and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
Knees with degenerative or rheumatoid arthritis may have associated intra-articular inflammation and effusion because of which they may assume a position of flexion in response to the pain and increased intra-articular pressure. Posterior femoral and tibial osteophytes along with those in the intercondylar notch in OA may enhance the deformity by tenting the posterior capsule or blocking full extension. This, in the long run, becomes a fixed flexion deformity, adding to the disability of the patient. Knee arthritis with a fixed flexion deformity interferes with ambulation causing increased energy expenditure, decreased stride length and velocity, decreased endurance and inability to stand for long periods. Flexion deformities are commonly encountered in knees with varus or valgus deformities. Isolated flexion deformities in knee arthritis are rare, although in some knees fixed flexion deformity may be the predominant deformity when compared to coronal plane deformities. It is estimated that flexion contractures may occur in up to 60 % of knees undergoing TKA. This chapter aims to discuss the management of fixed flexion deformities in TKA.
Introduction
Knees with degenerative or rheumatoid arthritis may have associated intra-articular inflammation and effusion because of which they may assume a position of flexion in response to the pain and increased intra-articular pressure. Posterior femoral and tibial osteophytes along with those in the intercondylar notch in OA may enhance the deformity by tenting the posterior capsule or blocking full extension. This, in the long run, becomes a fixed flexion deformity, adding to the disability of the patient. Knee arthritis with a fixed flexion deformity interferes with ambulation causing increased energy expenditure, decreased stride length and velocity, decreased endurance and inability to stand for long periods [1–5]. Flexion deformities are commonly encountered in knees with varus or valgus deformities. Isolated flexion deformities in knee arthritis are rare, although in some knees fixed flexion deformity may be the predominant deformity when compared to coronal plane deformities. It is estimated that flexion contractures may occur in up to 60 % of knees undergoing TKA [4]. Griffin et al. [6] reported the incidence of flexion contractures as 62 % in varus knees, 31 % in valgus knees and 26 % in neutral knees. This chapter aims to discuss the management of fixed flexion deformities in TKA.
Pathoanatomy
Flexion deformities in arthritic knees may result from intercondylar notch osteophytes which act as a mechanical block preventing full extension [7], whereas posterior osteophytes cause tenting of the posterior capsule which can enhance this deformity (Fig. 5.1). In long-standing cases, these osteophytes are associated with secondary contracture and shortening of soft-tissue structures such as the posterior capsule, posterior oblique ligament, semimembranosus (in varus knee) and popliteofibular ligament (in valgus knee) which add to the deformity. In severe cases, the hamstrings and gastrocnemius may also be affected. Rarely in patients with inflammatory arthritis, neuromuscular disorders, haemophilia or long-standing immobility, flexion deformity is primarily the result of isolated soft-tissue contractures, and minimal osteophytes may be present (Fig. 5.2).

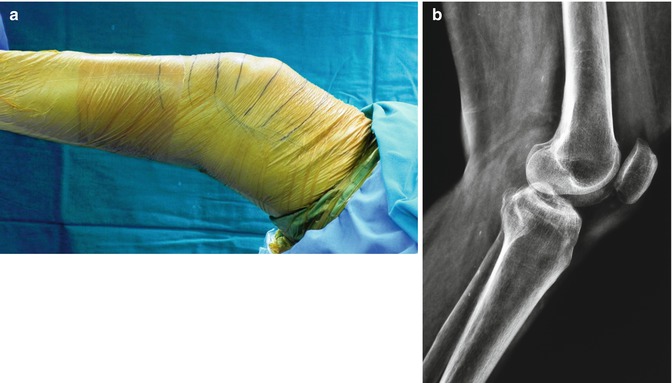

Fig. 5.1
Osteophytes in knees with flexion deformity undergoing TKA. (a) Lateral radiograph of the knee showing anterior tibial or “anvil” osteophyte (white arrow) and posterior tibial and femoral osteophytes (black arrows). Osteophytes at all these three locations can contribute to flexion deformity, anterior tibial osteophyte by mechanically blocking knee extension and posterior osteophytes by tenting soft-tissue structures. (b) Lateral radiograph of the knee showing a large posterior femoral osteophyte (arrow) which should be completely removed to not only achieve correction of flexion deformity but also prevent postoperative restriction of terminal flexion. (c) Lateral radiograph of the knee showing large osteophytes all around the knee joint including large, multiple osteophytes in the patellofemoral joint (arrow)
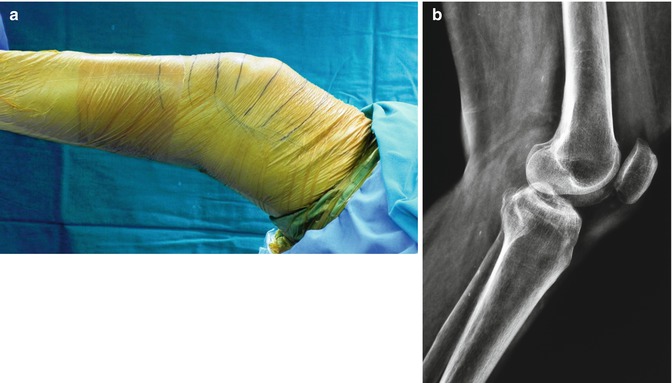
Fig. 5.2
Fixed flexion deformity of the knee due to contracture of soft-tissue structures. (a) Intraoperative clinical photograph of a patient showing fixed flexion deformity of almost 30°. (b) Lateral knee radiograph of the same patient showing absence of osteophytes around the knee joint. The flexion deformity in this patient with rheumatoid arthritis was purely due contracture of soft-tissue structures
Consequences of long-standing flexion deformities in arthritic knees include bone loss on the posterior aspect of the tibial plateau and reduction of quadriceps strength leading to persistent extensor lag postoperatively. The latter is typically masked preoperatively due to the flexion deformity and becomes obvious once the flexion deformity has been fully corrected with TKA. It is necessary to keep this in mind and inform the patient regarding the possible need for extensive postoperative physiotherapy not only to maintain correction of the flexion deformity but also to strengthen the quadriceps. Lombardi et al. [8] have divided flexion deformities encountered in patients undergoing TKA into three grades based on the severity of deformity (Table 5.1). The primary step in correcting flexion deformity is to remove all osteophytes whenever present in order to remove their tenting effect on soft tissues. This usually takes care of most mild to moderate deformities. However, severe deformities may require an additional soft-tissue release posteriorly.
Table 5.1
Classification of flexion contractures
Grade 1: <10° |
Grade 2: 10°–30° |
Grade 3: >30° |
The flexion gap is much larger than the extension gap in an arthritic knee with flexion deformity. This mismatch is further increased when there is an associated severe coronal plane deformity requiring extensive medial or lateral soft-tissue release. This mismatch can be addressed to a certain extent with a posterior soft-tissue release. However, if the extension gap continues to be small, 2 mm of additional bone may need to be resected from the distal femur. Another method is to upsize the femoral component so as to close the flexion gap relative to the extension gap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








