The ability to adapt to changing conditions is another trait of living organisms. In humans, this ability takes the form of maintaining balance while negotiating changing or uneven terrain (or sometimes even while standing or sitting still) or while responding to various external stimuli (e.g., antigens, emotional stresses, the occasional life-threatening event).
Postural adaptations are accomplished through a system that can be referred to as the equilibrial triad. This system is composed of three elements: (1) the proprioceptive system, found throughout the body in the Golgi tendon organs (GTOs), the muscle spindles, and the nerves that innervate these receptors; (2) the vestibular system, found in the inner ear, which signals the nervous system regarding the position of the head; and (3) the visual system.
Adaptations to antigenic challenges are primarily mediated thorough the immune system. However, as more evidence accumulates, the immune system is clearly interrelated with and is heavily influenced by both the endocrine and nervous systems.
Responses to other forms of stress are processed through the autonomic nervous system, which is discussed in some detail later in this chapter. Understanding this system, how it innervates the viscera, and its interplay with the somatic nervous system (that which innervates the muscles, joints, fascia, and skin) is absolutely crucial to the informed practice of the adjustive/manipulative arts.
Familiarity with the principles of tensegrity will provide a more thorough understanding of the operation of the musculoskeletal system and the proper maintenance of posture and balance. Tensegrity is a concept originated by the artist Kenneth Snelson and the architect Buckminster Fuller, which posits a balance of compressional and tensional forces through a body that exists in a gravitational field. Simplistically speaking, the bones and disks of the vertebral column are built to withstand compressional forces, and the muscles and ligaments are the tensional elements of the axial skeleton. In addition, the tensional elements are preloaded (i.e., muscle tone and connective tissue tension are at rest), which adds to the stability of the system. When compression and tension are in balance, an upright posture can be maintained with a minimum of work. Within this framework, the words origin and insertion will not be used to describe the attachments of the muscles. These common terms have been used over the years based on certain assumptions of the kinetics of the body. Specifically, the word origin has been used to describe a more proximal or stable attachment, and insertion is ascribed to the distal or mobile attachment of a muscle. However, especially relative to the muscles that influence the spine, an important point to realize is that either muscle attachment can produce movement, sometimes simultaneously, and thus it is believed that these two terms are too limiting.
The embryologic development of the human organism establishes a time line for the early period of life. A basic knowledge of this early history allows for a more thorough understanding of the ultimate arrangement of the human body, as well as the existence of anatomic variations and, in some cases, birth defects.
Wolff’s law is a concept with which all students of anatomy should be familiar. Wolff’s law simply states that when stress is placed on a bone, it undergoes a tissue reaction whereby its form may change to fit its function. An important point to remember is that bone is living tissue, and as such, it will react to stress and its local environment. An example of this phenomenon is the difference in size and shape of the vertebrae of a large, physically active man, compared with a small, inactive woman. The vertebra of the man would bear more weight and be subjected to greater stresses. Therefore the vertebral body would be larger, and the processes would be longer and perhaps broader and thicker, given that the muscles attached to these parts of the vertebra would be pulling harder to perform more work. This concept, although not specifically stated, can also be extended to soft tissues, such as ligaments, tendons, and other connective tissues, which also respond to the forces placed on them.
The various rhythms and oscillations of the body are also important for the clinician to appreciate. Most notable are cardiorespiratory rhythms and the (hopefully unimpeded) movement of the diaphragms of the body. These rhythms can be exploited in manual procedures to the advantage of both the clinician and the patient.
VERTEBRAL COLUMN AS A WHOLE
Anatomically, the human body is arranged lengthwise as a series of building blocks or segments. This arrangement can be observed most directly by looking at the individual vertebrae that make up the spinal column, which extends from the base of the skull to the “tail bone,” or the coccyx. Just above the coccyx is the sacrum, which is a single bone resulting from the fusion of five vertebrae. This fusion is significant because the sacrum articulates with the pelvic bones that, in turn, articulate with the femurs. This relationship produces an arch, which has the sacrum as its keystone.
The spine, or vertebral column, is usually composed of 33 individual vertebrae. Proceeding from superior to inferior, these vertebrae are 7 cervical, 12 thoracic, 5 lumbar, 5 fused vertebrae forming the sacrum, and 4 rudimentary vertebrae, usually fused, forming the coccyx (Fig. 4-1).
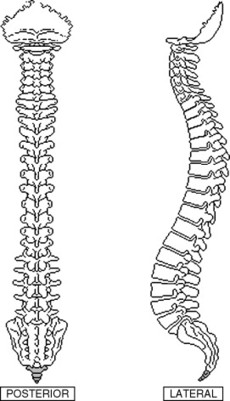 |
| Fig. 4-1 Posterior and lateral views of the spine. |
Each region of the spine is curved in the sagittal (front to back) plane of the body. The cervical and lumbar regions are curved with a posterior concavity, referred to as lordosis, or a lordotic curvature. The thoracic and sacral regions possess an anteriorly concave curvature, referred to as kyphosis, or a kyphotic curvature. Both of these curvatures exist within a normal range. However, curvatures outside the normal range will be seen. For example, excessive thoracic kyphosis (hyperkyphosis) is commonly referred to as hunchback (especially when combined with scoliosis, as described later), and excessive lumbar lordosis is commonly referred to as swayback.
Under ideal conditions, the spine is vertical in the frontal (side-to-side) plane of the body. Lateral curvatures are referred to as scoliosis and can exist separately or in combination with hyperkyphosis (hunchback) or hyperlordotic curves.
The curvatures of the spine are sometimes referred to as primary and secondary. Early in embryonic development, the spine is C-shaped (Fig. 4-2), that is, a single kyphotic curve (primary). As time passes, the spine gradually straightens, until at birth, two secondary lordotic curves begin to appear in the cervical and lumbar regions (secondary). As the infant learns to raise and hold his or her head erect with the supporting muscles of the neck, the cervical lordotic curve is enlarged. Later, as the infant learns to stand and walk, the lumbar lordosis is enhanced as a result of the activity of the posterior spinal musculature.
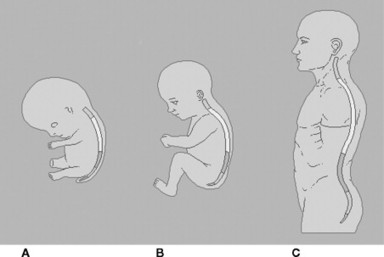 |
| Fig. 4-2 Development of the curvatures of the spine; A, fetus; B, infant; C, adult. |
FUNCTIONAL SPINAL UNIT
The functional spinal unit (FSU) includes two adjacent vertebrae and the joints that link them, as well as the skeletal muscles that move the joints. The FSU is closely related to the body segment (see the Embryonic Segmental Development section in this chapter), which also includes the spinal nerves, blood and lymphatic vessels, and fascia. Other bones, muscles, and associated fascia (e.g., ribs, intercostal muscles in the thoracic region), as well as visceral structures within the body cavities that receive innervation from the autonomic portion of the spinal nerves, should also be considered elements of individual segments.
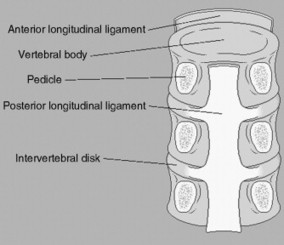
VERTEBRAL CHARACTERISTICS
Although the vertebrae vary considerably in size and shape from region to region and within specific regions, certain characteristics are common to all (Fig. 4-3). Each structure has an anterior body and a posterior vertebral arch, or neural arch. The arch consists of four elements: the pedicles, the transverse processes, the laminae, and the spinous processes. The pedicles, which are short and stout, attach to the vertebral body posterolaterally. The pedicles form part of the boundaries of the intervertebral foramina through which pass the spinal nerves and other structures (see later discussion). The transverse processes, which extend laterally from the ends of the pedicles, are of varying length. The laminae, which are generally broad and flat, project posteromedially from the transverse processes or pedicles. The spinous processes, which extend posteriorly from the midline junction of the laminae, are of varying length, shape, and angulation and can, in many cases, be easily palpated.
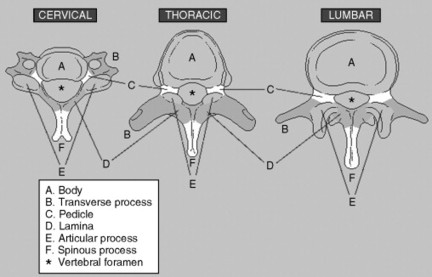 |
| Fig. 4-3 The parts of the vertebrae. |
The posterior aspect of the vertebral body and vertebral arch forms the vertebral foramen. The collective group of vertebral foramina creates the vertebral or spinal canal, which contains the spinal cord and related structures.
Projecting in both superior and inferior directions from the laminae are the superior and inferior articular processes, which form part of the synovial joints with the vertebrae above and below. The angle of the joint plane is of great significance because it will direct the motion of the FSU.
The vertebrae develop from the embryonic sclerotome (see later discussion), which contains several specific elements that are common to all vertebrae. The vertebral body corresponds to the centrum (or central element, Fig. 4-4). The pedicles, base of the transverse processes, laminae, and spinous processes correspond to the neural arch element. The transverse elements form the transverse processes. In addition, costal elements may be found, which in the thoracic region become the ribs but which also persist in other regions and will be described later. The costal element is often overlooked, especially in the cervical and lumbar regions. The costal element makes up the anterior portion, including the anterior tubercle of the cervical vertebra, and forms the majority of the transverse processes of the lumbar vertebra, as well as the anterior portion of the ala of the sacrum. The costotransverse foramen exists solely in the cervical and thoracic regions. The significance of the costotransverse foramen in the cervical vertebrae is the formation of the foramen transversarium for the passage (and presumably for the protection) of the vertebral artery. Failure of midline fusion of the posterior arch results in spina bifida, a potentially serious condition.
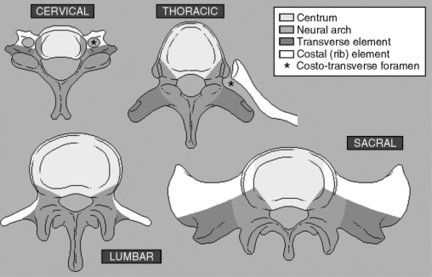 |
| Fig. 4-4 Developmental origins of the vertebrae. |
SUPPORTING STRUCTURES
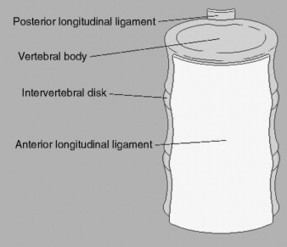
Anterior Longitudinal Ligament
The anterior longitudinal ligament (Fig. 4-5) is broad and thick. Extending from the basilar portion of the atlas to the sacrum, the ligament attaches to the anterior surfaces of the vertebral bodies and intervertebral disks. Superiorly, the anterior longitudinal ligament extends from the anterior arch of the atlas to the occiput as the anterior atlanto-occipital membrane and inferiorly as the anterior sacrococcygeal ligament. The anterior longitudinal ligament limits anterior protrusion of the intervertebral disks and hyperextension of the spine. This ligament is prone to damage in whiplash-type injuries in which the spine is hyperextended as a result of rapid acceleration (or a blow from behind).
 |
| Fig. 4-5 The anterior longitudinal ligament. |
Posterior Longitudinal Ligament
This ligament is found on the posterior surfaces of the vertebral bodies and intervertebral disks. Within the vertebral canal, the posterior longitudinal ligament (Fig. 4-6) is much narrower than the anterior longitudinal ligament. Extending from the axis to the sacrum, this ligament is continuous superiorly with the tectorial membrane and inferiorly with the deep dorsal sacrococcygeal ligament. Lateral extensions of the posterior longitudinal ligament exist at the level of the intervertebral disks. The posterior longitudinal ligament prevents posterior protrusion of the intervertebral disk and spinal hyperflexion.
 |
| Fig. 4-6 The posterior longitudinal ligament. |
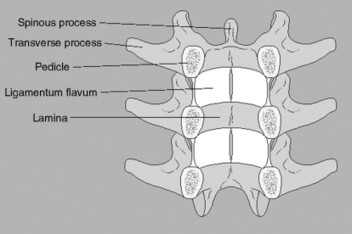
Ligamentum Flavum
These ligaments (Fig. 4-7) are found extending from the articular process to the spinous process and connect adjacent vertebral laminae and attach to the anterior surface of the lamina above and the posterior surface of the lamina below. The word flavum (L. for yellow) is used to describe these ligaments because of their yellow coloration resulting from the predominance of elastic tissue. These ligaments are the most important of the posterior ligaments in limiting flexion of the spine.
 |
| Fig. 4-7 The ligamenta flava. |
The anterior fibrous joints (symphyses) between the vertebral bodies are formed by the intervertebral disks (Fig. 4-8). The disks are found between the vertebral bodies from the C2-C3 to the lumbosacral junction. A small, rudimentary disk also exists between the sacrum and coccyx and possibly between caudal coccygeal segments. The intervertebral disk consists of two basic components: a central, gelatinous nucleus pulposus (a remnant of the embryonic notochord) and a peripheral, fibrocartilaginous annulus fibrosus.
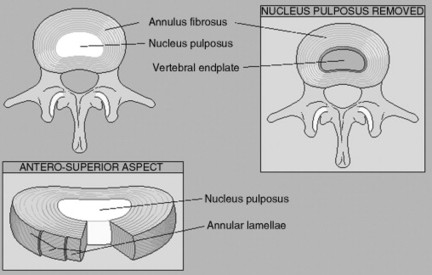 |
| Fig. 4-8 The intervertebral disk. |
The annulus fibrosus is arranged in concentric rings. The collagen fibers in each ring run obliquely from one vertebra to the next, and in each succeeding ring, the fibers run in the opposite direction; that is, one set of fibers runs clockwise, the next counterclockwise, and so forth. This arrangement limits the amount of torsion allowed on the disk and the amount of rotation of the vertebrae relative to one another. In addition, the fibers are under tension, creating a preloading effect, which increases the stability of the joint when it is not under stress, and increasing the ability of the disk to adapt to the stress placed on it, similar to the cables in a suspension bridge.
The outer portion of the annulus fibrosus has a blood supply and is innervated by the sinuvertebral nerves, which may be the cause of much idiopathic back pain. The inner portion has neither innervation nor blood supply and is nourished by diffusion, as is the nucleus pulposus.
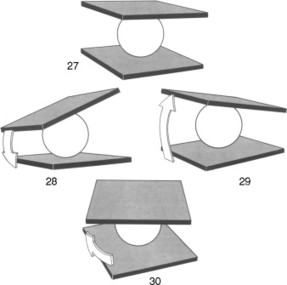
The nucleus pulposus is composed mainly of water, which is bound to a gelatinous matrix by high concentrations of hyaluronic acid. As mentioned, the nucleus is nourished by diffusion, primarily from the periphery of the disk. Dynamic weight bearing has a demonstrable effect on the shape of the disk (Fig. 4-9). During movements of the spine, the nucleus, because of its relative incompressibility, acts as a swivel or pivot around which one vertebra in the FSU can move relative to the other vertebra (Fig. 4-10). Additionally, as the spine moves, the shape of the disk changes because of the elasticity of the annulus fibrosus. This change causes the nucleus to move in various directions, depending on the action of the moment. The pressure of the incompressible nucleus, in turn, causes the annulus to bulge slightly. The bulge is typically held in check by the integrity of its own fibers, as well as by the anterior and posterior longitudinal ligaments. However, under severe loading, these fibers can rupture, creating an injury referred to as a herniated nucleus pulposus (HNP) or “slipped” disk. During the aging process, the water content of the annulus gradually decreases, and collagen cross-linking increases, which causes the annulus to become less elastic and more brittle. Consequently, the probability of incurring an HNP during certain lifting maneuvers is increased yet can be prevented by proper posture during this activity (“Lift with the legs, not the back.”). The arrangement of the anterior and posterior longitudinal ligaments holding the annulus in check predisposes herniation in a posterolateral direction, which unfortunately is in the direction of the intervertebral foramen. Often, nerve impingement and severe pain accompany disk herniation. Occasionally, the nucleus can herniate in a superior or inferior direction, creating a defect in the vertebral bodies, known as Schmorl’s nodes, which can be visualized radiographically.
 |
| Fig. 4-9 Deformation of the intervertebral disk. (From Kapandji IA: Physiology of the joints, New York, 1990, Churchill Livingstone.) Churchill Livingstone |
 |
| Fig. 4-10 Intervertebral disk acting as a swivel in vertebral motion. (From Kapandji IA: Physiology of the joints, New York, 1990, Churchill Livingstone.) Churchill Livingstone |
Other Ligaments
The additional intervertebral ligaments are described as being part of the fibrous intervertebral joints but can also be thought of as check ligaments. These additional ligaments are found between the transverse processes (intertransverse ligaments) and spinous processes (interspinous ligaments). A long, thick ligament is also found extending between and over the tips of the spinous processes, the supraspinous ligament, which extends from the axis to the sacrum. In the cervical region, this ligament forms an attachment point for the ligamentum nuchae. The interspinous and supraspinous ligaments in the cervical region are quite strong and, in deceleration-hyperflexion injuries, can actually avulse the spinous process of the vertebra.
Zygapophyseal Joints
The zygapophyseal joints (also called apophyseal joints or facet joints) occur between the superior and inferior articular processes of the vertebrae. Zygapophyseal joints are synovial joints with a thin, loose, somewhat elastic fibrous capsule and are of the gliding type. The joint facets are covered with hyaline cartilage and are oriented at oblique angles, which are region specific (Fig. 4-11). These joints significantly affect the movements of the vertebrae. Owing to their oblique orientation, motions in the transverse plane (rotation) and frontal plane (lateral flexion or sidebending) are said to be coupled. Although a very small amount of pure rotation or lateral flexion is allowed because of the intervening joint space, the facets engage quickly, and the direction of motion changes to conform to the facet plane. Although the plane of the facets is region specific, a gradual change in orientation takes place so that abrupt changes do not occur (e.g., between the cervical and thoracic regions). However, vertebrae do exist that exhibit characteristics of one region in the superior articular processes and of the caudal region with the inferior articular processes. Such vertebrae are described as transitional (Fig. 4-12).
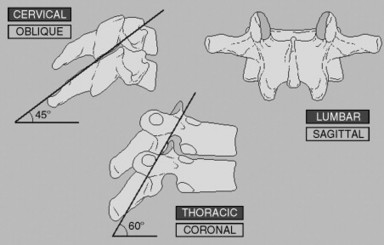 |
| Fig. 4-11 Orientation of the zygapophyseal joints. |
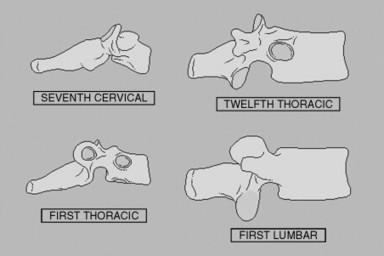 |
| Fig. 4-12 Transitional vertebrae. |
BLOOD SUPPLY AND INNERVATION OF THE VERTEBRAE AND JOINTS
The blood supply to the spine and related tissues differs from region to region. In the cervical region, the vertebral artery and its branches provide the primary blood supply to the vertebrae. In the thoracic and lumbar regions, typical segmental arteries supply the vertebrae. In the sacral region, the blood supply is derived from the lateral sacral branches of the internal iliac arteries (Fig. 4-13).
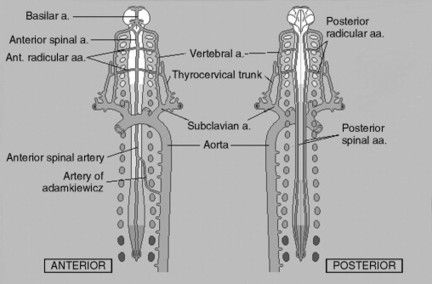 |
| Fig. 4-13 Arterial supply of the axial skeleton. |
Segmental Artery
The typical segmental artery is similar in distribution to that of the spinal nerve (Fig. 4-14). Many of the segmental arteries are branches of the aorta. The descending aorta lies slightly to the left of the midline; therefore the right segmental branch must cross the midline (i.e., the vertebral body) to reach the right side of the body. As the artery crosses the vertebral body, it sends off small branches to supply it, the anterior longitudinal ligament, and the anterolateral portion of the intervertebral disk.
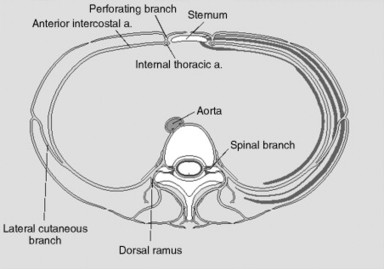 |
| Fig. 4-14 The segmental artery and its main branches. Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




