Chiropractic adjustive and manipulative techniques fall within the broad classification of manual procedures. As the term indicates, manual procedures encompass all therapeutic procedures performed or administered by hand. 1 Although this form of health care intervention has been traced to numerous ancient civilizations throughout the world, 2 only within the last century has it gained significance in the realm of mainstream health care, primarily via the growth and development of the chiropractic profession.34 and 5
Chiropractic offers a wide variety of technique systems. Many successful chiropractors draw on a variety of techniques, with each chiropractic adjustive procedure made richer through integration with others in a process of cross-fertilization. Although no single technique system can solve all problems, chiropractic technique should be nothing less than systematic. Approaching patients with a systematic method that is also eclectic is possible.
Manual procedures may be divided into two general categories:
• Joint adjustment and manipulation, including spinal and extremity adjustment and manipulation, manual traction-distraction, and the use of mechanical devices to aid adjustment and manipulation
• Adjunctive manual methods, including mobilization; manual soft tissue approaches such as point pressure techniques, massage, therapeutic muscle stretching; and visceral techniques (Box 12-1)
Box 12-1
CLASSIFICATION OF MANUAL METHODS
JOINT ADJUSTMENT AND MANIPULATION PROCEDURES
Adjustment
Manipulation
Manual traction or distraction
Mechanical devices to aid adjustment
ADJUNCTIVE MANUAL PROCEDURES
Mobilization
Point pressure techniques
Massage
Therapeutic muscle stretching or relaxation
Visceral techniques
A detailed study of all techniques and procedures in these categories is well beyond the scope of this chapter. This section offers the reader an overview of the more commonly used methods employed in the practice of chiropractic.
Joint manipulation procedures are techniques designed to introduce motion into a joint. These procedures may involve the application of a dynamic thrust, as in many adjustive procedures, or they may be of a nonthrusting nature, as in mobilization and traction-distraction procedures. 1,3,6 In either case, the procedure is specifically intended to affect some element of the neuromusculoskeletal system and, in doing so, to produce beneficial results for the patient via the action on the tissues involved. Although the precise mechanism of action is not fully understood, various authors believe it to be the result of improved intra-articular relationship (alignment), restoration of proper joint range of motion, improved nerve function, and reduction in tissue irritation and dysfunction.1378910 and 11
Careful distinctions, often based on interpretations of varying perspectives or philosophies in chiropractic, have been drawn between the terms manipulation and adjustment. Much has been written on the subject, with the distinguishing characteristic being that a chiropractic adjustment uses a specific short-lever osseous contact point (such as a transverse or spinous process) to correct a segmental misalignment or joint dysfunction, whereas a manipulation, commonly performed outside the scope of traditional chiropractic, uses longer leverage to increase range of motion, usually with less specificity. Some chiropractors would add that an adjustment corrects nerve interference or in some other way exerts a normalizing effect on the nervous system, whereas manipulation is intended to affect only musculoskeletal structures by mechanisms such as increasing joint range of motion. An important point to note is that some chiropractors within the profession use the terms adjustment and manipulation as synonyms. However, using the terms interchangeably usually describes the procedure in the context of a short-lever, specific contact manual procedure that uses controlled force, leverage, direction, amplitude, and velocity directed at specific joint or anatomic regions.
In this chapter, the terms adjustment and manipulation are interpreted more operationally than they are philosophically. The term manipulation refers to a high-velocity, low-amplitude (HVLA) thrust, sometimes simply described as a dynamic thrust, that moves a joint into the paraphysiologic joint space (see Fig. 10-4 in Chapter 10), beyond what is accessible through active and passive movements. The term adjustment refers to procedures designed to effect improvement in the neurologic component of vertebral subluxation, or joint dysfunction. Therefore the terms adjustment and manipulation are not mutually exclusive. An adjustment may use a manipulative (i.e., thrusting) approach, although it need not. An adjustment may use a different approach instead, such as having the patient lie on padded wedges or delivering a force using a percussive device. Similarly, a manipulation may be intended to adjust the spine (reduce nerve interference) but does not have to be delivered with this intent in mind. In this chapter, the context therefore defines whether the term manipulation or adjustment is more appropriate.
The terms chiropractic adjustment or chiropractic manipulation include a wide variety of manual and mechanical procedures applied with the intent of correcting a clinically identified adjustive/manipulative lesion (e.g., subluxation, muscle dysfunction, motion dysfunction). 3 The adjustment is characterized by the application of a specific dynamic thrust using controlled force, leverage, direction, amplitude, and velocity directed to a joint of the axial or extremity skeleton, after the involved joint has been tensioned to the end of its physiologic limits. The clinician must control the speed, amplitude, and direction of the thrust precisely1 to ensure the effectiveness of the procedure and minimize patient discomfort.
The adjustive or manipulative procedure forms the foundation of chiropractic case management and constitutes the most common procedure associated with the practice of chiropractic. 1,3 Simply stated, the procedure is characteristic of the profession and represents application of the chiropractic art. As such, the student, as well as the practitioner of chiropractic, must devote significant time and energy to developing and maintaining the necessary cognitive and psychomotor skills.
Adjustive Procedures Decision Making
Once a clinical impression is determined, the chiropractor must decide if manual procedures are indicated. The decision to apply this intervention must be balanced against the existence or absence of pain and the extent of the functional limitations. If no contraindications for the adjustment/manipulation are present, the chiropractor may choose from a wide variety and styles of procedures. Factors influencing the selection of manipulative procedures include4:
1. Age of the patient
2. Acuteness or chronicity of the problem
3. General physical condition of the patient
4. Clinician’s size and technical abilities
5. Effectiveness of the previous therapy, present therapy, or both
Other factors to consider are knowledge of the local anatomy, including the geometric planes of the articulations, the nature of the condition and presence of co-morbidities, and the mechanical characteristics of the adjustive/manipulative procedure. These factors will determine whether to use a long- or short-lever procedure, the positioning of the patient, specific contact points, the magnitude and vector of the force, and the type of thrust. Box 12-2 lists the factors governing the selection of adjustive methods.
Box 12-2
FACTORS GOVERNING THE SELECTION OF AND SPECIFIC APPLICATION OF ADJUSTIVE METHODS
ANATOMIC LOCATION OF JOINT DISORDER OR DYSFUNCTION
Morphology of tissues: size, strength, and mobility of structures. Some areas necessitate more power (mass and leverage).
PATIENT’S AGE AND PHYSICAL CONDITION
Ability to assume specific positions
Degree of pretension (force, mass, leverage, and depth of thrust) the patient can withstand
Stress to adjacent spinal or extremity joints and soft tissues
PATIENT’S SIZE AND FLEXIBILITY
Large or inflexible patient: needs increased mechanical advantage in the development of pretension and thrust
Table selection: height, articulating versus nonarticulating, release or drop pieces, mechanized
Method: leverage and type of thrust (e.g., push versus pull)
Flexible patient
Focus force by preloading the joint: removal of articular slack, use of nonneutral patient positions
Selection of method: shorter lever methods
PRESENCE OF MITIGATING DISORDERS OR DEFECTS
Preexisting congenital or developmental defects
Preexisting degenerative defects
Coexisting disease states
Adjacent motion segment instability (focused force minimizes stress to adjacent joints)
DOCTOR’S TECHNICAL ABILITIES AND PREFERENCES
PATIENT’S TREATMENT PREFERENCES
Cannot compromise safety and effectiveness
SPECIFIC MECHANICAL AND PHYSICAL ATTRIBUTES OF ADJUSTIVE METHODS
Adjustive localization and pretension
Patient position
Doctor position
Contact points
Leverage
Adjustive thrust
Leverage
Velocity
Amplitude (depth)
Mass
Point of delivery
Pause-nonpause
Short lever preferred to long lever
Issue of specificity
Patient of manageable size
Flexible patient
Patients with clinical motion segment instability
Long lever preferred to short lever
Spinal regions where additional leverage is desired
Patient size and flexibility demand additional leverage and power
From Peterson DH, Bergmann TF: Chiropractic technique: principles and procedures, ed 2, St Louis, 2002, Mosby.
As stated earlier, a wide variety of manual procedures are available from which to choose. As properly applied adjustment or manipulation is usually specific, induces joint separation, and is free of pain. The procedure should not produce joint compression, injury, or distractive forces at adjacent, undesired segmental levels. Achieving adjustive specificity depends on the procedures leading to adjustive localization and the actual delivery of the adjustive thrust. According to Peterson and Bergmann1“adjustive localization refers to the preadjustive procedures designed to localize adjustive forces and joint distraction.” Adjustive localization depends on proper patient positioning, doctor positioning, and adjustive contact points. Once appropriate preadjustive tension is developed, the application of a specific, controlled force can be applied. This force, when accompanied with a specific vector (line of drive), is known as the adjustive thrust. Together, adjustive localization and the adjustive thrust will improve adjustive specificity and minimize the effects of unwanted distractive forces to adjacent joints (Box 12-3).
Box 12-3
ACHIEVING ADJUSTIVE SPECIFICITY
ADJUSTIVE LOCALIZATION AND PREADJUSTIVE TENSION
Patient position
Doctor position
Doctor’s contact point
Doctor’s indifferent (supporting) hand
Segmental contact point
Tissue pull
ADJUSTIVE THRUST
Line of drive (vector)
Type of thrust
Adjustive Localization and Preadjustive Tension
Patient Position
The patient may be placed in several positions before and during the adjustment/manipulation. Each posture offers different advantages and disadvantages for both the clinician and the patient. Proper patient positioning is crucial when developing preadjustive tension and achieving adjustive specificity. Standard patient postures include prone, supine, standing, sitting, knee-chest, and side lying.
Supine: The patient lies on his or her back. The table headpiece is slightly raised to support the patient’s head.
Standing: The patient is erect with his or her feet shoulder-width apart allowing for appropriate balance. This position is commonly used for assessment (postural analysis, sacroiliac dynamic [motion] palpation) and upper extremity adjustment/manipulation procedures.
Sitting: The sitting posture is commonly used during cervical and upper extremity adjustive/manipulative procedures. Thoracic and lumbopelvic procedures can also be performed in the sitting position.
Knee-chest: The patient is placed in a kneeling position with his or her chest, neck, and head supported on a special table (Fig. 12-1). This position may be used when adjusting the thoracic and lumbar spines. The knee-chest position, similar to the prone position with the breakaway abdominal suspension piece released, does not restrict lower thoracic and lumbar extension, thus decreasing resistance to the posterior-to-anterior thrust. Therefore the clinician should exercise care regarding the depth of the posterior-to-anterior thrust.
 |
| Fig. 12-1 An adjustment of the thoracolumbar junction with the patient positioned on a knee-chest table. |
Side lying (side posture): The patient is lying on his or her side with the table headpiece elevated to support the head and neck. The lower shoulder is placed slightly anterior so that the patient’s upper torso is resting on the scapula and not on the shoulder itself. The lower arm is placed across the patient’s chest with the hand resting on the anterior deltoid of the upper shoulder. The upper leg is flexed at the hip and knee, and the foot is placed in the popliteal fossa of the lower leg (Fig. 12-2).
 |
| Fig. 12-2 Side-posture position. (From Peterson DH, Bergmann TF: Chiropractic technique: principles and procedures, ed 2, St Louis, 2002, Mosby.) |
Many mechanical devices and sophisticated tables have been designed to enhance the comfort and positioning of the patient and assist the clinician in the delivery of the adjustment. These devices and aids are briefly discussed later.
Doctor Position
The doctor position may refer to the position of the doctor in reference to the patient or to the type of stance or body posture the doctor is maintaining during a specific adjustive/manipulative procedure. The following list describes the doctor’s position in reference to the patient:
• Caudad: The doctor is facing toward the feet of the patient.
• Ipsilateral: The doctor is standing on the same side as the segmental contact point. For example, while making a hypothenar contact on the left transverse process of T6, the doctor may stand on the ipsilateral side, or left side, of the patient.
• Contralateral: The doctor is standing on the side of the patient opposite the segmental contact point.
In addition to these positions, the doctor may position himself or herself in a square stance or a staggered (fencer’s) stance. In a square stance, the doctor’s feet are approximately shoulder width apart and aligned in the coronal plane. The knees and hips are slightly flexed to allow the doctor to be comfortably positioned over the patient while maintaining an erect, neutral spine. When accommodating a lower table height, the doctor should avoid bending at the waist, and instead widen his or her stance, bending at the hips and knees while maintaining a neutral spine. In a staggered or fencer’s stance, the doctor positions one foot forward and one foot back. The knees are bent, and the doctor’s spine is maintained in a neutral position. As with the square stance, the doctor’s hip and knees should bend while accommodating a lower table. This stance allows the doctor to transfer his or her weight from the back foot to the front foot during the adjustive/manipulative thrust.
Doctors’ positioning and stance is the foundation for a balanced and controlled adjustive/manipulative procedure and is an essential component for achieving comfort for both the doctor and the patient. Positioning and stance is the foundation for a balanced and controlled adjustive/manipulative procedure. During the patient and doctor setup, the clinician should attempt to place his or her center of gravity over or near the segmental contact point (see later discussion). By controlling the center of gravity and using one’s body weight appropriately, the doctor can increase the efficiency (by saving energy) of the adjustment/manipulation and reduce unwanted stresses to the doctor’s upper extremity.
Performing manual procedures can be physically demanding. Occupational risks for the doctor of chiropractic are significant when performing numerous procedures all day long, day after day, and year after year. By being aware of sound body mechanics, established with appropriate doctor positioning, the chiropractor can decrease the risk of common postural and repetitive disorders.
Doctor’s Contact Point
Approximately 12 areas on the hand (Fig. 12-3) can be used to specifically contact the patient.11213 and 14 The doctor’s contact point is an attempt to localize the adjustive force to a specific area on the patient (i.e., the transverse process, spinous process, or lamina). However, an overly prominent or bony contact point (e.g., pisiform) can sometimes be uncomfortable or painful for the patient. The clinician must attempt to be firm but comfortable with the various hand contact positions.
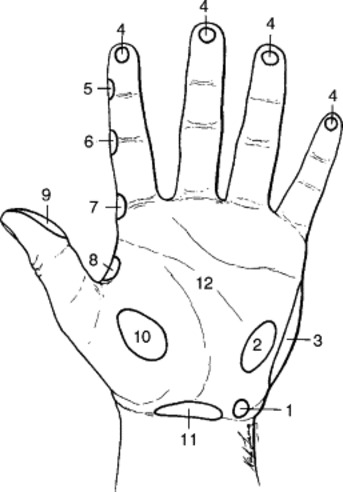 |
| Fig. 12-3 Contact points of the hand: (1) pisiform; (2) hypothenar; (3) metacarpal or knife-edge; (4) digital; (5) distal interphalangeal (DIP); (6) proximal interphalangeal (PIP); (7) metacarpophalangeal or index; (8) web; (9) thumb; (10) thenar; (11) carpal; and (12) palmar. (From Peterson DH, Bergmann TF: Chiropractic technique: principles and procedures, ed 2, St Louis, 2002, Mosby.) |
Many adjustive/manipulative procedures can be executed using several different contact points. The selection of which specific area of the hand a clinician uses is often a result of personal preference rather than one contact point being more efficient or specific than another.
Doctor’s Indifferent (Support) Hand
The hand that is used to stabilize the patient, support adjacent joint structures, or reinforce the contact hand during an adjustive/manipulative procedure is known as the indifferent or support hand. The indifferent hand is also used to assist the contact hand during the adjustive/manipulative thrust. For example, when adjusting/manipulating lateral to medial glide of the ulna on the distal humerus at the elbow, both hands deliver a low-amplitude, dynamic thrust in opposite directions. At other times, the indifferent hand may support the patient’s head while positioning the patient’s neck for a cervical procedure aimed at reducing a rotation dysfunction. When performing lumbopelvic side-posture procedures, the indifferent hand is used to contact the patient’s upper torso in a manner that helps stabilize the patient throughout the procedure.
Segmental Contact Point
Segmental contact points are anatomic structures, commonly referred as bony landmarks, located on the patient. Examples of common bony (osseous) landmarks used as segmental contact points are listed in Table 10-1. The clinician uses these structures as focal points for the adjustive force. That is, although many of these points are under deep layers of soft tissue, the doctor contacts over or near these osseous points in an attempt to generate forces to the specific segmental contact points. How close the doctor’s contact point is to the segmental contact point defines the difference between short- and long-lever adjustive procedures. Peterson and Bergmann1 have the following to say about short- and long-lever procedures:
Adjustive contacts established at or near the level of the dysfunctional joint are referred as short-lever (direct) adjustments. Adjustive contacts established at some distance from the level of the dysfunctional joint are referred to as long-lever (indirect) adjustments…
Additional information about short- and long-lever procedures will be described later in this chapter.
Tissue Pull
Establishing a firm contact over the segmental contact point is extremely important. Possible slipping away from the intended target point when applying the adjustive/manipulative thrust may dissipate the force and decrease the specificity of the procedure. 1,13 One precaution to avoid slipping or unnecessary movement involves the use of tissue pull. Tissue pull is established by applying traction to the superficial soft tissues over the segmental contact point. The indifferent hand is commonly used for this purpose. Typically, one finger of the indifferent hand tractions the soft tissue overlying the segmental contact point in the direction of the adjustive thrust (line of drive). While maintaining the traction, the finger of the indifferent hand is withdrawn and simultaneously replaced by the doctor’s contact point of the thrusting hand, allowing a secure and specific contact between the doctor and the patient.
Adjustive Thrust
Line of Drive (Vector)
The line of drive (vector) indicates the direction of the adjustive thrust. Along with the plane of the articulation, the line of drive determines the movement of the articular segment. Appropriate adjustive/manipulative vectors are necessary to induce joint distraction at desired joint levels. Vectors aimed in unsuitable directions may induce joint compression, cavitation, or both at undesired levels. (Cavitation is the formation of vapor and gas bubbles within fluid through the local reduction of pressure. HVLA adjustments and manipulations are theorized to produce a cavity within a joint, eliciting a characteristic cracking sound.) The line of drive is commonly described in anatomic terms. For example, a clinician may induce a line of drive from posterior to anterior and inferior to superior while contacting the right transverse process of T7. The following common anatomic terms are used to describe specific line of drives:
| Posterior to anterior | P-A |
| Anterior to posterior | A-P |
| Inferior to superior | I-S |
| Superior to inferior | S-I |
| Medial to lateral | M-L |
| Lateral to medial | L-M |
Anatomic descriptors are used in one plane of movement, as with P-A, or they can be used in combination, as with P-A and I-S. Notably, however, a single adjustive thrust may not prove sufficient to restore mobility to more than one direction of restriction. Several thrusting procedures, all with different vectors, may be necessary to normalize a single spinal motion unit or peripheral joint complex.
Type of Thrust
Dynamic adjustive thrusts can be divided into two physical forms: recoil thrusts and impulse (dynamic) thrusts. Recoil thrusts are HVLA ballistic thrusts that are immediately followed by a passive recoil. The thrust is initiated by simultaneously contracting the extensor muscles of the arms (triceps and anconeus) and pectorals. The force of the thrust should be applied equally with both arms, with the doctor positioned such that a straight line can be drawn from the doctor’s episternal notch to the segmental contact point. Immediately following the thrust is a rapid recoil of the doctor’s arms created by the relaxation and a rebound effect of the extensor muscles of the arms. The recoil thrust is commonly used with the joints in the neutral position, with little to no preadjustive tension (Fig. 12-4, A).
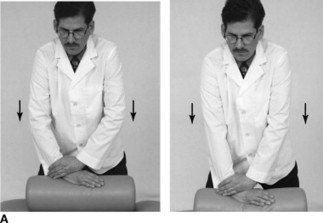 |
 |
| Fig. 12-4 A, Illustration of recoil thrust. The body is held in stationary position, and the thrust is generated by rapid acceleration at the elbows. The thrust is very shallow, with a quick termination, followed by an elastic recoil (the recoil phase is not illustrated here) as full elbow extension is reached. B, Illustration of shoulder-drop thrust. The body is held in a stationary position, and the thrust is generated through a quick depression (elongation) at the doctor’s shoulder. The doctor maintains a light contact after terminating the thrust to dampen reverberations generated by the shoulder thrust. C, Illustration of body-drop thrust. The thrust is generated by accelerating the doctor’s body weight through the adjustive contact. Transfer of body weight is generated by transferring weight from the doctor’s heels toward the front of his feet. This transfer is usually accomplished by inducing slight ankle dorsiflexion, knee flexion, and flexion of the trunk. Body-drop thrusts are often combined with shoulder-drop thrusts to produce a more rapid and rigid thrust and kinetic chain. (From Peterson DH, Bergmann TF: Chiropractic technique: principles and procedures, ed 2, St Louis, 2002, Mosby.) |
Preadjustive tension in a recoil adjustment is accomplished by exerting P-A pressure in the plane of the intervertebral disk or the vertebral body, maximizing the separation of the anterior bodies (i.e., increasing spinal extension) immediately before the dynamic recoil thrust is delivered. The depth and force of this adjustment is modulated through the degree of flexion in both arms at the time the thrust is delivered.
Impulse (dynamic) thrusts are HVLA procedures without the dramatic recoil following the thrust. Generating force with the doctor’s arms, body, or both can change the adjustive velocity. When less force is desired, as with cervical and some extremity joints, the thrust is generated with the arms only. When more force is desired, as with larger patients and using side-posture procedures, the doctor can transition additional weight from his or her trunk and lower extremity to the contact point. Impulse thrusts are commonly delivered when the target joint is near or at the elastic barrier and the joint is at tension. Shoulder drop and body drop thrusts are two examples of impulse thrusts (see Fig. 12-4, A and B).
CHIROPRACTIC SEGMENTALISM AND STRUCTURALISM
Throughout most of its history, starting with the Palmers, chiropractic has emphasized segmental subluxations, that is, spinal problems attributed to two adjacent vertebra and the related soft tissues. This emphasis has been generalized by all chiropractors to also include the atlantooccipital, lumbosacral, and sacroiliac joints, and by many chiropractors to also include the extremity joints. On the other hand, a structuralist or posturalist tendency has existed as well, probably starting with the work of Carver, which emphasized spinal regional considerations, and beyond that, the relation of the various spinal regions to one another.
The segmentalist chiropractor asserts that subluxations occur at specific motor units consisting of two bones, be they vertebrae, the skull, any of the pelvic bones, or combinations thereof. As a general rule, the segment above is characterized with respect to the one below, whether solely for the purpose of creating a readily understandable clinic record or to indicate the specific contact point for the adjustment. From the segmentalist perspective, subluxation in the specific motor unit results in postural distortions, such as scoliosis in the frontal plane, and loss or exaggeration of the two kyphotic and two lordotic curves in the sagittal plane. These postural distortions are seen as compensatory consequences of specific segmental subluxations and not as the problems in and of themselves. Gonstead technique is a classic example of the segmentalist approach.
The structuralist or posturalist chiropractor sees postural distortion as the subluxation in and of itself and proposes a language of listings that describes the linear and angular relationship of entire regions of the axial skeleton. A given motor unit (composed of two vertebrae and contiguous soft tissues) may exhibit more signs and symptoms of dysfunction than another, but this is seen by the posturalist to be the consequence rather than the cause of the primary postural distortion. For example, the apex of a lateral curvature in the frontal plane may present with more pain, and show more osteophytosis (degeneration) on x-ray, than the other segments that comprise the curvature. Nonetheless, the curvature, not its apex, is considered the subluxation. The posturalist claims that the spine subluxates as groupings of adjacent vertebrae and is to be adjusted accordingly, with relatively nonspecific contacts. Pettibon’s Spinal Biomechanics and Harrison’s Chiropractic Biophysics are classic examples of posturalist approaches.
An essential point to note is that a third way exists, an eclectic approach to chiropractic technique in which clinicians need not choose between segmentalist and structuralist thinking, endorsing one and rejecting the other. More likely, individual patients are better understood as suffering from either segmental or regional complaints and that a segmental problem is very much affected by the local environment in which it occurs, just as the local spinal environment is partially governed by segmental problems.
SPINAL AND EXTREMITY LISTINGS
Spinal and extremity listings describe abnormal joint positions or movements. In common parlance, a listing is a direction of tilt, a leaning to one side. Chiropractors have been using this term since the profession’s beginning to describe the direction in which a vertebra has misaligned. A segment can be misaligned only with respect to some other reference point: the segment above or below, the floor, or perhaps the central ray of the x-ray tube. Chiropractors have not been able to agree on a standard listings system.
The following factors have interacted to confuse the discussion:
• A common reference point for listings is lacking.
• Many different methods can be used for obtaining listings, including x-ray, motion palpation, static palpation, muscle palpation, reflex methods employing leg checks, and kinesiologic challenges.
• Some practitioners use the vertebral body, and others use the vertebral spinous process, as the reference point for their listings system.
Certain rules of nomenclature have been adopted to facilitate discussion of biomechanical dysrelationships. For example, if one supposes that a segment can be seen on a spinograph to reside anteriorward in relationship to the segment below, should one describe this situation in terms of an anteriority of the superior segment or a posteriority of the inferior segment? Established among medical physicians, as well as chiropractors, is that this condition should be termed an anterolisthesis (slipping forward or anterior misalignment) of the segment above. Unfortunately, this convention is seen by some clinicians to contain mechanical significance, with the inference that the superior segment has subluxated and should be contacted directly in any corrective thrust.
The terminologic convention should not imply that the underlying biomechanical fault resides in the one segment rather than the other, because the subluxation actually occurs in the joint between the two. Furthermore, no a priori reason exists to suppose that when a clinician attempts to reduce the subluxation by applying a thrust, the force that is applied moves a segment with respect to the one below any more than with respect to the segment above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







