and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
Varus deformity, the most commonly encountered deformity in patients undergoing total knee arthroplasty (TKA), is associated with a limb alignment (hip-knee-ankle angle) of less than 180° and varying degrees of contracture of medial soft-tissue structures, laxity of the lateral soft-tissue structures, flexion deformity and medial bone erosion at the knee joint. Medial osteophytes cause tethering and functional shortening of the medial soft-tissue structures in a varus deformity; posterior osteophytes exert the same effect on the posterior capsule leading to flexion contracture and obstruction to deep flexion. There may also be associated lengthening and attenuation of the lateral soft-tissue structures especially in severe varus deformities.
Introduction
Varus deformity, the most commonly encountered deformity in patients undergoing total knee arthroplasty (TKA), is associated with a limb alignment (hip-knee-ankle angle) of less than 180° and varying degrees of contracture of medial soft-tissue structures, laxity of the lateral soft-tissue structures, flexion deformity and medial bone erosion at the knee joint. Medial osteophytes cause tethering and functional shortening of the medial soft-tissue structures in a varus deformity; posterior osteophytes exert the same effect on the posterior capsule leading to flexion contracture and obstruction to deep flexion. There may also be associated lengthening and attenuation of the lateral soft-tissue structures especially in severe varus deformities [1].
Hence, the challenges in performing TKA in a varus arthritic knee include restoration of limb alignment, balancing the medial and lateral soft-tissue tension, equalising flexion and extension gaps and restoring medial bone loss. Severe varus deformities may be associated with malrotation of the distal femur and tibia which makes conventional bony landmarks less reliable to determine rotational alignment of the femoral and tibial components [2–4]. Furthermore, severe varus deformities may also be associated with extra-articular deformities such as excessive coronal bowing of the femoral shaft and proximal tibia vara which makes TKA technically challenging [5]. The current chapter describes the principles of dealing with a varus deformity, both mild to moderate and severe deformities, during TKA.
Pathoanatomy
Stability and function of the knee joint involve a dynamic interplay of various soft-tissue structures around the knee joint. A sound knowledge of these structures, both under normal and diseased conditions, is crucial to achieve optimum alignment, balance and kinematics after TKA for the arthritic knee. The issue of stability and balancing of soft tissues around the knee joint during TKA is compounded by the fact that ligaments and muscles around the knee joint are dynamic structures which behave differently in knee extension and flexion.
A sequential release of soft-tissue structures has been recommended to achieve equal medial and lateral gaps during TKA [1, 6–9]. It is hence important to know the soft-tissue structures around the medial aspect of the knee joint and the effect of release of these structures on gaps and alignment.
Traditionally, medial soft-tissue structures of the knee joint have been described in three layers [10–12]. The first and most superficial layer consists of the deep crural fascia of the knee joint including the retinacula and the pes anserinus (sartorius, gracilis and semitendinosus) attachment on the anteromedial aspect of the proximal tibia distally. The second layer consists of the superficial part of the medial collateral ligament (MCL) which also gives rise to the posterior oblique ligament (POL) posteromedially (Fig. 3.1). The third and the deepest layer consists of the deep part of MCL, the deep capsular layer and the insertion of the semimembranosus tendon at the posteromedial corner of the tibia just below the joint line. We performed a cadaveric study to quantify the effect of sequential posteromedial release on flexion and extension gaps using an image-free computer navigation system [13]. Our study demonstrated that sequential soft-tissue releases led to an incremental and differential effect on flexion and extension gaps [13]. Hence, judicious and titrated use of this posteromedial soft-tissue releases sequence and following an algorithmic approach will help in correcting deformity and restoring limb alignment and balance during TKA. Although several authors have described different sequence of soft-tissue release for varus deformities [1, 6–9], we follow our technique of sequential soft-tissue release as described here for a cruciate-substituting TKA (Fig. 3.2).
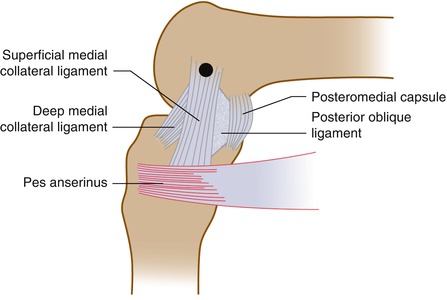
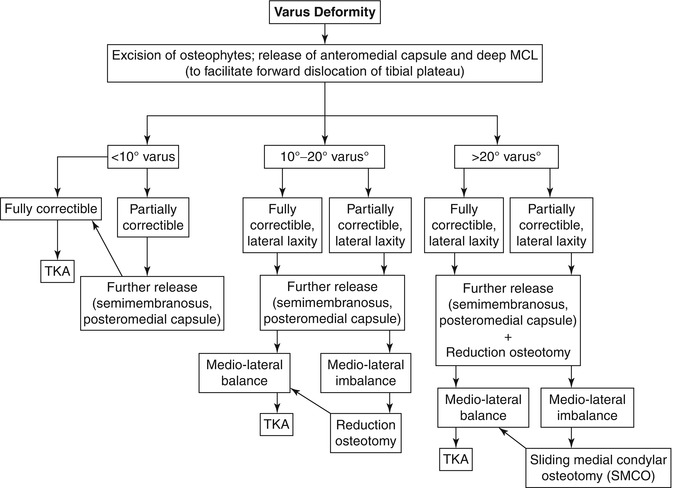
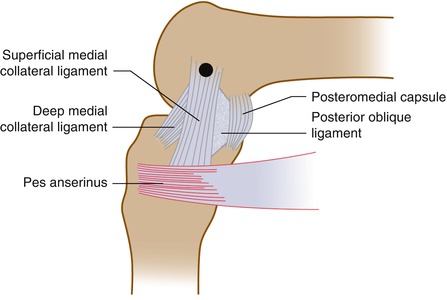
Fig. 3.1
Medial soft-tissue structures of the knee joint
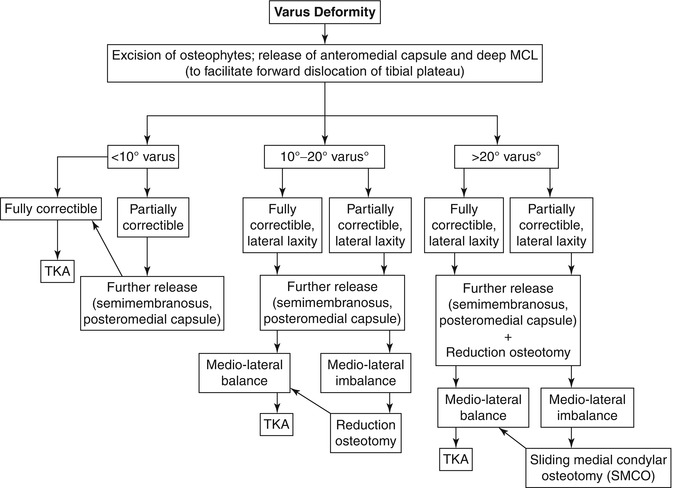
Fig. 3.2
Algorithmic approach to achieve limb alignment and soft-tissue balance in varus deformity during TKA
As described in Chap. 1, a lot of information can be derived about the pathologic soft-tissue and bony changes which have occurred in an arthritic knee based on preoperative radiographic features and examination of the knee under anaesthesia during TKA. Depending on the clinicoradiographic features presented by each varus arthritic knee, the surgeon will have to individualise the amount of bone resection, soft-tissue release and component size and position for each TKA in order to achieve optimum limb alignment and gap balance. Based on our experience of nearly 10,000 TKAs over the last 20 years, the authors have identified several clinical and radiographic features in varus arthritic knees which form the basis of their surgical technique.
The three principal clinical features of varus deformity on clinical examination (under anaesthesia) which need to be noted are (1) correctibility of the deformity (rigid, partially correctible, fully correctible and unstable) with knee in maximum extension, (2) associated sagittal plane deformity (fixed flexion or hyperextension) and (3) extent of lateral side soft-tissue laxity (mild, moderate or severe) (Fig. 3.3). The degree of correctibility of deformity will decide the amount of soft-tissue release required medially in order to achieve correction and balance. Similarly, amount of soft-tissue laxity on the lateral side of the knee in a varus deformity decides the extent of medial soft-tissue release required in order to equalise the medial and lateral soft-tissue gaps. Any associated sagittal plane deformity will require titrating the amount of tibial and distal femoral bony resection and posterior soft-tissue release to achieve deformity correction and flexion-extension gap balance.
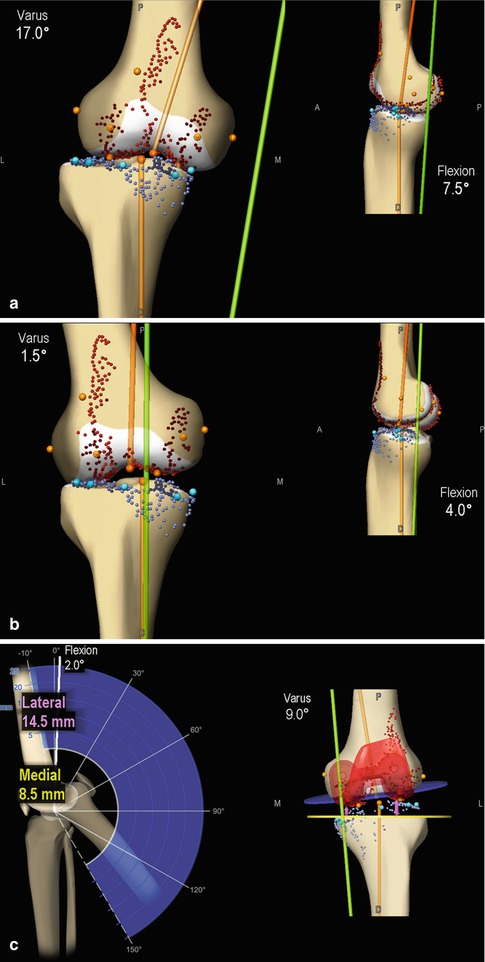
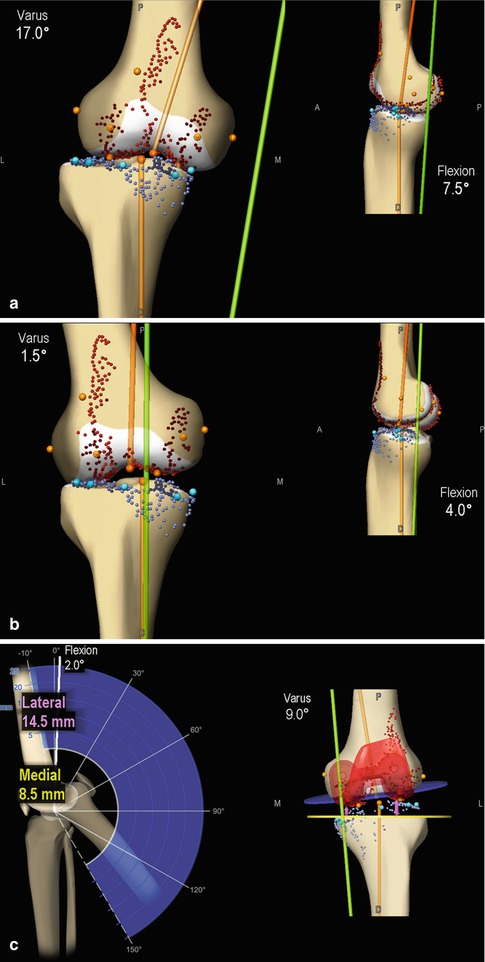
Fig. 3.3
The three principal clinical features of varus arthritic deformity which needs to be noted during TKA (shown here using computer navigation screen shot images). (a) Maximum varus deformity (using a varus stress at the knee joint in maximum extension) and maximum knee deformity in the sagittal plane (flexion). (b) Maximum correctibility of varus deformity (using a valgus stress at the knee joint in maximum extension). (c) Maximum lateral soft-tissue laxity (using a varus stress at the knee joint in maximum extension)
Preoperative radiographic features will usually provide hints as to what manoeuvres need to be carried out to correct the deformity and achieve optimum soft-tissue balance and can also help predict the difficulty a surgeon may face in achieving these goals. The five radiographic features of varus arthritic knees which need attention are (1) degree of deformity (as measured on full-length hip-to-ankle radiographs), (2) amount of lateral laxity (based on joint divergence angle and lateral translation of tibia), (3) presence of extra-articular deformity (coronal femoral bowing based on valgus correction angle, tibia vara based on tibial plateau angle), (4) medial bone loss (mild, moderate, severe) and (5) presence of osteophytes (minimal, moderate, abundant) (Fig. 3.4).
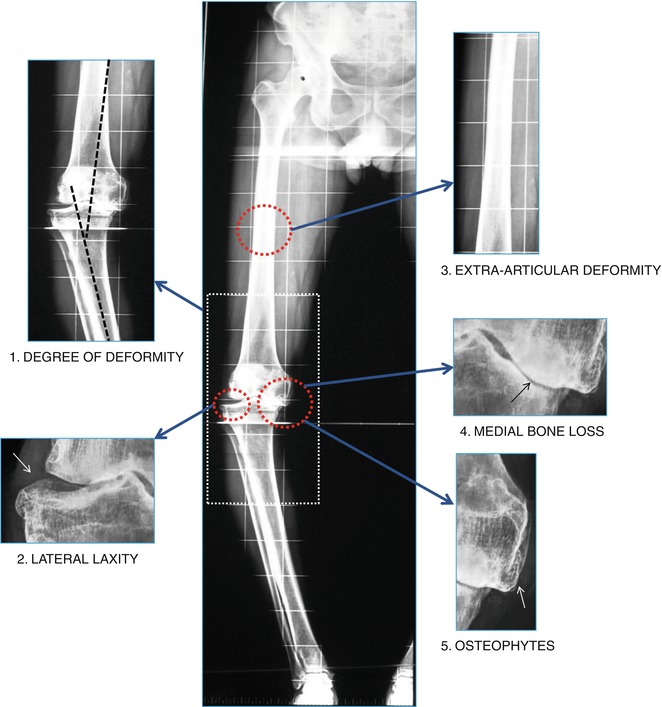
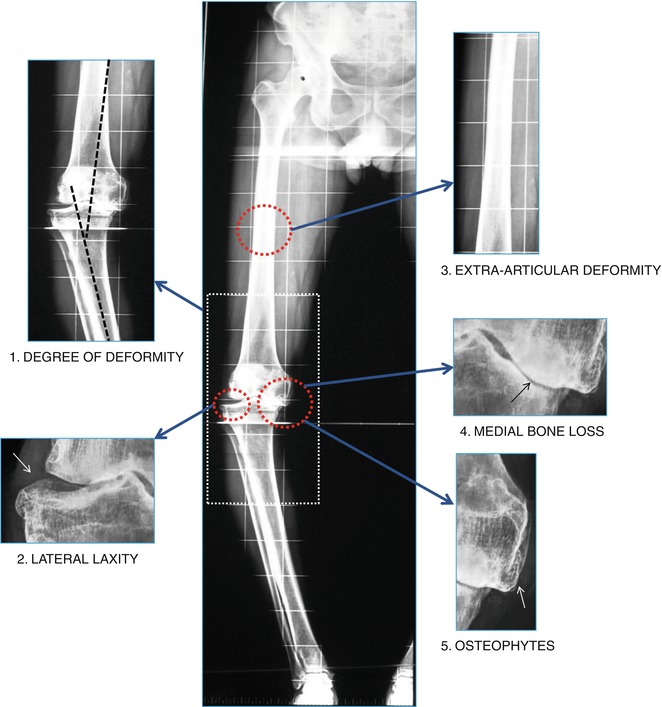
Fig. 3.4
The five principal radiographic features of varus arthritic deformity which needs to be noted on preoperative full-length hip-to-ankle radiographs
Several of the above features may be present or absent primarily based on the severity of arthritic involvement and the degree of knee deformity. Rigidity, associated sagittal plane deformities, excessive lateral laxity, abundant osteophytes and severe medial bone loss are more commonly seen in knees with severe long-standing varus deformities (especially ≥20°) than in knees with mild to moderate varus deformities [4]. In some knees, where the degree of arthritic involvement and the amount of intra-articular deformity is less severe, the above features may be absent. However, in these knees the degree of deformity may be confounded by the presence of an extra-articular deformity (commonly excessive coronal bowing of the femur) which adds to the overall severity of limb deformity and makes the case more challenging to treat (Fig. 3.5). Furthermore, increase in varus deformity may also cause variation in the distal valgus correction angle (VCA) and rotational profile of the distal femur and the tibia which needs to be accounted for while positioning the femoral and tibial components [2–4, 14–19].


Fig. 3.5
Extra-articular deformity confounding the severity of deformity in an arthritic knee. (a) Preoperative standing knee radiograph showing mild changes in terms of deformity, bone loss, osteophytes and lateral laxity. Dotted line shows femorotibial angle. (b) Preoperative standing, full-length hip-to-ankle radiograph of the same patient (a) showing significant coronal bowing of the femoral shaft (arrow) because of which the distal femoral valgus correction angle (VCA) in this patient is almost 10.5°. Dotted line is the anatomic axis of the distal femur and the black line shows the femoral mechanical axis; the angle formed by the two lines is the VCA
Based on radiographic analysis of 1,500 computer-assisted TKAs [5], the authors have described features of an “at–risk” knee which can be identified on preoperative standing, full-length hip-to-ankle radiographs (Fig. 3.6). The presence of these preoperative radiographic features put the knee at greater risk for malalignment after TKA [5]. Hence, the surgeon should identify such “at-risk” knees, and every measure must be undertaken to ensure optimum limb and component alignment and soft-tissue balance during TKA.
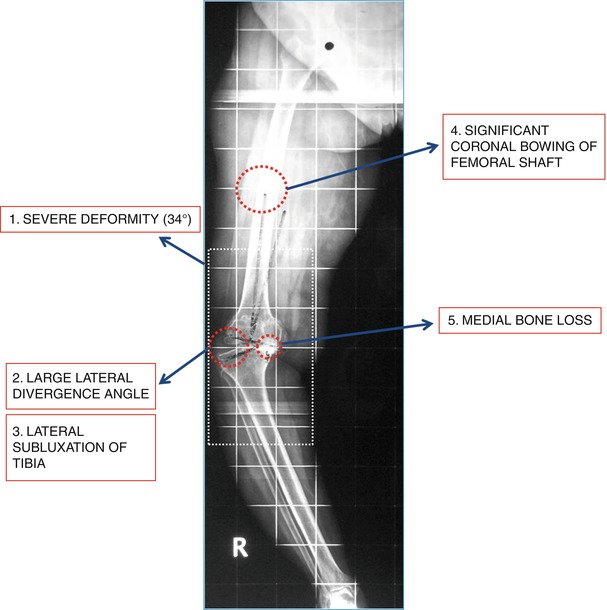
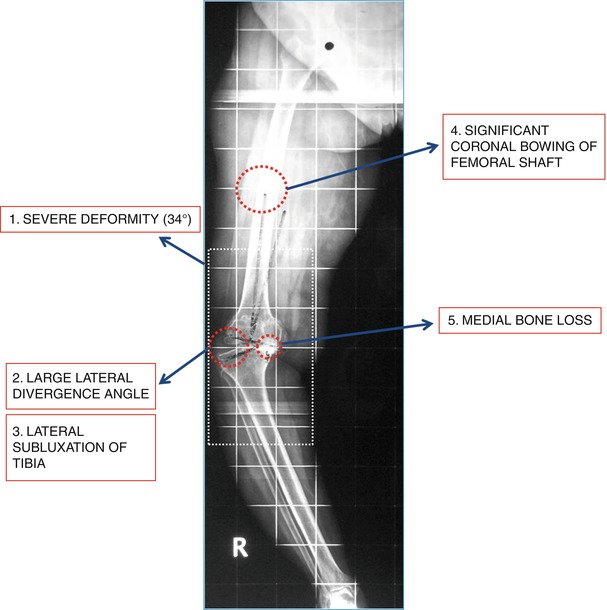
Fig. 3.6
The “at-risk” knee showing five features on preoperative full-length hip-to-ankle radiographs which may increase the risk of malalignment in this patient
Surgical Technique
The surgical technique followed by the authors for varus TKA is based on the presence of any combination of the three clinical and five radiographic features present in the arthritic knee. The basic technique followed is one of gap balancing where bone resection and soft-tissue release are tailored to each individual knee based on the presence or absence of the above clinicoradiologic features. The varus arthritic knee is treated with progressive release of medial soft-tissue structures to achieve full correction of deformity and to achieve “equipoise” with the lateral soft-tissue structures. However, this release of medial soft-tissue structures needs to be controlled and measured to avoid overcorrection or instability.
The first step to achieve these goals is to remove all osteophytes around the knee joint which will not only free the tethered soft-tissue structures but also helps avoid unnecessary soft-tissue release. Following this principal step, the surgeon can accurately assess in full extension how much residual deformity and soft-tissue tightness persists and which may require a formal soft-tissue release. Based on whether the deformity is fully correctible, partially correctible, rigid or unstable, further soft-tissue release may be required in order to correct the deformity. Most partially correctible deformities get fully corrected with removal of osteophytes and the preliminary soft-tissue release (deep MCL and semimembranosus) performed for exposure of the joint and anterior dislocation of tibia. However, the medial release required may be extensive (posteromedial capsular attachment to proximal tibia and segmental excision of the posteromedial capsule) in cases with rigid deformities or knees with severe medio-lateral soft-tissue imbalance and may also require performing a reduction osteotomy of the tibia (see Chap. 11 for technique) with or without undersizing the tibial component [20]. In contrast, soft-tissue releases should be restricted and controlled in knees which are unstable in coronal and or sagittal planes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








