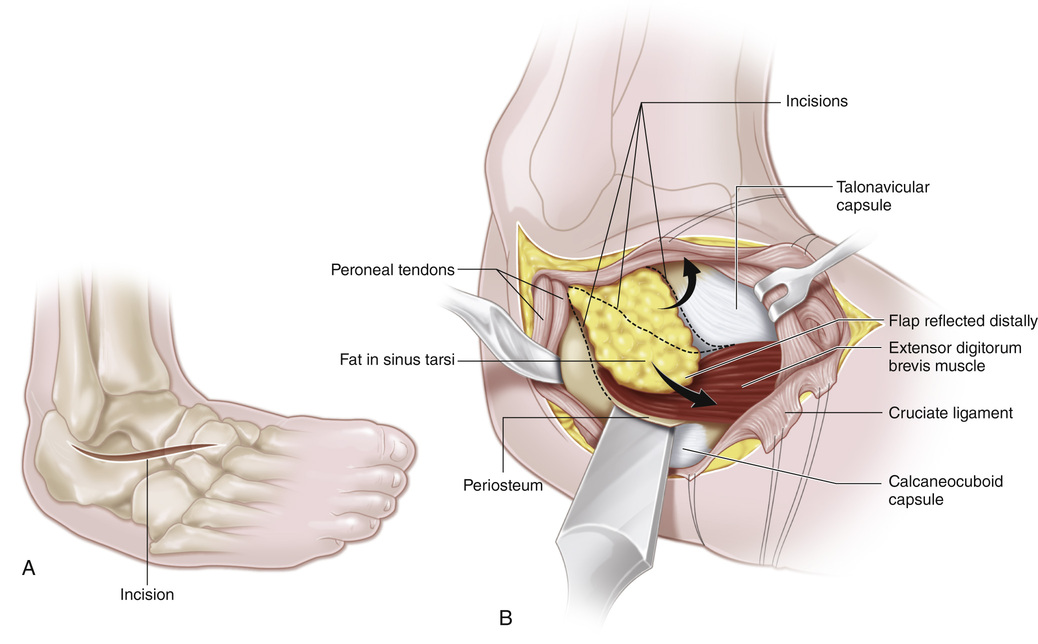
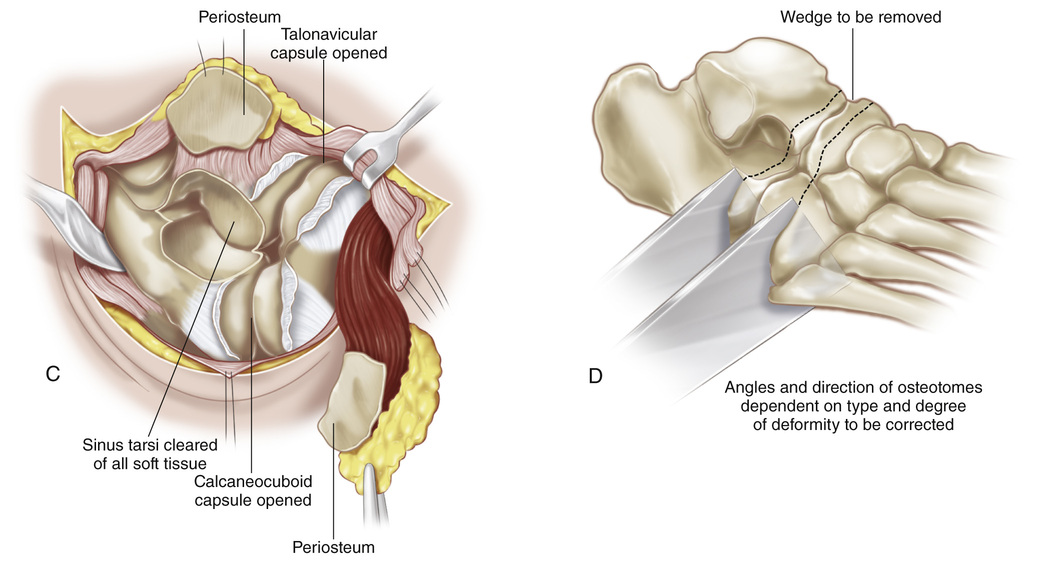
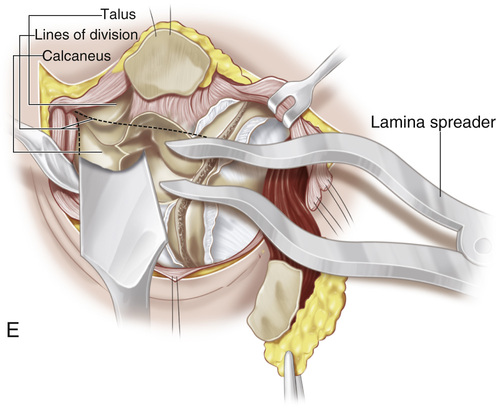
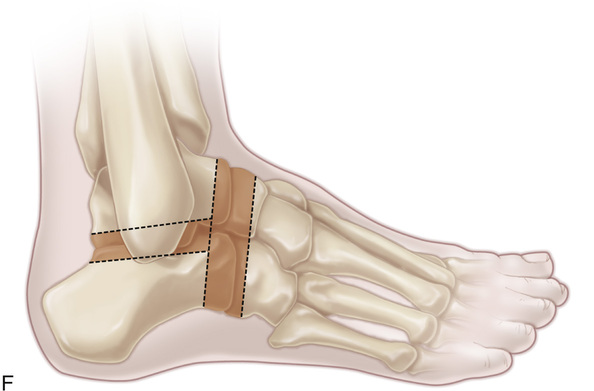
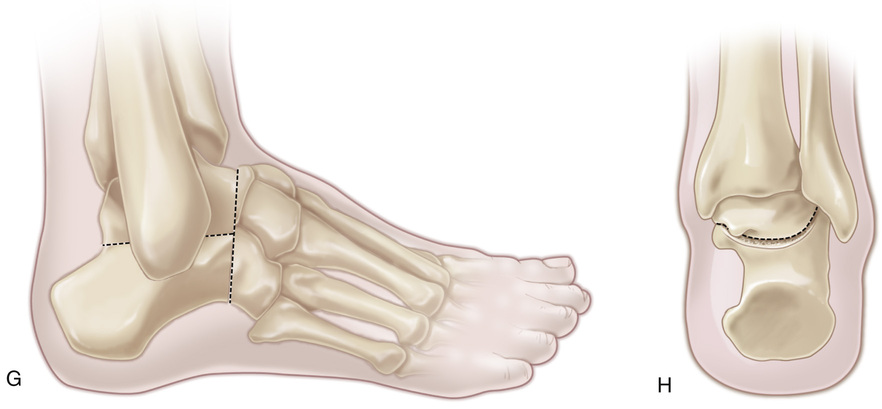
A pneumatic tourniquet is placed on the proximal aspect of the thigh, and the patient is positioned semilaterally with a large sandbag under the hip on the affected side. A, A curvilinear incision centered over the sinus tarsi is made. It starts one fingerbreadth distal and posterior to the tip of the lateral malleolus and extends anteriorly and distally to the base of the second metatarsal bone. B, Skin flaps should not be developed. The incision is carried to the floor of the sinus tarsi. By sharp dissection with scalpel and periosteal elevator, the periosteum of the calcaneus, the adipose tissue contents of the sinus tarsi, and the tendinous origin of the extensor digitorum brevis are elevated in one mass from the calcaneus and lateral aspect of the neck of the talus and retracted distally. It is essential to provide a viable soft tissue pedicle to obliterate the dead space remaining at the end of the operation. Next an incision is made superiorly over the periosteum of the talus, and the head and neck of the talus are carefully exposed. The upper flap of the skin, subcutaneous tissue, and periosteum should be kept as thick as possible to avoid necrosis. Traction sutures are placed on the periosteum. At no time are the skin edges to be retracted. It is not necessary to divide the peroneal tendons or their sheaths. By subperiosteal dissection, the peroneal tendons are retracted posteriorly to expose the subtalar joint. C and D, The capsules of the calcaneocuboid, talonavicular, and subtalar joints are incised. These joints are opened and their cartilaginous surfaces clearly visualized by turning the foot into varus position. A lamina spreader placed in the sinus tarsi will aid in exposure of the posterior subtalar joint. Before excision of the articular cartilaginous surfaces, the surgeon should review the deformity of the foot and decide on the wedges of bone to be removed for correction of the deformity. Circulation of the talus and the complications of avascular necrosis of the talus and arthritis of the ankle after triple arthrodesis should always be kept in mind. The height of the foot is another consideration. A low lateral malleolus causes difficulty wearing shoes. At times, it is best to add a bone graft rather than resect wedges of bone. With a sharp osteotome, the cartilaginous surfaces of the calcaneocuboid joint are excised. Next the articular cartilage surface of the talonavicular joint is exposed, the plane of osteotomy being perpendicular to the long axis of the neck of the talus and parallel to the calcaneocuboid joint. When the beak of the navicular is unduly prominent medially or when, in a varus foot, one cannot obtain adequate exposure of the talonavicular joint without excessive retraction, a second dorsomedial incision may be used to expose the talonavicular joint. E to H, With a lamina spreader in the sinus tarsi, the subtalar joint is widely exposed and the cartilage of the anterior and posterior joints is excised. The surgeon should keep in mind the neurovascular structures behind the medial malleolus. The wedges of bone that must be removed to correct the deformity are excised in one mass with the articular cartilage. It is of great help to leave the osteotome used on the opposing articular surface in place and held steady by the assistant as a second osteotome or gouge is used to take contiguous cartilage and bone. The divided articular surfaces of the joints to undergo arthrodesis are fish-scaled for maximum raw cancellous bony contact. The skin is closed with interrupted sutures. A well-molded long-leg cast is applied with the foot held in the desired position. We have not found fixation of the joints by staples necessary and do not recommend it. In foot stabilization in children with cerebral palsy, especially in the severely athetoid or spastic child, secure crisscross Kirschner wires are used to maintain position. These wires are removed in 6 to 8 weeks.
Triple Arthrodesis
Operative Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








