A patient has a Grade II traumatic cervical sprain as a result of a rear-end automobile accident. The patient’s chief complaint is severe pain located at the anterior cervical area. How should this case be approached from a manual point of view? A professional piano player reports pain and paresthesia in the first three and one-half fingers of his right hand. Surgery for carpal tunnel syndrome has failed to relieve his symptoms. What manual methods are appropriate in this case? Another patient complains of chronic lumbar pain, and examination reveals a chronically shortened iliopsoas muscle. What is the manual approach for treating the shortened iliopsoas muscle? Still another patient has consulted several orthopedists and chiropractors with chronic midscapular pain. He has a forward head and shoulder posture. Spinal adjustments have relieved the problem but offered no sustained solution. What alternative manual approach could be the primary treatment for this condition?
All these conditions will benefit from spinal adjustments, but in each case, soft tissue therapies can either completely resolve the condition or (in the acute first case) provide symptomatic relief until a spinal adjustment is feasible.
RATIONALE FOR MANUAL SOFT TISSUE PROCEDURES
Differentiating Spinal from Peripheral Causes for Pain
The first responsibility of doctors of chiropractic dealing with the total locomotor system is to find the source of the pain. The location of the source, along with its acuteness or chronicity, generally determines the type of treatment. In evaluating spinal subluxations related to musculoskeletal pain, the following question must always be asked: How much of the pain is directly related to the articular component of the subluxation? In many cases of peripheral soft tissue pain, the primary cause is in fact peripheral, in the local soft tissue itself, not in the spine. Thus although the lumbar spine and sacroiliac joint may be indirectly related to an Achilles tendinosis or a trochanteric bursitis, the majority of the treatment in these cases must be directed to the involved soft tissue.
From a soft tissue point of view, the problem may be located in various areas, including the muscle belly, musculotendinous portion, body of the tendon, insertion point of the tendon, bursa, ligament, or fascia. The soft tissue may be under tension because of a spinal source of pain; a postural, structural, or functional aberration; a viscerosomatic problem; or a problem located at the local soft tissue level. Chiropractors pay particular attention to the vertebral subluxation complex (VSC), with special emphasis on joint kinesiopathology, usually hypomobility. 1 If a primary reason for a subluxation is restriction within paraspinal or outlying muscles (i.e., the myofascial component of VSC) or connective tissue (i.e., the histopathologic component of VSC) because of microtraumatic or macrotraumatic injury, sedentary living, or altered motor patterns that have created muscular imbalances, then spinal adjustments alone may not fully address the condition.
In addition to influencing vertebral joint mechanics, spinal adjustments also directly affect soft tissues. Facet movement externally elicited by an adjustment affects the joint capsules and surrounding periarticular connective tissue including muscles, ligaments, and fascia. A joint is a space built for motion, and connective tissue structures surrounding that space are soft tissues affected by movement. The human spine, which is composed of vertebral bodies, disks, and supporting ligaments, lacks the ability to move on its own; it depends on the dynamic muscular system as its prime mover. Although spinal adjustments affect surrounding muscles, ligaments, and fascia, treatment of these soft tissue structures similarly affects spinal joint mechanics. It is important that chiropractors not limit their focus to only one side of this equation.
Evaluating and Treating the Whole System
Those seeking to develop expertise in treating functional conditions of the musculoskeletal system must evaluate and treat the whole system. The brain is a sensory and motor organ that delivers orders based on the sensory information it receives. Any persistent or chronic peripheral dysfunction (i.e., shortened muscle or fascia, trigger points, hyperpronation) will elicit a compensatory response from the central nervous system, which may result in an altered movement pattern. A typical example of such alteration is abnormal hip extension caused by a weak gluteus maximus. The weakened gluteus maximus could be caused by its antagonist, a shortened iliopsoas, based on Sherrington’s law of reciprocal innervation (contraction of muscles is accompanied by the simultaneous inhibition of their antagonists), or a sacroiliac fixation could have caused the weakened muscle. Abnormal hip extension could create a change in gait (weakened hip extension), resulting in compensatory lumbar lordosis and hypermobility at the L4 and L5 vertebral segments.
Many altered patterns of movement remain in place even after the original painful lesion has disappeared2,3 and are significant factors in subluxations that fail to respond to chiropractic adjustments or refixate after adjustment. Treatment of peripheral lesions not related to the spine, as well as treatment and prevention of spinal joint dysfunctions (subluxations), require evaluation and treatment of extraarticular soft tissue.
Distinguishing the Results from the Rationale
Clinicians using soft tissue methods usually report results through case studies because controlled studies are often difficult and sometimes impossible to perform. The rationales that clinicians use to explain their results are not necessarily valid, and researchers will eventually prove or disprove these theoretical explanations. For example, in 1984, Cyriax4 described the effects of his method of frictional massage as increasing circulation and breaking down scar tissue. However, it was eventually demonstrated through microscopy that friction massage increased fibroblastic proliferation, which is essential for synthesizing and maintaining collagen, fibronectin, proteoglycans, and other proteins of the connective tissue matrix for tissue repair. 5 Judgment regarding technique rationales must be withheld until scientific documentation confirms the reason a method works. What is most important is that the technique creates consistently positive results.
Literally hundreds of soft tissue techniques exist, among them friction massage, Active Release Techniques (ARTs), postisometric relaxation, postfacilitation stretch, counterstrain, myofascial release, and muscle energy technique. This chapter surveys a variety of common soft tissue methods. It will not make the practitioner an expert in these techniques; rather, it provides a clear rationale for soft tissue work and a basis for further education in these methods. All soft tissue techniques require hands-on supervision and practice.
Soft tissue techniques require the use of the hands as a sensor to evaluate the status of soft tissue. The practitioner learns to feel for end ranges of motion, barriers, and looseness, as well as types of tissue organization often characterized as “lumpy,” “leathery,” “stringy,” “doughy,” “boggy,” “nodular,” “mobile,” “taut,” and “springy.” Through manual palpation, the skilled practitioner discerns change in the tension of tissues, which helps determine the type of soft tissue treatment best suited to the patient’s needs and to monitor progress and patient response to treatment.
Certain soft tissue techniques are most effective in acute conditions, whereas others are effective in both acute and chronic conditions. The larger the number of effective soft tissue techniques in the practitioner’s repertoire, the better the overall quality of care.
Effect of Mechanical Load on Soft Tissue
Mechanical load on soft tissues, such as compression and tensile loading (Chapter 6), has been experimentally evaluated. Research has demonstrated that the form and function of musculoskeletal soft tissues are influenced by mechanical loading. 5 Loading methods such as transverse friction massage, deep massage, and the use of Graston instruments, can now be explained on a cellular level. Davidson and colleagues5 have produced a remarkable study on the effect of soft tissue mobilization on the rat tendon. By way of light and electron microscopy, the effects of augmented soft tissue mobilization (i.e., Graston technique or friction massage) on injured rat Achilles tendon causes an absolute increase in fibroblast proliferation. Gehlsen and colleagues7 have demonstrated that the proliferative response is directly dependent on the magnitude of the applied pressure.
Kolega8 has found that stretching tissues with mobile clusters of epithelial fibroblasts causes the microfilaments within the cells to align along the long axis of that tension, thus offering a structural mechanism for fibroblast realignment with longitudinal mechanical stress. As a result, loading the tissue (in this case by stretching) alters the structure of the cytoskeleton (i.e., the microfilaments that make up the structure of the cell). This allows the fibroblasts produced by mechanical load (e.g., stretching, friction massage), which eventually become new collagen, to form with normal longitudinal lines of stress rather than with an abnormal cross-linking pattern. Excessive cross-linking of collagen is responsible for restrictive inelastic tissue, resulting in the potential for soft tissue abnormalities and eventual pain. Many studies8 have shown that “cells in muscle, tendon, ligament, skin, and cartilage generally respond to ‘windows’ of increased loading by increasing matrix synthesis, increasing metabolic activity, and increasing cellular replication rates, and modifying their production of matrix components.”
A piezoelectric phenomenon is another important effect of mechanical load on soft tissue. 9 Massage, especially deep massage, causes deformation of collagen, which generates electrical signals. Piezoelectricity (i.e., pressure electricity) is the result of mechanical energy turning into electric energy. The effect is activation of the healing processes by the creation of electrical commands into the extracellular matrix, which affects extracellular events such as the proper alignment of collagen bundles in tendons, fascia, ligaments, and arteries. 10 Piezoelectric energy is currently used in medicine to accelerate fracture healing and callus formation.
Transverse friction massage (TFM) is localized pressure usually administered on a ligament or on the components of muscle (e.g., belly, musculotendinous portion, body of the tendon, insertion). It has recently been described for use on chronically painful bursae. 11 This technique is extremely valuable in the treatment of tendinosis, ligamentous sprains, muscular lesions, and chronic bursitis. It is useful in both acute and chronic conditions, depending on the condition and area involved. Light friction may be used on a recent partial tear and in recent ligamentous sprains, but caution is required because cells in the process of repair are in an immature state. The application of stronger friction, respecting the patient’s tolerance, is useful in the chronic stage.
Cyriax, 4 a medical physician, has proposed that the pressure and movement concentrated in a small local area by TFM can create greater therapeutic movement than strenuous exercise or manipulation. He states that TFM creates traumatic hyperemia (increase in blood) and movement that breaks down connective tissue (CT) adhesions. Recent studies on the effect of loading on cells has shown increased matrix synthesis, increased metabolic activity, increased cell replication rates (i.e., fibroblastic proliferation), and remodeling of matrix. 11 The digital stimulation of TFM acts on the local mechanoreceptors and may create temporary anesthesia, allowing for increased levels of pressure. After 10 to 20 minutes of TFM, if the massage is terminated while anesthesia is still present, functional isometric muscle testing of the involved area will demonstrate decreased pain, providing positive feedback to both doctor and patient. 12
The exact placement of the practitioner’s finger is extremely important. Cyriax emphasizes a functional evaluation of the area stressing particular tissues, thus allowing the practitioner to apply friction to the precisely correct location. He notes that the most painful area is not necessarily the source of the pain and that painful isometric muscle testing often reveals a pain source that is not the most tender area.
The practitioner’s finger and the patient’s skin should move as if they are attached. Otherwise, the skin will be frictioned, and bruising will occur. Knowledge of surface anatomy is necessary to ascertain that the exact location is being treated. Recent cadaver studies have demonstrated new approaches to palpation for some rotator cuff muscle and tendon areas. 13
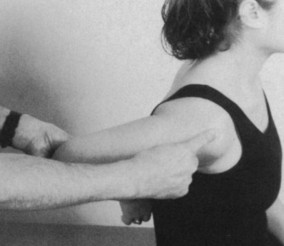
The new optimal position for palpating the supraspinatus insertion for maximum exposure has the patient sitting, with arm behind back, in maximal adduction, with medial rotation, and up to 30 to 40 degrees of hyperextension, depending on patient tolerance (Fig. 13-1). The maximal exposure for palpating and treating the insertion of the teres minor and infraspinatus has the patient sitting with shoulder in flexion to 90 degrees, combined with 10 degrees of shoulder adduction and 20 degrees of shoulder lateral rotation (Fig. 13-2).
 |
| Fig. 13-1 Optimal position for palpating and treating supraspinatus tendon insertion. |
 |
| Fig. 13-2 Optimal position for palpating and treating insertion of infraspinatus and teres minor (just below infraspinatus). |
Cyriax, 4 who used injectable steroids for many conditions, nevertheless considered certain anatomic areas curable only by deep friction. These include the following:
• Belly of the subclavius
• Musculotendinous junction of the supraspinatus
• Long head and lower musculotendinous junction of the biceps
• Belly of the supinator
• Ligaments about the carpal lunate bone
• Adductors of the thumb
• Interosseous belly at the hand
• Interosseous tendon at the finger
• Intercostal muscles
• Oblique muscles of the abdomen
• Lower musculotendinous junction of the iliopsoas (Fig. 13-3)
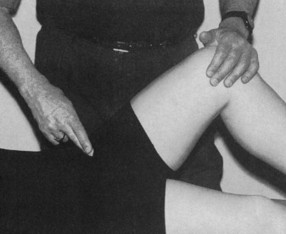 |
| Fig. 13-3 Position for friction massage of lower musculotendinous junction of iliopsoas. |
• Quadriceps expansion at the patella
• Coronary ligament of the knee
• Lower musculotendinous junction of the biceps femoris
• Musculotendinous junction of the anterior and posterior tibial and peroneal
• Posterior tibiotalar ligament
• Anterior fascia of the ankle joint
• Interosseous belly at the foot
ACTIVE RELEASE TECHNIQUES
Developed by chiropractor P. Michael Leahy, ART is a patented method used for the examination, diagnosis, and treatment of repetitive stress disorders such as carpal tunnel syndrome and epicondylosis (i.e., tennis elbow).141516 and 17 Leahy states that acute injury or repetitive injury of a constant pressure or tension may lead to a cumulative injury cycle, which may result in a state of adhesion and fibrosis. 14 Unless connective tissue is free of adhesions, a traction neurodesis may occur, resulting in peripheral nerve entrapment. A traction neurodesis represents fibrosis (formation of fibrous tissue) around the nerve, resulting in the nerve being stretched instead of performing its normal gliding function. Peripheral nerves must be able to glide during movement. For example, the brachial plexus moves 15.3 mm during shoulder abduction or adduction, and median nerve excursion proximal to the elbow is 7.3 mm during full elbow flexion and extension. 14 Any restriction to this motion will affect transmission of impulses through the peripheral nerve. Peripheral nerve entrapment is far more common than spinal nerve root entrapment.
As with all other soft tissue techniques, ARTs require a hands-on learning experience. Through palpation, the practitioner must evaluate tissue texture, tension, movement, and function, along the lines of the PARTS (Pain/tenderness; Asymmetry; Range-of-motion abnormality; Tissue tone, texture, and temperature abnormality; and Special tests) paradigm described in Chapter 10. According to Leahy, it is possible to determine the duration of a condition through skilled palpation. 14 For example, in the inflammatory phase (i.e., 24 to 72 hours after injury), a movable, fluidlike swelling with associated signs of inflammation may be palpated. After 2 days to 2 weeks, a “stringy, guitar string” feeling will be elicited. A lumpy feeling will be palpated after 2 weeks to 4 months, and finally after 3 months a leathery feeling will be present.
ART is an appropriate treatment for the failed carpal tunnel surgery discussed at the beginning of this chapter. It is an excellent procedure for treating entrapment of the median nerve as it passes through or under the pronator teres muscle. Often percussion of the pronator teres at its midbelly elicits a positive Tinel’s sign, referring paresthesia (abnormal sensation such as burning or prickling) to the median nerve distribution in the hand.
POSTISOMETRIC RELAXATION
Lewit uses postisometric relaxation (PIR) to relax tense muscles, comparing this method with the Travell spray-and-stretch technique. 2 For muscle tension caused by spinal fixation or viscerosomatic reflexes, this technique will not be effective. The patient with acute whiplash and muscle spasm offers the classic case for the appropriate use of PIR, with treatment directed to the upper trapezius.
The technique is as follows (Fig. 13-4):
1. The practitioner lengthens the muscle until the slack is taken up at the point where slight resistance is encountered without creating pain.
2. The patient is then asked to contract the muscle isometrically with minimal force (this should cause little or no pain) and to inhale and look with the eyes to the side of contraction. The patient should contract the muscle for 10 seconds. Gaymans18 has shown that inhalation has a facilitating effect on muscles and exhalation an inhibiting effect; moving the eyes toward the side of muscle activity facilitates the contracting muscle, whereas looking away from the side of contraction inhibits the contracting side.
3. The patient is then told to “let go,” to relax, exhale, and look in the opposite direction. The practitioner allows the muscle to lengthen by spontaneous decontraction. Relaxation can last 10 to 20 seconds, as long as the muscle lengthens, at which point a new barrier is reached. The procedure can be repeated three to five times. If the patient has difficulty relaxing, the isometric contraction phase can be increased up to 30 seconds.
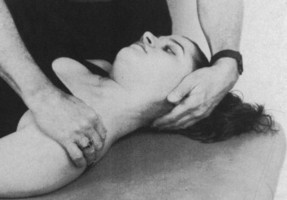 |
| Fig. 13-4 Patient lets go, exhales, and looks in opposite direction as practitioner allows muscle to lengthen by spontaneous decontraction. |
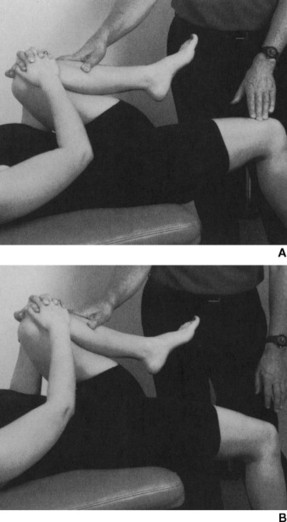
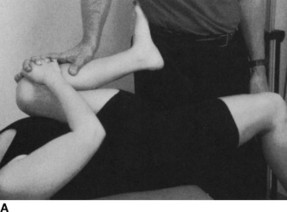
An example of appropriate use of PIR for the lower extremity would be a patient who is in acute pain and who is forward flexed as a result of iliopsoas spasm assumes a modified Thomas position (Fig. 13-5, A, under postfacilitation stretch); a flexed right hip is observed because of spasm of the right iliopsoas. The patient executes the same procedure as performed for the upper trapezius, but in this case the eyes look up during inspiration. The doctor exerts minimal pressure on the knee, feeling the psoas contract (Fig. 13-6, A). During inspiration phase, the patient may minimally contract isometrically as long as pain is not elicited. Fig. 13-6, B, shows the patient “letting go” with expiration and eyes downward for 10 to 20 seconds or until relaxation occurs.
 |
 |
| Fig. 13-5 A, Modified Thomas’ test indicating a tight right iliopsoas. Note slight flexion of right hip. B, Patient isometrically resists doctor’s pressure for 7 seconds. C, Patient lets go, and doctor stretches iliopsoas for 12 seconds. |