Pupillary Response
Mainstream research organizations such as the Foundation for Chiropractic Education and Research (FCER) now actively support research on a wide range of somatovisceral disorders, and the definition of chiropractic provided by the Association for Chiropractic Colleges (ACC) 1,2 in 1996 (see Chapter 2 for the full ACC definition) appears to support the contention that somatovisceral considerations are part of mainstream chiropractic. However, a small sector of the profession still wishes to restrict chiropractic to the care of acute, uncomplicated musculoskeletal pain in adults.
Somatovisceral research findings are important, in part, because they represent the scientific study of chiropractic’s role in maintaining wellness. Although wellness and general health can be studied in any patient, whole-person benefits are less obvious when attention is limited to sprain and strain injuries. Research at the somatovisceral interface may provide a window into wellness.
Enhanced understanding of somatic dysfunction and the autonomic effects of the vertebral subluxation complex (VSC) can potentially improve chiropractic assessment methods. To the extent that measurement of autonomic tone becomes a routine step in evaluating VSC, every patient examination can serve as a lesson in the whole-person benefits of chiropractic care. This is no radical departure; the assessment of autonomic tone has a solid pedigree in chiropractic history (Fig. 25-1).
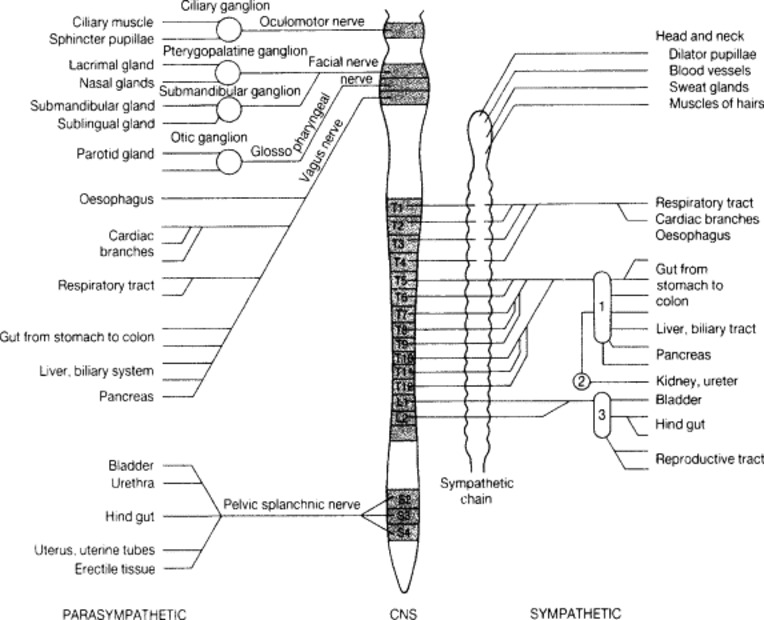 |
| Fig. 25-1 The autonomic nervous system, showing at which levels and within which cranial and spinal nerves that autonomic fibers link with the central nervous system (CNS). 1, Celiac ganglion; 2, renal ganglion; 3, pelvic ganglion. (From Rogers AW: Textbook of anatomy, Edinburgh, 1992, Churchill-Livingstone.) Churchill-Livingstone |
HISTORICAL PERSPECTIVES
An early method of chiropractic analysis was nerve tracing—the use of digital pressure to follow a line of hypersensitive tissue from an uncomfortable body part to the spine or vice versa. A nerve trace to a particular spinal segment was held to represent disturbed tone in the indicated spinal nerve. The chiropractor would suspect disturbed neurologic tone as a cause of dysfunction in all tissues (somatic or visceral) innervated by the indicated nerve.
D.D. Palmer’s foundational concept of tone was understood to apply to any part of the body or the body as a whole3:
Life is the expression of tone. In that sentence is the basic principle of chiropractic. Tone is the normal degree of nerve tension. Tone is expressed in functions by normal elasticity, activity, strength, and excitability of the various organs, as observed in a state of health. Consequently, the cause of disease is any variation in tone.
In modern terms, tone would be defined as the rate or intensity of function of any tissue or organ, reflecting the neurologic integrity of that tissue or organ. Although the whole-body aspect of tone bears much resemblance to the contemporary concept of homeostasis, the segmental aspect of tone was the center of the nerve tracer’s concern.
B.J. Palmer published photographs of many such nerve traces in a book written in 1911. 4 As the reproductions in Figs. 25-2 and 25-3 make clear, originating a nerve trace from an inguinal hernia or a deaf ear was held to be as legitimate as tracing from a sore shoulder or painful hip.
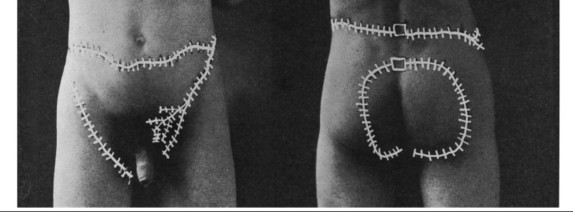 |
| Fig. 25-2 Nerve trace of a patient with a history of inguinal hernia. The results of the nerve trace indicated an apparent relationship between the inguinal and scrotal areas and a lumbar and lumbosacral subluxation. (Courtesy Palmer College of Chiropractic. From Palmer BJ: The philosophy, science and art of nerve tracing, Davenport, Iowa, 1911, Palmer School of Chiropractic.) |
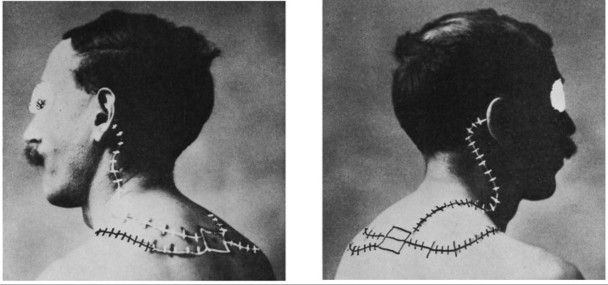 |
| Fig. 25-3 Nerve trace of a patient with a history of deafness in both ears. The results of the nerve trace indicated an apparent relationship between the dysfunctional ears and a subluxation at T2-3. (Courtesy Palmer College of Chiropractic. From Palmer BJ: The philosophy, science and art of nerve tracing, Davenport, Iowa, 1911, Palmer School of Chiropractic.) |
Nerve-tracing data, correlated with autonomic neuroanatomy, was systematized into the meric system of chiropractic analysis. This development was already under way when Mabel Palmer (the wife of B.J. Palmer) published Chiropractic Anatomy in 1918 and had reached maturity by the time R.W. Stephenson published his Chiropractic Textbook in 1927. In meric analysis, a clinical problem is considered in terms of the zone (the body section innervated by a particular pair of spinal nerves) in which it occurs. All tissue of a particular type within a zone is termed a mere. For example, a zone’s muscle tissue is its myomere; its visceral tissue is its viscemere. This concept bears some resemblance to the contemporary concepts of the dermatome (i.e., the skin innervated by the sensory division of a particular spinal nerve) and the myotome (i.e., the muscles innervated by the motor division of a particular spinal nerve).
When a patient complained of stomach discomfort, the meric chiropractor would recognize the involved organ as part of the viscemere corresponding to the fifth through eighth thoracic vertebrae. The results of nerve tracing and the palpation of paraspinal taut and tender fibers would indicate the precise subluxated segment. If these results were ambiguous, a radiographic examination would clarify the analysis. 5
By the early 1920s many chiropractors used the back of the hand to palpate for hot boxes (i.e., areas of increased temperature along the spine). Fascinated by this analytic method, Dossa D. Evins, a 1922 graduate of the Palmer School of Chiropractic, developed the neurocalometer, the first chiropractic heat-reading instrument. It consisted of two thermocouple probes and a galvanometer, which indicated left-to-right thermal asymmetry while the examiner glided the instrument up or down the spine. Persistent thermal asymmetry was taken to be a sign of disturbed vasomotor tone, consistent with the presence of VSC. 6
To summarize, in chiropractic’s early years, assessment of autonomic tone was an integral part of chiropractic analysis. This took the form of nerve tracing, meric analysis, and vasomotor analysis by instrument or by hand. The goal of this autonomic assessment was not to determine whether a patient could be cured of hypertension, asthma, constipation, or other visceral disorders. Rather, it was an essential part of characterizing a patient’s state of disturbed tone (or dis-ease).
It was proposed that VSC could disturb the tone of any neurologically controlled function. Given this assumption, chiropractic analysis logically was not limited to muscular tone, but included vasomotor tone, bronchial tone, alimentary tone, and so forth. Contemporary somatovisceral research is best understood in the spirit of this traditional perspective. It is hoped that this research will encourage the modern evolution of D.D. Palmer’s science of tone.
GASTROINTESTINAL TRACT
Clinical Research: Historical Perspectives
An early osteopathic research team, under the leadership of Louisa Burns, studied the effects of experimental spinal lesions on animals from 1907 to approximately 1948. 7 Hyperemia, hyperchlorhydria, petechial hemorrhages, and ulcers were found in the gastric mucosa of rabbits lesioned at T4-T7.
Medical researcher Henry K. Winsor8 studied correlations between spinal curvatures and internal organ pathology observed during 50 autopsies at the University of Pennsylvania in 1922. Stomach pathology was identified in nine cadavers, liver disease was found in thirteen, gallbladder pathology was described in five, and pancreatic disorders were observed in five. In 28 of these 32 instances of alimentary pathology, curvature was noted in the T5-T9 area.
Chiropractic practitioner and educator Clarence Gonstead recorded a number of clinical insights relevant to the alimentary tract during his long career. 9 Gonstead found peptic ulcers and diarrhea to be most frequently related to upper cervical subluxation, and duodenal ulcers more frequently related to the T4-T10 region. Constipation was linked to multiple sites of subluxation, including T3-T5, T8-T12, L1-L4, and occasionally the upper cervical area.
Several osteopathic investigators have maintained that the upper cervical region and the area from T4-T10 were most often implicated in gastric, duodenal, and peptic ulcers. 10,11 Magoun, 12 an exponent of osteopathic cranial manipulation, has emphasized the importance of lesions affecting the jugular foramen (and therefore the vagus nerve) in the development of various kinds of ulcers and other gastrointestinal disease. An osteopathic study by Northup13 and a study by Lindberg, Strachan, and Koehnlein14 noted the association of the thoracolumbar area and colitis.
Controlled Experimental and Clinical Studies
Pikalov and Kharin15 studied 11 adult patients with endoscopically demonstrated duodenal ulcer who received spinal manipulation supplemented with regional mobilization and manual soft tissue therapy. This group was compared with 24 ulcer patients receiving medication. Both groups were placed on a bland diet. Weekly physical and endoscopic examinations were the major outcome measures. Ulcer remission in the experimental group took place an average of 10 days earlier than in the control group. The most frequently manipulated segments were in the T9-T12 region.
The association of infantile colic and the VSC is controversial. To date, the published controlled clinical trials in this area have failed to settle the issue. A chiropractic team at the University of Odense in Denmark randomly assigned 50 colicky infants to chiropractic care or medication with the drug dimethicone. 16 Dimethicone, which decreases foam in the gastrointestinal tract, is prescribed for colic, although several controlled studies have shown it to be no better than placebo. 17,18 In the chiropractic group, adjustments were administered by light fingertip pressure at segments identified by motion palpation. Most of the adjustments were performed at the upper and middle thoracic regions. By day 12 of the study, the parents of the chiropractic group reported a 67% reduction in hours of crying; there was only a 38% reduction in the medication group. These results were statistically significant. The researchers concluded that, “either spinal manipulation is effective in the treatment of the visceral disorder infantile colic or infantile colic is, in fact, a musculoskeletal disorder.”16
A contrasting view is provided by a study performed under the auspices of a University Pediatrics Department in Norway. 19 In this study, 86 infants were randomly assigned to chiropractic care or placebo (i.e., being held for 10 minutes by a nurse, rather than being given a 10-minute visit with the chiropractor). In the chiropractic group, adjustments were administered by light fingertip pressure. The methods used to identify involved segments were not described, and no mention was made of which regions were most frequently involved. Both groups experienced substantial decreases in crying—the primary outcome measure. Seventy percent of the chiropractic group improved, compared with 60% of those held by nurses. However, no statistically significant differences were found between the two groups in terms of the number of hours of crying or as measured on a five-point improvement scale (from “getting worse” to “completely well”). The researchers concluded that, “chiropractic spinal manipulation is no more effective than placebo in the treatment of infantile colic.”19
It is worth considering whether or not the descriptive literature, which is reviewed in the following section, indicates the existence of an important subset of colicky infants who do respond to chiropractic adjustments. It is suggested that the reader consider the implications of those cases in which the infant responded after a single adjustment, as well as cases in which previous medical intervention failed to resolve the colic. In addition, the reader should consider those cases in which well-described signs of VSC were reduced at the same time that symptoms of colic were reduced. In the absence of clear, effective medical protocols for infantile colic, and in view of the extreme distress that infants and their families can experience as a result of this disorder, the existence of a subset of VSC-related colic could justify a trial of chiropractic care for such infants.
Descriptive Research
A number of well-described cases and case series involving chiropractic care for colicky infants have been published. The most impressive case series to date was published by Klougart, Nilsson, and Jacobsen, 20 in which 38% of Denmark’s chiropractors participated in a prospective study. According to parental reports, 90% of the infants improved within 2 weeks, with 23% improving after a single adjustment. The most commonly adjusted segments were occiput, C1 and C2.
A number of individual case reports are worthy of mention. Pluhar and Schobert21 reported reduced crying, improved sleep, and increased formula consumption after a single adjustment of a 3-month-old girl with a 4-week history of colic. Previous medical intervention had not been successful. Hyman22 reported alleviation of colicky crying, of back arching, and of flatulence after a single adjustment (at T9 and C1) of a 5-week-old boy with a 3-week history of colic.
In a case based on clinical records from the late 1940s and recently recovered from the files of the B.J. Palmer Research Clinic, Killinger and Azad23 reported favorable results with a 5.5-month-old colicky infant after two modified Palmer upper cervical adjustments delivered over a period of 1 week.
Fallon and Lok24 presented a case suggesting a possible cause for some cases of infantile colic. Their patient was a 3-week-old girl with a 2-day history of projectile vomiting, accompanied by colicky crying (up to 18 hours each day). Based on a previous medical diagnosis of pyloric stenosis, surgery had been recommended. The parents opted for a chiropractic consultation before surgery. Palpation of the right upper abdominal quadrant revealed a hard olive-shaped mass, consistent with hypertrophy of the pyloric muscles, thereby supporting the previous diagnosis of pyloric stenosis. A temperature asymmetry of 3° F was noted at the styloid fossae, and attempts to motion palpate the upper cervical spine produced a loud wail from the patient. Light-force upper cervical adjusting was the only intervention, with the exception of a T4 adjustment on one visit. The mother noted cessation of projectile vomiting and reduction in screaming at the fourth visit (eighth day of care); the temperature asymmetry was reduced to 2° F. By the tenth visit, screaming had ceased. The authors suggested that undiagnosed pyloric stenosis may be the cause of some cases of infantile colic.
A number of other descriptive studies in the gastrointestinal arena deserve mention. DeBoer, Schutz, and McKnight25 demonstrated inhibition of stomach and duodenal smooth muscle in rabbits as a result of surgical misalignment of T6. Hewitt26 described the case of a 7-month-old with chronic constipation. According to the patient’s mother, the child had suffered from constipation since birth. At the initial examination, the mother reported that the child’s bowel movements occurred between one time per day and one time every 3 days. Hours of straining and crying preceded each bowel movement, and the consistency of the feces was described as similar to rabbit pellets. After chiropractic examination, gentle diversified adjusting was administered to L5-S1, L4-L5, T6-T7, to the atlantooccipital motion segments, and to the coronal suture. Four such adjustments were performed over a period of 8 weeks. During this time, the child had one to two soft, effortless stools per day, with the exception of 1 week of diarrhea secondary to chicken pox. At the time of publication, this improvement was stable at 1-year follow-up. In addition to the Hewitt study, cases involving constipation and other bowel disorders are described in the section on pelvic organic dysfunction.
Implications for Clinical Assessment
Much chiropractic clinical experience relevant to the gastrointestinal tract has been with pediatric patients. Nyiendo and Olsen27 found that gastrointestinal problems were common primary complaints among pediatric patients attending a chiropractic teaching clinic. These investigators also found that pediatric patients were more likely than adult patients to have nonmusculoskeletal primary complaints. The widespread nerve supply to the gastrointestinal tract makes symptoms of distress in this system good general indicators of autonomic tone.
RESPIRATORY FUNCTION
Clinical Research: Historical Perspectives
Respiratory disorders attracted early and significant attention within the chiropractic and osteopathic research communities. As early as the 1920s, patients with asthma were routinely managed at the B.J. Palmer Clinic.
Of historic and scientific interest is a paper presented by Miller28 at a 1975 Interdisciplinary Conference on Spinal Manipulation at the National Institutes of Health (NIH). In this study, 44 chronic obstructive pulmonary disease (COPD) patients underwent osteopathic examination. COPD is characterized by clinically significant, generalized obstruction of the airways associated with varying degrees of chronic bronchitis, loss of elastic fibers in the lung tissue, and rupture of the alveolar septa. The pathologic changes associated with COPD are generally considered to be irreversible.
Signs of somatic dysfunction noted in Miller’s examination included asymmetry of paraspinal muscle tone, loss of intersegmental mobility, skin drag (i.e., palpatory assessment of asymmetry or local alteration in friction offered to the examiner’s finger while it moves along the patient’s paraspinal skin—a sign consistent with altered sweat gland activity caused by changes in autonomic tone), and red reflex (i.e., visual assessment of asymmetry or unusual intensity in reactive skin hyperemia after stroking with the examiner’s fingertip or fingernail—a sign consistent with altered vasomotor activity caused by changes in autonomic tone). Based on this evaluation, the greatest number of abnormal findings was evident in the thoracic spine, particularly at T2-T5.
Miller’s patients were randomly assigned to treatment and control groups. Both groups received standard medical interventions (including bronchodilators, postural drainage, and breathing exercises); the treatment group also received osteopathic manipulation, consisting of two visits per week (duration of care was not mentioned). Lung volumes were measured, and patients filled out a questionnaire on respiratory symptoms.
The lung volume results were inconclusive; both groups improved, with no significant difference between groups. However, more patients in the treatment group reported the ability to walk greater distances; they also reported fewer colds, less coughing, and less dyspnea than before treatment.
A case series by Hviid29 failed to gather enough data to provide calculations of statistical significance. However, the preliminary data indicated that of 17 symptomatic asthma patients, more than 75% reported subjective improvement by the eighth chiropractic visit. More than 35% were symptom free by the eighth visit. Five of these patients demonstrated increased vital capacity (i.e., the amount of air expelled in a complete exhalation).
Controlled Experimental and Clinical Studies
Two controlled clinical studies have been published in this arena, both dealing with asthmatic patients. Nielsen and colleagues30 reported a randomized controlled clinical trial of chiropractic care for adult asthma patients in which no statistically significant differences were found between sham adjustments and actual chiropractic intervention. The sham maneuver consisted of gentle, apparently specific manual pressure, with the patient positioned on a drop table. While this light pressure was applied with one hand, the drop mechanism was simultaneously released with the other hand. Because the whole patient sample experienced improvement by the end of the study, both in terms of asthma symptom severity and nonspecific bronchial hyperreactivity (i.e., a measure of resistance to histamine-induced bronchial obstruction), it is also possible that both the sham adjustments and the actual adjustments may have elicited healing effects.
An important and controversial study was published in 1998 by Balon and colleagues. 31 After a 3-week baseline evaluation period, 91 children who had continuing symptoms of asthma despite usual medical therapy were randomly assigned to receive either actual or sham chiropractic adjustments for 4 months. Morning peak expiratory flow (i.e., the maximum velocity of air during a forced exhalation) was the major outcome measure. Although both groups of children exhibited improved peak expiratory flow, no significant difference existed between groups. Both groups also demonstrated improvement in terms of secondary outcome measures such as quality of life, daytime symptoms, nighttime symptoms, and inhaler use. However no significant difference between groups was noted in terms of these secondary outcome measures.
The authors offer three possible explanations for the results of this study:
1. Patients in both groups may have responded favorably to frequent professional attention.
2. Patients in both groups may have been growing out of their symptoms at the time of the study.
Another possible explanation is that the sham treatment was not as biologically inert as a placebo should be. Simulated adjustive treatment included several distraction and low-amplitude, low-velocity impulse maneuvers to the cervical, thoracic, and lumbopelvic areas. As in the previously cited paper by Nielsen and colleagues, 30 Balon and colleagues31 assumed that these simulated adjustments would not effect any correction of subluxation or elicit beneficial effects through other means. However, this assumption is questionable. The contemporary chiropractic perspective would anticipate that taking the spine through those movements could, in fact, affect the biomechanical integrity of spinal motion segments, influencing mechanoreceptor and nociceptor pathways. Such concerns are shared by Hondras, Linde, and Jones, 32 who noted in their Cochrane Collaboration review that sham-controlled trials may underestimate the actual benefit of manual therapy. Additional criticism of the sham procedure in the Balon study was offered by Jongeward33 and Richards, Mein, and Nelson. 34
Additional questions concerning the paper by Balon and colleagues was discussed by Rosner, 35 who noted that in a poster presentation at the May 1997 conference of the American Thoracic Society (17 months before publication in the New England Journal of Medicine), Balon and colleagues stated that the patients receiving real chiropractic adjustments improved in terms of nighttime symptoms to a significantly greater degree than those patients receiving the sham procedure. This important and encouraging result was not published in the New England Journal of Medicine paper authored by the same team. This discrepancy remains unexplained as of September, 2002.
Descriptive Research
The case of a COPD patient under chiropractic care was reported by Masarsky and Weber. 36 After a 2-week baseline period, diversified chiropractic adjustments were administered at various levels, usually including the upper cervical and upper thoracic regions. The frequency of visits was three times weekly for more than 14 months. Intersegmental traction, vitamin-C supplementation, cranial adjustments, and soft tissue procedures were also included in the chiropractic regimen. Outcome measures included forced vital capacity (FVC), a measure of the volume of air expelled in a single forceful exhalation; forced expiratory volume in 1 second (FEV1), a measure of the volume of air expelled in the first second of a forceful exhalation; patient ratings on a 10-point severity scale (with 1 mildest and 10 most extreme) for coughing, dyspnea, and fatigue; and a daily count of laryngospasms. Up to three laryngospasms per week had been the norm for the subject for 17 years.
Mean scores during the last 7 months of this study were compared with the mean baseline scores. FVC increased by more than 1.0 L, and FEV1 increased by more than 0.3 L. Coughing intensity, dyspnea, and fatigue all decreased sharply. The patient reported no laryngospasms during the final 5 months of the study. Improved lung volumes lagged behind the subjective improvements by several months. These functional improvements are very encouraging, given that the pathologic changes of COPD are generally considered irreversible.
Peet, Marko, and Piekarczyk37 reported similarly encouraging results with a group of 8 pediatric patients with medically diagnosed asthma. After 10 adjustments according to Chiropractic Biophysics Technique (CBP) protocols, this patient group demonstrated an average increase in peak flow of 25%. The parents of seven of the eight children also reported a decrease in medication use.
Another instructive case involving pediatric asthma was presented by Bachman and Lantz. 38 After three Gonstead adjustments at T3, T12, and the sacrum, the 34-month-old patient experienced 8 weeks of freedom from symptoms. During the previous year, the patient had weekly asthma attacks, twenty of which were severe enough to require visits to the hospital emergency department. An exacerbation at 8 weeks followed a fall from a stepladder; this time the asthma symptoms were accompanied by nocturnal enuresis. Both sets of symptoms resolved after three more adjustments at the same levels. After a full year of freedom from symptoms, the boy fell from a horse and experienced a return of both asthma and enuresis. A single adjustment resolved this exacerbation. The researchers reported no recurrence after 2 years of follow-up evaluation. Peet39 presented the case of an 8-year-old girl medically diagnosed with asthma 3 years before initiation of chiropractic care. Interestingly, this patient exhibited no evidence of respiratory disease until suffering a traumatic injury. This injury was severe enough to cause dislocation of the left elbow. Medication delivered by inhaler was used by this patient one to three times per day before the first chiropractic visit. After eight adjustments according to CBP protocols over a period of 2.5 weeks, the mother stated that the child had not used an inhaler for 2 days, was not wheezing, and could run without gasping. At the time of publication, the patient was reported to have been free of asthmatic attacks for 4 months without medication.
After a retrospective study of the files of 79 patients with medically diagnosed bronchial asthma, Nilsson and Christiansen40 reported that patients likely to have a good response to chiropractic care tend to have less severe asthma symptoms at presentation and an earlier age of onset than do those patients with a poor response.
Masarsky and Weber41 reported on six cases of dyspnea that resolved upon correction of VSC and related somatic dysfunctions. The term somatic dyspnea was coined to refer to such clinical situations. All six patients demonstrated midthoracic fixations on motion palpation, leading clinicians to suspect restriction of rib excursion, disturbance to the sympathetic nerve supply to the lungs and bronchi, or both of these problems. One patient reported a clear-cut association between a C2-C3 correction and relief from dyspnea, suggesting a connection to the phrenic nerve. The most common extravertebral dysfunction associated with somatic dyspnea was at the temporomandibular joint. Somatic dyspnea is a subjective symptom; it is not always accompanied by measurable depression of lung volumes. However, the improved subjective ease of breathing is often rapid and dramatic.
A small but important body of work has demonstrated improved lung volumes in patients without respiratory symptoms and with initial lung volumes within normal limits. Masarsky and Weber42 presented a retrospective study in which FVC and FEV1 improved in a sample of 50 chiropractic patients after one to three diversified adjustments. The majority of these patients had no respiratory complaints at initiation of care and demonstrated FVC and FEV1 within normal limits at intake examination. An additional instance of spirometric improvement in a lung-normal patient appeared in a later case series published by the same authors (case 1). 43
Kessinger reported FVC and FEV1 improvement in a sample of 55 patients after they had received chiropractic care for the correction of upper cervical subluxation. 44 These improvements were significant in the 33 patients with depressed lung volumes at initiation of care and in the 22 patients with initially normal lung volumes.
Implications for Clinical Assessment
Although the lungs are visceral organs, skeletal muscles make inspiration and expiration possible. These include the diaphragm, external and internal intercostals, sternocleidomastoids, levator scapulae, serrati, scalenes, abdominals, trapezii, latissimus dorsi, pectoralis major, and pectoralis minor muscles. In other words, breathing is a musculoskeletal act. More than most bodily functions, breathing straddles the somatovisceral interface. Even if researchers never provided direct evidence that the chiropractic adjustment can improve the lung tissue of pulmonary patients, maintaining the tone of the respiratory muscles of such patients through the chiropractic adjustment would still be a worthy goal.
Although objective measures (e.g., lung volumes) and subjective measures (e.g., respiratory symptom severity) do not directly demonstrate the presence of VSC, such measures do help demonstrate the tone of skeletal and smooth respiratory muscles. As reflections of tone, respiratory observations and measurements can be useful to the chiropractor in assessing clinical outcome.
Taken together, the results on lung-normal patients reported in the two studies by Masarsky and Weber42,43 and the Kessinger44 study imply that even people with normal lung volumes may be functioning well below their potential, and that chiropractic care may improve this already normal physiology. The general health implications of improved pulmonary function cannot be overstated. Lung volumes have long been recognized as a biologic marker of aging. Improvement in these volumes may be seen as tantamount to enhancing vitality and reversing at least one effect of aging.
CARDIOVASCULAR FUNCTION
Clinical Research: Historical Perspectives
Chiropractic’s concern with cardiovascular health goes back to the profession’s earliest days. D.D. Palmer45 described a case of “heart trouble” shortly after the Harvey Lillard case. A later contribution was made by chiropractic clinician, educator, and researcher Carl S. Cleveland Jr. 46 Using surgically implanted spinal splints, Cleveland produced segmental spinal misalignments in the spines of rabbits. Physiologic measures on live rabbits were correlated with postmortem findings. In this innovative first attempt by chiropractic investigators to use an animal model of subluxation, heart diseases, valvular leakages, arrhythmias, and vasomotor paralysis were noted, but the exact spinal levels were apparently not reported. (For further discussion of this study, see Chapter 7.)
Henry K. Winsor, the medical anatomist previously mentioned in the discussion of the gastrointestinal tract, reported autopsy results correlating regions of spinal curvature to 20 cases of heart and pericardium pathology. 8 Spinal curvature was found in the T1-5 region in 18 cases and at C7-T1 in two cases (see Chapter 8).
Osteopathic investigators conducted a great deal of the early research correlating spinal function to cardiovascular health. Louisa Burns’ research team4748 and 49 found experimentally induced lesions from T2 to T4 to be most likely to be followed by cardiac pathology in rabbits. Clinical researchers Becker50 and Koch51 implicated dysfunction of the T1-T6 region in human heart disease.
In a small case series reported by Appleyard, 52 dysfunction in the upper cervical and upper thoracic regions was found to correlate with angina pectoris. Electrocardiographic (ECG) abnormalities noted before osteopathic manipulation were found to have normalized 30 minutes after treatment.
Northup53 reviewed records of 100 hypertensive patients under osteopathic care and reported that dysfunction at T8-T9, the upper cervical area, and the occipitomastoid suture were most frequently found in those patient whose hypertension normalized under osteopathic manipulative therapy. Citing many years of clinical experience, Lewit, 54,55 a Czech medical physician and manual medicine practitioner, maintains that paroxysmal tachycardia with no organic heart lesion routinely responds to osteopathic spinal manipulation.
Controlled Experimental and Clinical Studies
The only recent chiropractic controlled clinical trial in the cardiovascular arena is the hypertension study by Yates and colleagues. 56 Although the number of subjects was small and the physiologic outcome was only measured for the short term (i.e., 1 to 10 minutes postadjustment), this carefully designed study provides a useful model for future work. Twenty-one patients with elevated blood pressure were randomly assigned to active-treatment (adjustments in the T1 to T5 region, based on Activator and protocols), placebo treatment (sham adjustments with the Activator instrument set on zero tension), and control (no intervention) groups. Noting that previous studies may have been confounded by elevated initial readings caused by anxiety (i.e., white coat hypertension), Yates and colleagues used a standard psychologic questionnaire before and after the intervention. They found a statistically significant decrease in both systolic and diastolic blood pressure in the active treatment group but not in the placebo or control groups. Because the active and control groups did not differ on anxiety reduction, this was ruled out as an explanation for the difference between groups. These findings support the hypothesis that short-term blood pressure reduction in hypertensives is a physiologic effect of the chiropractic adjustment.
Descriptive Research
A number of well-described cases involving patients with hypertension have been published in the recent chiropractic literature. Plaugher and Bachman57 published an instructive case study involving a 38-year-old man with a 14-year history of hypertension. The patient also reported side effects caused by his two medications, including bloating sensations, depression, fatigue, and impotence. Low back pain was also reported as an incidental issue.
Examination according to Gonstead protocols revealed evidence of VSC at various levels, particularly in the midcervical, upper thoracic, and middle thoracic regions. Adjustments were administered once per week. After three visits, the patient’s medical doctor was able to reduce the dose of one medication and stop administration of the other one. All medication was discontinued after seven visits. After this, the frequency of visits was reduced to twice per month. Follow-up at 18 months showed that blood pressure was stabilized within normal limits without medication. Bloating, depression, fatigue, and low back pain abated; normal sexual function returned.
Connelly and Rasmussen58 reported favorable results with three hypertensive patients using the cranial procedures of DeJarnette’s sacrooccipital technique (SOT). Particular attention was given to dysfunction of the occipitomastoid suture in these cases. DeJarnette theorized that opening the occipitomastoid suture decompresses the jugular foramen, resulting in a reduced interference to the vagus nerve and subsequent normalization of blood pressure. SOT and osteopathic cranial theory are in apparent agreement in this regard; Northup59 also emphasized the importance of the occipitomastoid suture.
A number of interesting studies involve ECG studies of subjects under chiropractic care. Lott and colleagues60 reported ECG improvements in three of four patients after chiropractic adjustments in conjunction with diet and exercise advice. All four patients experienced improvement in blood pressure, heart rate, or both.
Implications for Clinical Assessment
From the perspective of chiropractic analysis, a history of cardiovascular disease does not isolate an area of subluxation with any certainty. However, increased suspicion is warranted regarding subluxation at the upper thoracic and upper cervical regions of the spine and the occipitomastoid suture of the cranium.
Plaugher and Bachman57 note that the combined effects of antihypertensive medication and chiropractic adjustments can temporarily drive a patient’s blood pressure below normal levels. A patient experiencing vertigo secondary to hypotension after a chiropractic adjustment may be concerned about the possibility of a stroke or some other form of damage. Explaining the possibility of transient hypotension to such a patient at the beginning of treatment is advisable.
PELVIC ORGANIC DYSFUNCTION
Clinical Research: Historical Perspectives
Current understanding of the influence of spinal dysfunction on the pelvic organs (i.e., urogenital tract, lower intestinal tract) owes much to early osteopathic and chiropractic investigators. Clarence Gonstead found that diarrhea was most frequently related to upper cervical subluxation. 9 Gonstead implicated multiple sites of subluxation in association with constipation, including T3-5, T8-12, L1-4, and occasionally the upper cervical area.
Osteopathic investigator Northup13 emphasized the importance of lesions at the thoracolumbar junction in patients with mucous colitis. Lindberg, Strachan, and Koehnlein14 demonstrated a correlation between spinal lesions from T6-L1 and colitis, based on analysis of 349 cases at the Chicago Osteopathic Hospital.
Controlled Experimental and Clinical Studies
To date, dysmenorrhea and pediatric nocturnal enuresis are the only pelvic organic dysfunctions subjected to controlled study in the chiropractic scientific community. In a 1979 study, Thomason and colleagues61 looked at the responses of eleven women suffering from menstrual pain and dysfunction. Among women given lumbar side-posture adjustments, 88% demonstrated significant symptomatic improvement (as assessed by a menstrual symptom questionnaire), whereas none of the women in a control group or in a sham adjustment group reported significant improvement.
In another small trial, Kokjohn and colleagues62 used both symptomatic measurements and serum prostaglandin levels as outcome measures. Citing previous biomedical research implicating elevated serum levels of prostaglandins as an important cause of symptoms of dysmenorrhea, Kokjohn’s team theorized that chiropractic adjustments might reduce these levels. However, there was no statistically significant difference in serum prostaglandin levels between women receiving side-posture adjustments and women in the control or sham adjustment groups. Nevertheless, symptomatic improvement in the experimental group was approximately twice that of the control group, a statistically significant finding that confirmed Thomason’s findings.
Hondras, Long, and Brennan’s follow-up study63 to the earlier study by Kokjohn and colleagues failed to find significant differences in pain (as measured by visual analog scales [VASs]), disability (as measured by questionnaire), or serum prostaglandin levels of dysmenorrhea sufferers receiving side-posture manipulation versus patients receiving a sham procedure. Patients in both the manipulation and sham groups demonstrated mild improvement.
It should be noted that the sham procedure in both the Kokjohn and Hondras studies may not have been as biologically inert as the investigators supposed. It involved a low-amplitude side-posture thrust with both of the patient’s legs flexed, rather than one leg flexed. It was supposed that the flexion of both legs and the reduced amplitude of the thrust would constitute a maneuver that would not correct biomechanical dysfunction. The long history of minimal-force chiropractic adjusting techniques such as Logan basic and SOT pelvic blocking should serve as a caution against such an assumption. The absence of significant differences between the two procedures in the Kokjohn and Hondras studies could reflect that both procedures were corrective at least to the extent of affecting symptom severity, if not prostaglandin levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







