effects that include increasing range of joint motion, changes in facet joint kinematics, increased muscle strength, attenuation of alpha-motoneuron activity, enhanced proprioception, changes in beta-endorphins, and increased pain tolerance. 1 A common theme in each of the various conceptual models of vertebral subluxation is the expectation that spinal biomechanical derangement causes some form of nerve dysfunction or nerve interference.
According to Vernon2:
This has come to be understood as either (1) some element of compression of the spinal nerves in the environs of the intervertebral foramen or (2) …initiation of pain in the spinal joints … capable of creating secondary aberrant reflex effects such as increases in motoneuron or sympathetic neural activity.
Harrison and colleagues34 and 5 propose that prolonged alterations in posture or spinal canal length impart stretch, compression, or tensile forces to the spinal cord, especially in the sagittal plane (flexion and extension) and that such postures have direct and indirect effects on the central nervous system (CNS) and its associated structures.
For various reasons, including the increasing body of supportive research evidence, a rapid expansion of interest has occurred in spinal adjustive/manipulative procedures by medical physicians, physical therapists, osteopaths, and health care decision makers. Health providers who manage patients with low back pain and neck pain may find it rare not to have discussion on the topic of spinal manipulation and adjustment because a significant number of their patients are receiving or considering this form of health service. An understanding of the various theories and concepts related to the spinal adjustment, its mechanisms, clinical manifestations, and results is therefore increasingly necessary. 6 Various hypotheses have been advanced to explain the association of vertebral subluxation complex (VSC) with neuronal disturbance and related dysfunction and symptoms.7891011 and 12 Meeker and Haldeman1 identify at least five mechanical and neurologic mechanisms (Table 8-1).
| Action | Mechanism |
|---|---|
| Mechanical-anatomic | Alleviation of an entrapped facet joint inclusion or meniscoid that has been shown to be heavily innervated139 and 140 |
| Mechanical-anatomic | Repositioning of a fragment of posterior annular material from the intervertebral disk140,141 |
| Mechanical-anatomic | Alleviation of stiffness induced by fibrotic tissue from previous injury or degenerative changes that may include adaptive shortening of fascial tissue142,143 |
| Neurologic-mechanical | Inhibition of excessive reflex activity in the intrinsic spinal musculature or limbs or facilitation of inhibited muscle activity144145 and 146 |
| Neurologic-mechanical | Reduction of compressive or irritative insults to neural tissues147 |
The common hypotheses related to the neuropathophysiologic manifestations associated with altered joint mechanics that represent the focus of this chapter appear in Box 8-1.
Box 8-1
NEUROBIOLOGIC RELATIONS OF SUBLUXATION COMPLEX
CONTEMPORARY HYPOTHESES
1. Nerve compression hypothesis
2. Aberrant spinal reflex hypotheses
a. Somatosomatic
b. Somatovisceral
c. Viscerosomatic
3. Joint dysafferentation
4. Visceral disease simulation
5. Decreased axoplasmic transport
a. Neurodystrophic hypothesis
NERVE COMPRESSION HYPOTHESIS
From the beginnings of the chiropractic profession, the theory that nerves can become compressed through impingement from intersegmental spinal biomechanical derangements has been accorded biomechanical, functional, and clinical significance1314151617181920 and 21 and has even been proposed as a primary cause of disease.1314151617181920 and 21 Chiropractic authors emphasize the importance of the intervertebral foramen (IVF) and its anatomic contents—the spinal nerve, nerve roots, recurrent meningeal (sinuvertebral) nerves, blood vessels, lymphatics, and connective tissue—and devote much attention to changes resulting from compression of the elements within the IVF.131415161718202122232425 and 26
Although contemporary research2728293031 and 32 has demonstrated that other mechanisms of spinal biomechanical derangement may be responsible for inducing neuronal disturbances, the clinical significance of nerve compression should not be discounted. 21 Cramer and Darby22 attribute much of the importance of the IVF to the fact that it provides an osteoligamentous boundary between the CNS and the peripheral nervous system.
The question is: To what extent are spinal nerves, nerve roots, and dorsal root ganglia vulnerable to compression or irritation by abnormal biomechanics affecting the IVF? The anatomy of the lumbar and thoracic spine suggests that sufficient room exists for spinal nerves to pass unimpeded through IVFs in these areas. However, the anatomic relationship of the spinal nerve to the cervical intervertebral foramen is significantly different.
Anatomy of the Cervical Intervertebral Foramen
Orthopedic surgeons DePalma and Rothman23 describe the cervical spine intervertebral foramina as small ovoid canals with vertical diameters approximately 10 mm in height, with the anteroposterior diameter about one half the size of the vertical diameter. The authors state that the “…nerve roots and mixed spinal nerves completely fill the anteroposterior diameter of the intervertebral foramina. The upper one quarter of the canal is filled with areolar tissue and small veins” and “small arteries arising from the vertebra.” DePalma and Rothman continue, “any space taking lesion which pinches the anteroposterior diameter of the intervertebral foramen might be expected to cause some compression of the nervous tissue elements traversing this limited space.” In contrast, these authors describe the normal lumber IVF as five to six times the diameter of the spinal nerve, permitting relatively great freedom from constriction.
Jackson, 24 an orthopedist, in describing the boundaries of the cervical IVF, states:
[The] posterior walls of the canals are formed by the adjacent posterior articular processes, but primarily by the superior articulating process of the distal vertebrae. The anterior walls are formed by the lateral portion of the bodies of the adjacent vertebrae and the margins of the intervening interbody articulations. The anterior walls are of great significance from a mechanical standpoint, in as much as the nerve roots pass directly over and are in intimate contact with the margins of the lateral interbody joints. The gliding motion which occurs between these joints whenever the head and neck are turned or moved in any direction subjects the nerve roots to irritation if there is any mechanical derangement present.
Parallel to the conclusions of Rothman and DePalma, Jackson concludes:
The nerve roots lie on the floor of the canals and fill their anteroposterior diameter completely. The upper one-eighth to one-fourth of the foramina, or the canals, is filled with areolar and fatty tissues and small veins. Small spinal arteries which are branches from the vertebral artery pass back through the intervertebral foramina to enter the vertebral canal. Minute branches from the nerve trunks which are known as the recurrent meningeal nerve pass back through the intervertebral foramina anterior to the nerve roots.
Jackson notes that ventral nerve root fibers are in intimate contact with the margins of the lateral interbody joints. The posterior fibers, or posterior nerve roots, are in intimate contact with the posterior-superior articular processes of the adjacent distal vertebrae. Jackson explains:
[Because] of their close proximity to the anterior and posterior walls of the intervertebral foramina the cervical nerve roots are extremely vulnerable to compression or to irritation from any mechanical derangement or inflammatory condition in or about the foramina. Such irritation or compression may cause pain and/or sensory and motor disturbances anywhere along the segmental distribution of the nerves.
Jackson uses the term cervical syndrome to describe the group of symptoms and clinical findings resulting from irritation or compression of the cervical nerve roots in or about the IVF. 24
Lu and Ebraheim, 33 in dissections of the dorsal root ganglia of the second cervical nerve, found that the dorsal ganglia are all proximally placed and occupy most of the foramen. The cervical ganglia at this spinal level are confined within the foramina between the arch of the atlas and the lamina of the axis. These ganglia occupy 76% of the foramen height. Such anatomic relationships may render the second cervical dorsal ganglion vulnerable to entrapment. These authors further state that trauma with extreme rotation and extension, as occurs in whiplash injuries, at the C1-C2 joint has the potential to crush the second cervical ganglion between the arch of the atlas and the lamina of the axis and may be implicated in cervicogenic headache. Many patients with headache and or neck trauma have a history of motor vehicle accident typical of whiplash. Cervicogenic headache (see Chapter 24) may result from displacement, abnormal movements, or arthritic changes in the atlas-axis articulation, compromising the second cervical nerve root and ganglion. In addition, compressing or entrapping the second cervical ganglion involves fibers that contribute to the greater occipital nerve.
Crelin, 34 an anatomist, in a 1973 article frequently quoted by opponents of chiropractic, argued that nerve roots pass through spacious intervertebral foramina and that therefore exertion of pressure on a spinal nerve does not occur. However, a review of the study’s methodology coupled with current research demonstrates that Crelin’s conclusion is in error concerning the effects of joint subluxation. 35
Seeking to “prove” that the theory of spinal nerve impingement is “impossible,” Crelin34 obtained vertebral columns from six individuals. Three columns were from full-term infants; the others were from adults ages 35, 73, and 76 years. The vertebral column of each was excised within 3 to 6 hours after death. The skull was disarticulated from the first cervical vertebra, and the fifth lumbar vertebra was disarticulated from the sacrum. Each spinal nerve was transected 8 cm after emerging from the IVF. Deep paraspinal musculature, ligaments, and joint capsules were left intact.
Two metal vises were clamped to a platform supported the vertebral column while it was subjected to compressive forces. Five vertebral segments of the newborn column and three of the adult columns were suspended between the vises. A Dillon force gauge was used to measure force of compression applied to the vertebra. A range of maximum compression forces, including twisting and flexion, were applied. The osseous boundary of the foramen did not come in contact with the nerve, and Crelin reported that there was never less than 1.5 mm of space completely surrounding the cervical nerves, 3 mm around the thoracic nerves, and 4 mm surrounding the lumbar nerves. Crelin explained that all spinal nerves emerging from their IVFs were exposed before testing and that gentle teasing with small forceps removed the flimsy areolar tissue surrounding the nerves to expose the border of the “spacious vertebral foramina.”
However, this very tissue that Crelin removed contains important connective tissue elements that may be compressible36 or, when irritated, may release chemicals having an adverse effect on nerve function.37383940 and 41 Some critics of the nerve compression theory have neglected to recognize that spinal biomechanical derangements do not involve “hard bone on soft nerve.” Instead, the key issue is the potential for altered interforaminal mechanics to affect vascular and connective tissue support structures, as well as the important neural components within the IVF.
Contemporary information describes the IVF as an extended interpedicular zone, 42 often containing transforaminal ligaments.43444546 and 47 These anatomic factors, combined with current understanding of spinal nerve root sensitivity to pressure4849 and 50 and irritation,3738394041 and 51 render Crelin’s conclusions unsupportable. 52
Interpedicular Zone
Giles42 maintains that the IVF should no longer be conceptualized as a two-dimensional hole, but rather as a canal or tunnel through which the spinal nerve and other related structures pass. Giles maintains that “neural and associated vascular structures within the important interpedicular zone may well be compromised due to vertebral joint subluxation. This may result in chronic compression,” adding, “The precise significance clinically… is yet to be determined.”
Giles took nine randomly chosen sections of adult lumbosacral spinal tissue and examined them histologically for measurement of the L4-L5 and L5-S1 IVF canals. The zone between the pedicles of adjacent vertebrae was found to have a horizontal length of 8.2 to 12.2 mm. At a minimum, the distance between the nerve structures and the side of the IVF canal was 0.4 to 0.8 mm for both the L4-L5 and L5-S1 segments. Giles concludes that the Crelin study was “meaningless as a basis for consideration of the possible physiological and/or pathophysiological functions of spinal nerves beyond the intervertebral canal as he did not examine the important interpedicular zone.” that contains the spinal nerve root and ganglion. Rather, he examined only “the relatively insignificant lateral border.”
Transforaminal Ligaments—A Key Anatomic Structure
As described by Golub and Silverman, 43transforaminal ligaments (TFL) are ligamentous bands crossing the IVF at any spinal level (Fig. 8-1). In dissections of 15 lumbar spines representing 150 IVFs, Bachop and Hilgendorf44 found varying numbers of TFLs. Bakkum45 determined that TFLs, once considered an abnormality, are normal and greatly reduce the functional compartment or space available for the spinal nerve. In Bakkum’s study, four adult lumbosacral spines without visible pathology or degenerative changes were examined, yielding the following results: 35 of the 49 IVFs examined (71%) had at least one TFL. More than one quarter (27%) had two TFLs, and 8% had three or four.
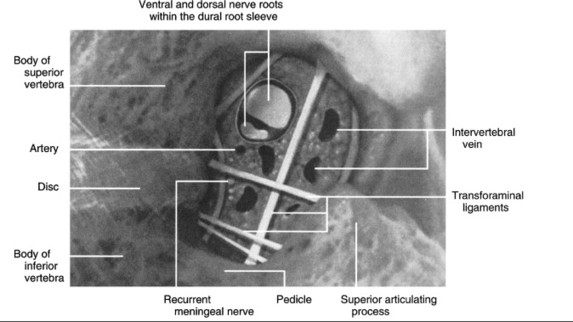 |
| Fig. 8-1 Transforaminal ligaments. (From Cramer G: Clinical anatomy of the lumbar region and sacroiliac joints. In Greenstein G, editor: Clinical assessment of neuromusculoskeletal disorders, St Louis, 1996, Mosby; with permission. Illustration by Dino Juarez, the National College of Chiropractic.) |
In the presence of TFLs, the superior-to-inferior dimension (height) of the functional compartment containing the ventral ramus of the spinal nerve was significantly decreased. The average height reduction was approximately one third (31.5%). In 12%, the reduction was at least 50% in the IVF containing a TFL, with one case being reduced by over two thirds (67.8%).
According to Bachop and Janse, 46 the higher the TFL is situated in the foramen, the less space remains for the spinal vessels. This anatomical relationship can conceivably lead to ischemia or venous congestion. On the other hand, the lower the TFL is located, the greater the possibility will be of sensory deficits, motor deficits, or both. In a study of accessory ligaments of the IVF, Amonoo-Kuoffi and colleagues47 conclude that the spinal nerve, segmental veins and arteries, and the recurrent meningeal nerve are held in place through the openings between the accessory ligaments within the IVF. In IVFs in which multiple TFLs are present, these nerves and vessels are literally threaded through a lattice created by the TFLs.
Hadley on Subluxation and the Intervertebral Formen
Hadley, 51 a medical radiologist, states that the importance of the IVF lies in the fact that, except for the first and second cervical nerves, each peripheral nerve must pass through one of these openings. The cervical region contains “a close five-way interrelationship between the foramen, the nerve root which passes through it, the vertebral artery contacting the root in front, the co-vertebral joint anteriorly and the posterior cervical articulation in back.” Hadley also notes that arthrotic and degenerative changes involving these structures may become an important factor resulting in foraminal encroachment and that, “bulging disc substance, exostoses or subluxation of a posterior joint may produce pressure upon the root.”
Hadley51 goes on to state: “Subluxation (partial displacement) of the vertebral bodies …may present radiographically one or more of the following features:
1. Shift of the corresponding spinous process toward the side of the subluxation with the patient and film exactly centered
2. Slight increase in the size of the corresponding intervertebral foramen
3. Encroachment of the opposite foramen
4. Displacement of the articular surfaces upon each other
5. Because of the inclined plane of the posterior articulation, the side of the vertebra is elevated as it is carried forward. For that reason the disc appears thicker on the side of the unilateral subluxation.”
Regarding cervical encroachment, Hadley51 observes that, in addition to local and referred pain, patients can suffer from bizarre symptoms called chronic cervical syndrome. These symptoms are described as paroxysmal deep or superficial pain in parts of the head, face, ear, throat, or sinuses; sensory disturbances in the pharynx; vertigo; and tinnitus, with diminished hearing. Vasomotor disturbances include sweating, flushing, lacrimation, and salivation. Hadley adds, “spontaneous subluxation at the C1-C2 level either unilateral or bilateral, is usually a sequel to an inflammatory process of the throat.”
Hadley’s observation of spontaneous subluxation associated with inflammation of the throat raises interesting questions from a chiropractic perspective. Is this inflammatory process truly a viscerosomatic reflex response, or are these symptoms a result of somatovisceral manifestations leading to lowered tissue resistance in the throat that contribute to the inflammation?
In a study of 76 children with chronic tonsillitis, Czech physician and manual medicine specialist Lewit53 observed, “The most striking and constant clinical finding was movement restriction at the craniocervical junction, in the great majority between occiput and atlas (70 cases or 92%).” Lewit concluded that “tonsillitis goes hand in hand with movement restriction… mainly between occiput and atlas, with little tendency to spontaneous recovery,” adding, “our experience suggests that blockage (movement restriction) at this level increases the susceptibility to recurrent tonsillitis.”
Commenting on the thoracic region, Hadley51 states, “Since the thoracic roots are relatively small, compression of these structures does not occur in the foramina of this region.” Regarding the lumbar region, Hadley affirms that the spinal nerve occupies approximately one fifth to one fourth the diameter of the normal foramen. The remainder of the space is taken up by blood and lymphatic vessels, areolar, and fatty tissue, which together constitute a “compressible safety cushion space which allows the physiological encroachment to occur without nerve compression.” Moreover, “any abnormal constriction in the size of a normal IVF if not actually causing nerve root pressure, nevertheless decreases the reserve safety cushion space surrounding that nerve and may predispose to pressure.”
Effects of Degeneration
In a study of the kinematics of the lumbar IVF under normal physiologic spinal motions, Panjabi and colleagues54 maintain that in cases of spinal degeneration, normal physiologic motion “may be enough to compromise the space around the nerve root to such a degree that very little safety margin is left.” These authors further state:
[With] age and degeneration, the nerve loses its flexibility and develops adhesions with the IVF walls. It may not easily slip away from the compressing forces. The result may be a chronic threat of compression and mechanical irritation leading to inflammation of the nerve root.
Panjabi, discussing the research of Sunderland, 48 agrees that “in contrast to the thicker connective tissue covering of the peripheral nerve, the anatomical and mechanical weakness of the spinal nerve root more easily causes interneural fibrosis and adhesions to the surrounding IVF tissues.”
Muscular Influences on Nerves
Korr, 55 a physiologist and osteopathic researcher, observes that much of the pathway taken by nerves as they emerge from the cord is through skeletal muscle. The contractile forces of this muscle along with associated chemical changes exert profound influences on the metabolism and excitability of neurons. In such an environment, neurons are subject to considerable mechanical insult (compression and torsion), as well as chemical influences. Nerve sheaths, which are extensions of the meninges surrounding the spinal cord, extend distally along the spinal nerve roots, providing a root sleeve that allows the nerves to slide smoothly in and out without friction during a wide range of vertebral column movement. Over time, however, slight mechanical stresses may produce adhesions, constrictions, and angulations. From a chiropractic prospective, this vulnerability of nerve trunks represents effects associated with the myologic component of the VSC and also relates to its inflammatory and biochemical components.
Vascular and Sympathetic Influences
Vascular structures pass through the IVF and provide blood supply to both the bony vertebral column and the spinal cord. 56 Ischemia of the nerve cells within the dorsal root ganglia may lead to progressive loss of sensory function, including proprioception. Edematous pressure from even slight congestion of venous drainage may affect nerve conduction. 56 Such relationships are associated with the vascular and neurologic components of VSC. Olmarker and colleagues, 56a in studying the effects of experimental compression on intraneural capillary and venular blood flow through tracking the intraneural transport of tracer-labeled glucose, determined that as low as 10 mm Hg pressure applied to the dorsal roots reduced nutritional transport to the peripheral axons to 20% to 30%.
Sympathetic ganglia in the highly mobile neck area and the cervical chain of ganglia positioned against the vertebral column are subject to stress imposed by motion. This stress may exert profound influence on the physiology of sympathetic nerve cells. Furthermore, the mechanical disturbances or somatic insults previously described by Korr exert slight forces resulting in slight tissue changes within the IVF and in paraspinal structures. This condition may adversely affect nerve function. A further proposal asserts that disorders of muscle tension, tissue texture, and visceral and circulatory function are reflected at the body surface as observable diagnostic elements. 49,50
Neurophysiologic Effects of Nerve Compression
Spinal nerve roots, as compared with peripheral nerves, have a less abundant protective epineurium, no branching fasciculi, and poor lymphatic drainage.5657 and 58 These facts imply that the nerve root is more susceptible to injury by mechanical forces. 59 Panjabi and colleagues54 state that “the nerve root is constrained in the intervertebral foramen and may be easily compressed or mechanically irritated under adverse conditions of degeneration and movement.” In consideration of the effects on nerve function by subluxation or spinal biomechanical impairment, questions arise regarding possible pathophysiologic mechanism associated with compression or mechanical irritation of nerves.
Sharpless, 60 in a study to determine the susceptibility of spinal nerve roots to compression, concluded:
[Pressure] of only 10 mm Hg produced a significant conduction block, the potential falling to 60% of its initial value in 30 minutes. After such a small compressive force is removed, nearly complete recovery occurs in 15 to 30 minutes. With higher levels of pressure, we have observed incomplete recovery after many hours of recording.
Rydevik61 determined:
Venous blood flow to spinal roots was blocked with 5–10 mm Hg pressure. The resultant retrograde venous stasis due to venous congestion is suggested as a significant cause of nerve root compression. Impairment of nutrient flow to spinal nerves is present with similar low pressure.
Konno and colleagues62 reported that compression of cauda equina nerve roots decreased action potentials with as little as 10 mm Hg of pressure. Hause63 proposed a mechanism of progression in which mechanical changes lead to circulatory changes, after which inflammatogenic agents produce chemical radiculitis. This action, in turn, leads to disturbed flow of cerebrospinal fluid, with defective fibrinolysis and subsequent cellular changes. In addition, the influence of the sympathetic system may result in synaptic sensitization of the central and peripheral nerves, creating a vicious circle, resulting in radicular pain. Hause also proposes that compressed nerve roots can exist without causing pain.
Mechanical Tension and the Muscle-Dural Connection
Mechanical tension on the pain-sensitive dura mater may contribute to headache. Hack and colleagues64 found that the rectus capitis posterior minor muscle extends from the occiput to the posterior arch of the atlas vertebra and connects via a bridge of connective tissue to the spinal dura. This connection may resist inward folding of the dura, which may compromise cerebrospinal fluid flow when the neck is extended. The dura is extremely sensitive, and tension applied during surgery is felt as headache. The muscle-dura connection may transmit forces from the neck muscles to the pain-sensitive area of the dura. This muscle-dura connection may represent an anatomic basis for the effectiveness of manipulation/adjustment, which may decrease muscle tension and reduce pain by reducing the forces between C1 and C2 involving the rectus capitis posterior major and oblique capitis inferior muscles (see Fig. 23-5, p. 479).
ABERRANT SPINAL REFLEX HYPOTHESES
A basic chiropractic hypothesis holds that abnormal spinal biomechanics and muscle dysfunction have effects, via the nervous system, throughout the body and that the chiropractic adjustment is applied not only to restore range of motion and alignment, but also to cause or relieve reflex effects in the nervous system. In this respect, the chiropractor functions not only as an engineer (correcting joint function), but also as a telecommunications specialist (influencing spinal reflexes and nerve function). 35
Except for skilled movements, body functions are largely reflexive. Examples include heartbeat, respiratory movements, digestive activity, and postural adjustments. Reflexive responses to stimuli include muscular contraction and glandular secretion. These spinal reflexes, which are involuntary responses to stimuli, are purposeful and exist to regulate physiologic functions, including somatic, autonomic, and endocrinologic processes. A reflex arc consists of a stimulus-activated receptor, transmission over an afferent pathway to an integration center, transmission over an efferent pathway to the effector, and induction of a reflex response65 (Fig. 8-2).
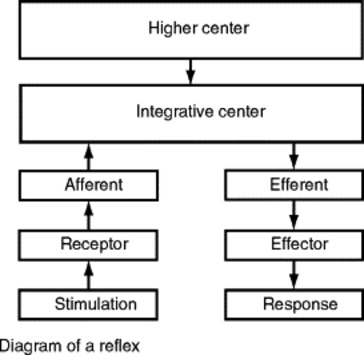 |
| Fig. 8-2 Diagram of a reflex. (From Haldeman S: Principles and practice of chiropractic, ed 2, East Norwalk, Conn, 1992, Appleton & Lange; with permission.) Appleton & Lange |
Reflexes can be divided into four types based on the contributions of somatic and autonomic nerves to the efferent and afferent pathways of the reflexes. These reflexes include (from Sato65):
1. Somatosomatic: Reflexes whose afferents and efferents are somatic nerve fibers
3. Somatovisceral (also termed somatoautonomic): Reflexes whose afferents are somatic sensory fibers and whose efferents are autonomic efferent fibers
4. Viscerosomatic (also termed visceromotor reflexes): Reflexes whose afferents are visceral sensory fibers and whose efferents are somatic motor nerve fibers
It is proposed that joint subluxation or biomechanical impairment can, however, alter these reflexes adversely. Korr27286667 and 68 conducted much of the basic clinical research demonstrating that prolonged nerve excitability, sustained hyperactivity of afferent receptors, and reflex response were associated with movement restriction in the spine. Korr reported evidence of heightened reflexive reactivity at spinal cord levels associated with palpable osteopathic lesions and observed reliable increases in galvanic skin response (GSR) readings at specific cord levels that he termed facilitation, the facilitated segment, or the facilitated lesion.
A fundamental hypotheses of both osteopathy and chiropractic is that locally altered somatovisceral reflexes associated with traumatized spinal joints evoke a vicious cycle of altered afferent and efferent impulse traffic, therefore leading to a facilitated or hyperactive spinal segment.2728666768 and 69
As presented by Dhami and DeBoer, 70 this hyperactivity is proposed to further alter neural activity, both segmentally and centrally, within the cord, resulting in increased local somatic tissue changes with altered joint function and tissue texture, along with muscle splinting, tenderness, and temperature changes. This facilitated segment at a specific spinal level is proposed to lead to altered sympathetic and parasympathetic outflow affecting local vascularity and ongoing neural and visceral activity. 71
Spinal adjustment, manipulation, mobilization, and pressure point therapy are proposed by Korr55 to influence these sustained and facilitated spinal reflexes in the following ways:
1. Directly, as a reflex therapy in itself, in that the adjustive/manipulative or mechanical intervention introduces a stimulus to joint and muscle receptors producing a reflex response that modifies or inhibits the current facilitated reflex activity, thus reducing pain and causing relaxation of paraspinal muscles
2. Indirectly, in that the manual procedure normalizes joint mechanics, thereby removing spinal joint and muscle dysfunction that produces abnormal levels of spinal reflex activity that resulted in the facilitated lesion at a given spinal segment
Akio Sato, 65 a medical physician and researcher in the area of spinal reflex physiology, states:
Manipulation performed by chiropractors excites somatic afferent fibers in the musculoskeletal structures of the spine. These afferent excitations may, in turn, provoke reflex responses affecting skeletal muscle, autonomic, hormonal, and immunologic functions. An understanding of spinal reflex physiology is, therefore, fundamental to comprehending the effects of manipulation.
VARIETIES OF SPINAL REFLEXES
Three major types of spinal reflexes—somatosomatic, somatovisceral, and viscerosomatic—are referred to extensively in chiropractic, osteopathic, and medical literature. The order in which the root words are combined indicates the origin of the reflex and the site of its effect, respectively. For example, somatovisceral denotes that the initial stimulus or insult to the nervous system was a somatic receptor as in a spinal joint and that the efferent reflexive manifestation or response is expressed in a visceral tissue or organ.
Aberrant Somatosomatic Reflex Hypothesis
In Greek, soma means “body.” In the somatosomatic reflex hypothesis, stimulus at one level of the soma or musculoskeletal system produces reflex activity in the nervous system, which is then exhibited elsewhere in the musculoskeletal system. The knee-jerk reflex is an example of a somatosomatic reflex. A light tap on the patellar ligament activates stretch receptors located within that ligament and in the tendon of the quadriceps muscle, which inserts on the patella. Impulses are conducted by sensory (afferent) neurons to the CNS, specifically at the intersegmental L3 and L4 levels, where these neurons synapse with motor neurons in the gray matter of the spinal cord. Without conscious involvement of the brain, impulses are then conducted by motor (efferent) neurons back to the quadriceps muscle. The muscle contracts in response to the impulses traveling along its motor nerve.
In this example, a stimulus was applied to a receptor in a somatic structure, eliciting a response in another somatic structure. Similarly, stimuli to receptors in spinal structures, whether from abnormal joint or muscle tension or from chiropractic adjustment72 or manipulative treatment30,31,73,74 to relieve it, cause various spinal reflex responses in the musculoskeletal system.
The interneurons of the dorsal horn are proposed to be involved in pain inhibition. As an example, strong tactile stimulation, as in skin rubbing, has long been known to diminish sensations of dull aching or sharp pain originating from an injured area. This decreased sensation is the result of the effect of afferent inhibition or the gate control theory. The mechanical intervention of rubbing activates the large, fast-conducting tactile-or touch-responsive A-alpha fibers (mechanoreceptors), which, in turn, inhibit the synaptic transmission of the pain signals by blocking the synaptic gates normally used by the smaller C-fibers that convey pain signals, therefore suppressing the signals of pain.
Wyke3031 and 32 suggested that spinal manipulation stretches mechanoreceptors in the joint capsule and that this stimulus has an inhibitory effect, mediated through spinal cord interneurons, on nociceptive activity. Increased mechanoreceptive input from increased joint motion reduces, or closes, the gate on pain signal transmission. This proposed mechanism is an adaptation of Wall’s gate control theory. 75
A subcomponent of the somatosomatic reflex model, referred to as the proprioceptive insult hypothesis26,76,77 suggests that receptors in the highly innervated soft tissue in and around joints may become irritated, leading to reflex modifications in postural tone and neural integration of postural activities. The proprioceptive insult hypothesis has been described in chiropractic writings78,79 as undue irritation and stimulation of sensory receptors (including proprioceptors) located in the articular structures and in the parasegmental spinal ligaments. This irritation may result when structures are under stress from derangement of the intervertebral motor units caused by subluxation. Janse26 proposes that the afferent barrage of impulses into the nervous system may disturb equilibrium, create somatosomatic reflexes, and cause aberrant somatovisceral and somatopsychic reflexes.
Reflex muscle spasm is another example of a somatosomatic reflex. 80 This reflex has been associated with the facilitated segment, in which muscle spasm may result from and contribute to proprioceptive irritation. Theories80 suggest that the spinal cord segments in the vicinity of a spinal fixation have a lower threshold for firing and therefore are neurologically hyperexcitable. Korr refers to this concept as the facilitated lesion. 81,82
Aberrant Somatovisceral Reflex Hypothesis
The Latin meaning of viscera is internal organ. In this concept, a stimulus to nerves or receptors related to spinal structures produces reflexive responses influencing function in the visceral organs, such as those in the digestive, cardiovascular, or respiratory systems. Alternate terms for this form of spinal reflex are somatosympathetic and somatoautonomic.
Lewit, 53 in a review of vertebrovisceral relations in a variety of cases, cites an example in which changes in spinal function (joint blockage or hypomobility) are linked to tachycardia. Therefore when mobility of the spinal column is normalized, heart rhythm also becomes normal and remains so as long as no relapse occurs in spinal column dysfunction. Lewit states that “although direct evidence of disturbed motor function causing organic heart disease is lacking, it would seem reasonable to grant it the role of a possible risk factor.” Lewit uses the term blockage to describe spinal movement restriction, noting that the characteristic pattern of spinal hypomobility in ischemic heart disease is “blockage affecting the thoracic spine from T3 to T5, most frequently between T4 and T5, movement restriction being most noticeable to the left, and at the cervicothoracic junction.” Of historical relevance is that as early as the 1920s, chiropractic authors such as Vedder83 and Firth84 recommended adjustment of Heart Place, identified as the second and third dorsal vertebral segments, for treating tachycardia.
Somatovisceral Studies—Hypertension, Dysmenorrhea, Infantile Colic, and Female Infertility
In a 1988 randomized controlled trial involving 21 hypertensive patients, Yates and colleagues85 observed significant short-term (1–10 minutes) decreases in systolic and diastolic blood pressure in the chiropractic adjustment group, although no significant change was noted in the placebo and control groups. Adjustive procedures were applied to the T1 through T5 spinal levels. Kokjohn and colleagues, 87 in a study of 45 subjects, including experimental and sham manipulation control groups, concluded that spinal manipulative therapy may be an effective and safe nonpharmacologic alternative for relieving the pain and distress of primary dysmenorrhea.
Hondras and colleagues, 139 in a larger follow-up to Kokjohn and colleagues’ dysmenorrhea study, failed to find significant differences in pain (as measured by visual analog scales), disability (as measured by questionnaire), or serum prostaglandin levels of patients with dysmenorrhea receiving side posture manipulation versus patients receiving a sham procedure. Patients in both the manipulation and sham groups demonstrated mild improvement. (See Chapter 25 for more detailed discussion of this and other chiropractic research studies on somatovisceral disorders.)
In a prospective study of 316 cases of infantile colic treated by chiropractors, Klougart and colleagues87 found satisfactory results in 94% of cases within 14 days from the start of chiropractic care. The authors found that chiropractic treatment resulted in “both a reduction of the daily length of colic periods and a reduction of the number of colic periods per day.” Because recovery began between 5.7 and 7.7 weeks of age, the authors maintained that this finding provided substantial evidence that the improvement might not be attributed strictly to “natural cessation of colic symptoms.”
In a 1999 study, Wiberg, Nordsteen, and Nilsson88 found that “spinal manipulation has a positive short-term effect on infantile colic.” Researchers randomly placed otherwise healthy, colicky infants into either a chiropractic treatment or a dimethicone medication group. Parents maintained a diary of symptoms and behaviors before and during the trial. Both groups received 2 weeks of treatment. The infants in the chiropractic group exhibited a “reduction of 67% on day 12” of daily hours with colic (nearly identical to the study by Klougart and colleagues87). The “dimethicone group only had a reduction in daily hours with colic of 38% by day 12.” The authors noted:
[Manipulation] is normally used in treatment of musculoskeletal disorders, and the results of this trial leave open two possible interpretations. Either spinal manipulation is effective in treatment of the visceral disorder infantile colic or infantile colic is, in fact, a musculoskeletal disorder, and not as normally assumed, visceral.
Volejnikova, 59 in concert with Karel Lewit, conducted a randomized trial involving women referred for medical rehabilitation for infertility. The study population consisted of 166 women between the ages of 22 and 30, with normal sperm partners and patency of the fallopian tubes. The women in all groups had received unsuccessful infertility treatment for an average of 4 years. These women were randomly allocated to five different groups. Two treatment groups received procedures termed Majzisova’s Protocol, directed to the lumbar spine and pelvis, which included stretching and relaxation of lumbar and pelvic musculature, postisometric relaxation of the gluteal and pelvic floor muscles, and other exercises. In the first half of the menstrual cycle, a physiotherapist performed mobilization of hypomobile areas of the sacroiliac joints, lumbar spine, and ribs. Home exercises were also prescribed.
Typical symptoms other than infertility were painful menstruation, bleeding with clots, dyspareunia (painful coitus), back pain, and headache. On examination, frequent structural and somatic manifestations included bad posture, scoliosis, sacroiliac dysfunction, asymmetry of the intergluteal line, gluteal and levator ani muscle weakness, and tenderness of coccyx, sacroiliac joints, and lumbar erector spinae. The course of treatment ended after six visits and was considered successful if pregnancy occurred within the study period. Other subject groups were assigned active and passive exercises or other nontreatment interventions. The two treatment groups experienced 34.3% and 27.4% success rates for pregnancy, compared with 8% to 9% success rate for each of the three minimal or nonintervention control groups.
Pikalov Study on Duodenal Ulcers
Going beyond the consideration of visceral dysfunction and observing the effects of spinal adjustment or manipulation on structural visceral pathology, Pikalov and Vyatcheslav90 in a 1994 study demonstrated improved remission rates of actual pathologic conditions in patients with observable duodenal ulcer. The statistically significant results suggest that spinal somatic dysfunction predisposes the duodenum to disease and is a cause of the true visceral disease and pathologic conditions. Andrei Pikalov, who conducted this study, is a medical physician and physiology researcher, formerly of the Medical Research Institute at the Russian Ministry of Internal Affairs in Moscow and a former member of the research faculty of Cleveland Chiropractic College, Kansas City.
In this study, 35 adults attending the Gastroenterological Department at Moscow Central Hospital with acute, uncomplicated duodenal ulcer confirmed by endoscopic examination were examined for vertebral subluxation. Twenty three participants demonstrated characteristics of subluxation, that is, displacement, spinous process tenderness, restricted motion, contracture, and painful paravertebral muscles. Spinal segments T9 through T12 were the most frequently affected. This finding again coincides with the writings of chiropractors Vedder84 and Firth, 84 who in 1920 associated duodenal ulcer with subluxation of T9.
In the Pikalov study, patients were assigned to either a standard medical management group or a spinal manipulation group. Patients in the medical group received standard drug therapy and dietary regime over 4 to 7 weeks. For the other group, a course of spinal manipulation up to 14 treatments over a 3-week period was undertaken along with the standard dietary regime. Remission or healing took an average of 16.4 days in the manipulation group, approximately 9 days or 40% faster than the 25.7-day average in the medical group. The principal outcome, confirmed by endoscopic examination, was full clinical remission of the ulcer in terms of smooth healing of the lining of duodenum (epithelialization) or healing by scar formation (cicatrization). Pain resolved in 3.8 days on average in the manipulation group. The authors speculate that possible mechanisms to explain their results include “normalization of the action of the autonomic nervous system which influences both cellular metabolism and the vasomotor dynamics of the stomach and duodenum” and “stimulation of the endogenous opiate system.”
These patients did not have simulated or pseudoulcer (visceral disease simulation is discussed later in this chapter) but actually exhibited endoscopically observable duodenal ulcers, confirmed by photographs. The manipulation applied to relieve somatic or spinal dysfunction not only relieved the pain, but also apparently provided a healing effect significantly superior to that obtained from standard drug therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







