and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
The rotational alignment of femoral and tibial components in TKA is based on various bony landmarks and reference axes around the knee joint. However, most of these landmarks and reference axes have been derived from normal unaffected knees. In knees with arthritis, these landmarks and axes may get distorted due to significant cartilage wear, bone loss, soft-tissue contracture and additional extra-articular bony deformities frequently associated with severe knee deformity.
Introduction
The rotational alignment of femoral and tibial components in TKA is based on various bony landmarks and reference axes around the knee joint. However, most of these landmarks and reference axes have been derived from normal unaffected knees. In knees with arthritis, these landmarks and axes may get distorted due to significant cartilage wear, bone loss, soft-tissue contracture and additional extra-articular bony deformities frequently associated with severe knee deformity [1].
Varus arthritic deformities of the knee are typically associated with increased external rotation of the tibia [2]. Similarly, severe arthritis and deformity are associated with excessive wear of the femoral condyles, and excessive medial or lateral soft-tissue contracture leading to increased internal or external rotation of the distal femur [3]. These pathological changes cause distortion of standard reference axes and landmarks such as the tibial tubercle, posterior condyle angle, epicondylar axis and anteroposterior axis. Hence, if such torsional deformities are not taken into account during TKA, it may result in rotational malalignment of components which will lead to patellar maltracking, abnormal gait, postoperative pain, poor function and early wear [4–8]. This chapter aims to address rotational deformities in arthritic knees undergoing TKA.
Pathoanatomy
The lower extremity from an in utero position of internal rotation slowly undergoes lateral or external rotation throughout the growth phase of the child till skeletal maturity [9]. Staheli and Engel [10] in their study of tibial torsion in children estimated tibial torsion at 15° of external rotation at skeletal maturity. Based on the orientation of the bimalleolar axis with respect to the flexion-extension axis of the knee joint, the tibia shows dynamic internal rotation when the knee is flexed [11, 12]. During gait, the tibia shows dynamic internal rotation with respect to the femur at mid and terminal stance and dynamic external rotation from toe off until slightly before heel strike [12]. In normal subjects, the tibia is typically in external rotation with Caucasian limbs showing greater external rotation compared to Asian limbs [13].
Whether abnormal torsion is a cause or a consequence of knee osteoarthritis is still unclear. Nagamine et al. [14] in their CT scan analysis of normal and osteoarthritic tibiae in Japanese subjects had suggested that the traditional way of sitting on the floor with the foot internally rotated (tatami position) since childhood may cause growth disturbance at the proximal tibial meta physis, causing tibia vara and medial torsion of the tibia. Krackow et al. [15] in a recent study to quantify the association between medial knee loading and tibial torsion reported that subjects with medial OA and associated tibial intorsion walked with significantly greater knee loading compared to controls. Hence, the incidence and pattern of torsional deformity in patients with knee OA shows wide variation depending on the ethnicity of the population and severity of deformity.
Several techniques are used to determine the rotational position of the femoral component during TKA. These include using bony landmarks on the distal femur, soft-tissue tension and flexion gap (gap balancing) and computer navigation [16]. However, no single technique has emerged as a clear winner [17], and most surgeons use a combination of two or more techniques. Distal femoral bony landmarks are most frequently and principally used to determine rotation of the femoral component (Fig. 7.1). However, several reports have underlined the fact that such bony landmarks show wide variation not only among arthritic knees but even among normal subjects [2, 18–22]. Furthermore, use of one specific bony landmark may be unreliable to determine femoral component rotation and may be affected by severity and type of underlying arthritic knee deformity. For example, the anteroposterior axis (Whiteside’s line) may not be reliable in cases with severe patellofemoral arthritis which may cause significant trochlear wear and distortion [23, 24], and the posterior condylar angle (PCA) may not be reliable in knees with severe wear and bone loss of the posterior condyles [25]. Hence, in such cases some other technique must be used to determine femoral rotation. The gap-balancing technique involves rotating the femoral component so as to achieve medio-lateral flexion gap symmetry (with the help of a tensioning device such as laminar spreaders) after having achieved a balanced and symmetric extension gap. However, the femoral rotation required may vary depending on the amount of distal femoral bony loss or distortion and the extent of medio-lateral flexion gap asymmetry. Although computer navigation has proven to improve limb and component alignment during TKA, studies have reported malrotation of the femoral component during CAS TKA when a single anatomic landmark is used as reference [26, 27]. For example, using only the epicondylar axis as reference may lead to excessive external rotation of the femoral component. However, using a combination of anatomic and kinematic data has been reported to improve accuracy of rotational alignment of the femoral component [27].
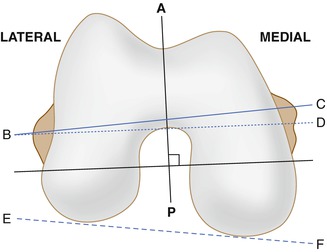
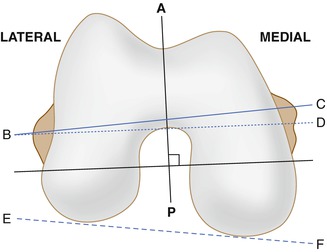
Fig. 7.1
Distal femoral bony landmarks frequently used to determine rotation of the femoral component. Line AP – Anteroposterior axis or the Whiteside’s line drawn along the deepest part of the trochlear sulcus. The femoral component is placed perpendicular to this axis. Line BC – Anatomic transepicondylar axis connecting the lateral epicondyle (point B) and the medial epicondyle (point C). Line BD – Clinical transepicondylar axis connecting the lateral epicondyle (point B) and the medial sulcus (point D). Line EF – Posterior condylar line drawn tangent to the posterior-most point of the medial and lateral posterior femoral condyles
On the tibial side, options to determine tibial component rotation include using bony landmarks and putting the knee through an arc of flexion and extension and positioning the tibial tray vis-à-vis the femoral component (the “self-positioning” method) [16]. Traditionally, the tibial tubercle (junction of the middle and medial one-third) has been used as a fixed bony landmark to determine the rotational alignment of the tibial tray. However, similar to distal femoral bony landmarks, the tibial tubercle may show wide variations among patients depending on the severity of knee deformity and ethnicity [2, 28–30]. Sun et al. [29] in a CT scan-based study of Chinese osteoarthritic knees reported that the tibial component has a tendency to be placed in greater external rotation when the medial one-third of the tibial tuberosity is used as a landmark in arthritic knees with varus or valgus deformities. Hence, they concluded that the tibial tuberosity is an unreliable rotational landmark for tibial tray in Asian patients with deformed, arthritic knees [29]. In a similar study on European subjects, Bonnin et al. [31] reported significant variation in the position of the tibial tuberosity which caused not only excessive external rotation of the tibial component but also deficient coverage of the tibial cut surface by the tibial tray.
Surgical Technique
Femur
The severity and type of knee deformity and the presence of an extra-articular rotational deformity must be taken into account before deciding on the rotational alignment of the femoral component during TKA. Matsui et al. [2] in a CT scan study of 150 arthritic knees and 31 normal controls reported progressive external rotation of the distal femur with increasing severity of varus deformity when compared to rotation in normal controls. However, this difference was significant only when the epicondylar axes (either surgical or clinical) were compared, whereas there was no difference when the posterior condylar axes were compared. Therefore, the distal femoral rotation in an arthritic knee with varus <10° is similar to a normal knee, whereas the distal femur may be in excessive external rotation when the varus deformity is 20° or more. In valgus knees, Matsuda et al. [3] using MRI analysis of the distal femur reported that the posterior condylar line with respect to the transepicondylar axis was in 11.5° internal rotation compared to 6.4° internal rotation in normal knees and 6.1° internal rotation in varus knees. This is probably due to significant distortion and wear of the lateral femoral condyle in valgus knees.
Owing to wide variations in bony landmarks in arthritic knees, the authors use the combined referencing technique to determine femoral component position during TKA. Using a soft-tissue tensioner, the medio-lateral gap is first assessed with the knee in 90° flexion, and the tentative posterior cut is marked (parallel to the cut tibial surface) on the distal femur surface based on soft-tissue tension. We use the AP axis as the preliminary reference to position the AP cutting block equivalent to the femoral component size estimated. In cases where the femoral trochlea shows significant wear, the epicondylar axis is used as the preliminary reference. The surgeon then references the anterior cortex of the distal femur (using a stylus or angel wing) to avoid notching and the previously made mark on the posterior aspect of the distal femoral cut surface based on soft-tissue tension. The AP cutting block should be generally parallel to the epicondylar axis and perpendicular to the AP axis (Whiteside’s line). Appropriate soft-tissue releases are performed if required to achieve medio-lateral gap balance. In valgus knees there may be excessive tightness laterally, and medially in varus knees. This becomes evident if the cutting block position deviates significantly from any of the chosen references. After pinning the AP cutting block to the distal femur, the flexion gap balance is assessed using a spacer block. If the flexion gap seems too tight either medially or laterally, the AP block may be slightly externally or internally rotated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








