Antalgic
Palpation is a cornerstone of manual adjusting procedures. Many hours of practice and concentration are necessary to master this art. Manual palpation is the chiropractor’s primary evaluative intervention and is used in combination with other diagnostic methods of chiropractic case management. The very core of adjusting lies in the ability to identify contact landmarks, contracted muscles, inflammation, restrictions of movement, and hard end-feel resistance. This chapter describes different forms of palpation and the best methods of learning these skills.
Aside from its unsurpassed value in enabling the chiropractor to determine the most advantageous adjustive strategies, palpation can serve as a powerful doctor-patient communication tool, helping the patient understand the importance of following through on a recommended treatment plan. Patients can feel pain and resistance as the chiropractor palpates. In response to chiropractic care, patients feel diminished pain and restriction, often before their symptoms abate. Through skilled palpation, the focus subtly shifts away from an overemphasis on symptoms toward awareness of the changes the chiropractor is palpating and monitoring from one office visit to the next.
The reliability of palpating landmarks and decreased range of motion is not on a par with reading a thermometer, but it is comparable to cardiac auscultation and the reading of radiographs.1234 and 5 Quantifying a manual art is difficult because of the lack of a standard for comparison. Palpation is a skill that develops over time and must be nurtured. Tissues become warm, muscles atrophy and or go into spasm, joints block or become hypermobile, and these conditions can be felt. How well the chiropractor will be able to feel them depends on how seriously he or she chooses to practice the various palpation procedures described in this chapter.
IDENTIFYING THE ADJUSTIVE/MANIPULATIVE LESION
All professions that perform adjustment/manipulation involving the spine, an extremity, or both, describe the same phenomenon, using different nomenclature (Box 10-1). Traditionally, chiropractors have used the term subluxation complex to encompass all the mechanical, inflammatory, and neurobiologic components of this neuromusculoskeletal entity. The adjustive/manipulative lesion is the component to which chiropractic techniques are applied so as to impose a demand for increased function. When this procedure is successful, the body responds by restoring function to the joints adjusted. From this perspective, a dysfunction of the joint is involved, not a “bone out of place” misalignment. It is true that joints that regain movement can change their resting position, but an important point to recognize is that adjustment affects the joint’s ability to function in all its ranges of motion. Enhanced function changes the neurobiologic mechanisms and leads to the reduction of the inflammatory process. For these reasons, to identify when, where, why, and how often to adjust a patient, chiropractors need to be able to work with the following procedures and feel what is occurring specifically in each patient.
Box 10-1
DEFINITION OF TERMS DESCRIBING FUNCTIONAL OR STRUCTURAL DISORDERS OF THE SYNOVIAL JOINTS
Orthopedic subluxation: Partial or incomplete dislocation
Chiropractic subluxation: Aberrant relationship between two adjacent structures that may have functional or pathologic sequelae
Joint dysfunction: Joint mechanics showing functional disturbances without structural changes
Somatic dysfunction: Impaired or altered function or related components of the body framework (somatic system)
Osteopathic lesion: Disturbance of musculoskeletal structure, function, or both, as well as accompanying disturbances of other biologic mechanisms
Joint fixation (restriction): Temporary immobilization of a joint in a position that it may normally occupy during any phase of normal movement
Adapted from Peterson DH, Bergmann TF: Chiropractic technique: principles and procedures, ed 2, St Louis, 2002, Mosby.
COMPONENTS OF THE ADJUSTIVE/MANIPULATIVE LESION
As with other aspects of patient examination, the doctor of chiropractic uses observation, palpation, percussion, and auscultation when identifying the adjustive/manipulative lesion. Using the acronym PARTS modified from the osteopathic profession to identify somatic dysfunctions,6,7 Bergmann and Finer8 describe five diagnostic criteria (Pain and tenderness; Asymmetry; Range-of-motion abnormality; Tissue tone, texture, and temperature abnormality; and Special tests) for identifying joint subluxation or dysfunction.
Pain and Tenderness
Pain is the localized sensation of discomfort, distress, or agony reported by an individual. 9 By contrast, tenderness is defined as abnormal sensitivity to touch or pressure. 9 Although these reports are subjective signs, a skilled and experienced doctor can feel the tissue changes that correspond with patients’ feeling pain and tenderness. Identifying whether the pain lingers after the pressure of palpation is removed is significant. Pressure over inflamed tissues causes a lingering pain. Pressure and challenging the end resistance of a dysfunctional but noninflamed joint will hurt only while the pressure is applied. As a general rule, inflamed joints should not be adjusted until the inflammation has subsided and the postinflammatory pattern of joint dysfunction has appeared. Pain can occur with vibration, such as placing a tuning fork over a bone fracture. Traction and compression can elicit pain that is mild at rest; once again, whether it lingers is significant. The chiropractor can use various reliable and valid tools to measure and quantify pain. These tools include self-administered pain and functional questionnaires, algometry (the measurement of pressure or painful stimuli) visual analog scales (VAS), pain scales, pain diagrams, and pain drawings.
Antalgic (leaning to avoid pain) and asymmetric postures are common in acute presentations but are often within normal limits in mildly symptomatic patients. Therefore asymmetries and misalignments can occur on a segmental or a regional level. Observation of posture and gait often shows a gross distortion of the patients’ pelvis, spinal column, shoulders, knees, feet, and ankles. The forward displacement of a lumbar spondylolisthesis will be observed and palpated as a dimple (step defect), with the patient in a side-lying position. The spine is not normally perfectly symmetrical, and the chiropractor is unlikely to be able to palpate a displacement of a few millimeters based on the location of the spinous processes. As the spinal connective tissues degenerate, the resulting displacement is visualized on x-rays and other diagnostic imaging methods by placing patients in full flexion and extension suggestive of excessive intersegmental movement (hypermobility) or instabilities.
Range of Motion
Gross range of joint motion can be measured by using an inclinometer, protractor, ruler, plumb line, and various computerized methods. Ultrasound and motion x-ray studies have been used to observe and measure the complex intersegmental movement of spinal and extremity joints. Various systems of motion palpation have been described, and until an article by Marcotte and colleagues, 10 interexaminer reliability has been a major concern. Joints move, and the chiropractor can palpate that movement, but agreeing on which joints are not moving fully and by what degree of dysfunction has been a challenge. Many chiropractors use motion palpation to determine the joints to be adjusted and the line of drive (direction of dynamic thrust) they introduce into the joint complex. Other chiropractors simply use these records of the ranges of joint motion for evaluating a patient’s progress.
Active gross movement (the range-of-joint motion possible through the patient’s voluntary effort) is tested first. Passive gross movement is then tested, with the doctor pressing the range a little further. Accessory joint movements are tested at the end of the passive range of motion by springing further to see if a little elasticity is present, called the springy end feel. Intersegmental motion of spinal joints is well described in texts on biomechanics. The goal for all doctors of chiropractic is to be able to assess these rotations around the orthogonal axes to determine the correct adjustments to restore normal active, passive, and joint play movement. Many chiropractors use motion palpation to determine the specificity of the thrust into the directions of resisted end feel in a spinal motion unit or extremity joint. This procedure is demonstrated later in this chapter.
Tissue Tone, Texture, and Temperature
Tissue tone is determined by palpation, observation, instrumentation, and tests for the length and strength of muscles. The doctor should be able to palpate nodules to determine if they are loose or attached to bone, ligament, or tendon. In some areas, nerves are palpable, such as the ulnar nerve in the forearm. Classical diagnosis considers the liver palpable when it is enlarged, as are the lymph nodes, arterial pulses, and some hernias. The biceps tendon can be palpated when it slips out of the biceps groove of the humerus.
None of these skills are natural to a student, and perseverance is needed to become a professional. Soft, skillful hands convey an important sense of confidence to a patient, which promotes relaxation and minimizes guarding resistance to being adjusted. Short or hypertonic muscles will restrict the joint motion of the agonist, and these shortened antagonists will often be full of palpable nodules that need specific treatment before normal, active ranges of motion can be attained. A hamstring or quadriceps can feel similar to a ridged washboard because of these adhesions from past tears. Tissue swelling is easy to visualize, but by using palpation, the doctor can determine whether pitting edema is present. The fluids drawn into the legs by gravity in certain heart and kidney diseases causes pitting after pressure is applied. Joint effusion is a tight swelling and is quite painful when tested for pitting. Palpation of the deep muscles in the neck will often reveal a knotted feeling in the specific muscle responsible for a patient’s cervicogenic headache (see Chapter 24). These very common headaches often disappear when corrected by joint adjustment/manipulation and soft tissue procedures targeted at the chronic muscle spasm that has been identified through skilled palpation. Identifying normal and abnormal tissue characteristics is an art worth practicing and mastering.
Special Tests
Special tests include additional physical examination, laboratory procedures, or both, which aid in the differential diagnosis of joint dysfunction. Examples include orthopedic and neurologic tests, diagnostic imaging procedures, blood and urine testing, and electrodiagnosis. Testing procedures specific to a technique system, such as leg-length assessment, specific radiographic marking techniques, and particular muscle testing procedures, should also be considered.
DEFINITION AND CLASSIFICATION OF PALPATION PROCEDURES
Inspection, auscultation, and palpation are the three basic diagnostic methods used in conventional clinical medicine. 11 However, in an age of rapidly advancing technology with sophisticated diagnostic and laboratory equipment, palpation is underused in conventional medicine and is slowly becoming a lost art. To the contrary, palpation is recognized as an essential skill by chiropractors, osteopaths who use manipulation, and physical and manual therapists and is the most important tool that doctors of chiropractic can use to identify the manipulative/adjustive lesion. An important point to note is that, after a well-executed history, palpation provides the first direct physical contact with the patient. 12 The quality of this contact may strengthen existing trust or nullify positive rapport established between clinician and patient.
The foundations of palpatory literacy are knowledge of anatomy (cognitive) and the acute ability to touch and feel (psychomotor) 12 (Box 10-2). Although anatomic knowledge is primarily cognitive in nature, the development of psychomotor skill is a complex phenomenon that must be obtained by experience and practice. Thus developing good palpation skills requires many hours of practice and concentration. The skillful palpator who develops both tactile and kinesthetic sensation will also find the art of adjustment/manipulation easier to master.
Box 10-2
STATIC PALPATION TIPS
1. Use the least pressure possible. (Touch receptors are designed to respond only when not pressed too firmly.)
2. Concentrate on the area, structure, or both, which are to be palpated.
3. Try not to cause pain if possible. (Pain may induce protective muscle splinting and make palpation more difficult.)
4. Carefully penetrate to deeper structures. (Brisk progress may induce reflex muscle spasm.)
5. Try not to lose skin contact before completing the palpation of the area.
6. Use broad contacts whenever possible.
7. Close sight to increase palpatory perception.
Palpation procedures are commonly divided into static and dynamic assessments (Box 10-3). Static palpation is usually performed with the patient in a stationary position and includes bony (joint structures) and soft tissue assessment. Dynamic palpation, or motion palpation, is commonly performed to assess abnormal vertebral or extremity joint motion and is performed with the patient in a variety of positions.1314151617 and 18
Box 10-3
TYPES OF PALPATION
Static palpation
Bony
Soft tissue
Dynamic (motion) palpation
Active
Passive
Joint play
End play (end feel)
Accessory
Static Palpation
Static palpation of bony landmarks of the spine and pelvis includes assessment of spinous, transverse, and mammillary processes of the vertebrae and of the posterior superior iliac spine (PSIS), ischial tuberosities, and iliac crest contours of the innominate bones. Bony landmarks such as femoral condyles, olecranon processes, and greater trochanters are examples of bony landmarks commonly palpated around extremity joints. The evaluator should note any asymmetries or anomalies while keeping in mind that positional faults are unreliable and should be confirmed with additional evaluation procedures.
Palpatory tenderness has been shown to be a reliable method for identifying the adjustive lesion.19202122 and 23 However, a difference exists between palpation of pain and tenderness and tactile palpation. Tactile palpation provides thermal and mechanical information that aids in structural assessment and may correlate with previous examination and historical findings. Tenderness palpation, on the other hand, may help distinguish healthy from unhealthy tissues. 12 Healthy tissues can usually tolerate greater pressure than can injured or diseased tissues. In the absence of a destructive lesion, these tissue changes are important indicators of joint subluxation or dysfunction that may respond to manual treatment procedures.
Layer palpation is a systemic method of assessing the mobility and condition of myofascial and other soft tissue structures. 24 Palpation begins with the most superficial structures and proceeds to deeper tissues. Light palpation with the pads of the fingers is used to assess superficial tissues (Fig. 10-1). Deeper structures require increased pressure and should be performed in a firm but gentle manner. Anatomic landmarks commonly palpated are listed in Table 10-1.
 |
| Fig. 10-1 Light palpation with the pads of the fingers over the transverse processes of the thoracic spine. |
| EOP, External occipital protuberance; PSIS, posterior superior iliac spine; ASIS, anterior superior iliac spine. | ||
| Landmark | How to Locate | Clinical Significance |
|---|---|---|
| CERVICAL SPINE | ||
| EOP | Posterior. Midline projection of posterior aspect of skull at junction of head and neck. | Used as a reference landmark. Adjustive contact points lateral to EOP are commonly used with occipital (C0-C1) dysfunctions (subluxations). |
| C2 spinous process | Posterior. First bony point palpated in midline inferior to EOP. | Commonly used as an adjustive contact point and reference land mark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| C6 spinous process | Posterior. Moves (anteriorly) away from palpating finger during cervical extension; easily palpated in cervical flexion. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| C7 spinous process | Posterior. Most prominent spinous process in this region (T1 may be the most prominent in some individuals); C7 moves on T1 during cervical flexion and extension; C7 palpated throughout cervical flexion and extension. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| Cervical facet joints | Posterior. Palpated 1.5-2.0 cm lateral to spinous process. | Commonly used as an adjustive contact point. Soft tissues over these areas are commonly tender to palpation with facet joint sprains or strains, and dysfunctions (subluxations). |
| C1 transverse process | Lateral. Palpated between mastoid process (prominence of temporal bone posterior to ear) and angles of the jaw. | Used as an adjustive contact point. Tender with common conditions such as spinal dysfunctions (subluxations), sprains or strains, and postural syndromes. |
| THORACIC SPINE AND RIBS | ||
| T1 spinous process | Posterior. May be most prominent spinous process in this region; C7 moves on T1 during cervical flexion and extension; also located at the level of acromioclavicular joint. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| T3 spinous process | Posterior. Lies at the middle of a line drawn between medial aspects of spine of scapulae. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| T7-T8 spinous process | Posterior. Lies at the middle of a line drawn between inferior borders of scapulae. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| T1-T4 transverse process | Posterior. Palpated one interspinous space above spinous process lateral to midline. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| T5-T8 transverse process | Posterior. Palpated two interspinous spaces above spinous process lateral to midline. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| T9-T12 transverse process | Posterior. Palpated one interspinous space above spinous process lateral to midline. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| Second rib | Posterior. Palpated at superior border of scapula. | Serves as a reference landmark. |
| Seventh rib | Posterior. Palpated at inferior border of scapula. | Serves as a reference landmark. |
| LUMBAR SPINE AND PELVIS | ||
| L4 spinous process | Posterior. Lies at the middle of a line drawn between the highest points of iliac crests. | Commonly used as an adjustive contact point and reference landmark. Tender with spinal fractures, infections, sprain or strains, neoplasia, and dysfunctions (subluxations). |
| L4-L5 intervertebral disk | Posterior. Lies at the middle of a line drawn between the highest points of iliac crests. | Serves as a reference landmark. Soft tissues over this area are tender to palpation with intervertebral disk injury and syndromes. |
| Lumbar facet joints | Posterior. Palpated one interspinous space above spinous process and lateral approximately 1-1½ in. | Commonly used as an adjustive contact point. Soft tissues over these areas are commonly tender to palpation with facet joint sprains or strains, and dysfunctions. |
| S2 spinous process (sacral tubercle) | Posterior. Lies at the middle of a line drawn between PSIS. | Serves as a reference landmark and as a contact point for adjustments. |
| PSIS | Posterior. Skin dimples superior and lateral (approximately 4 cm from midline) to intergluteal cleft. | Commonly used as a reference landmark and as a contact point for sacroiliac adjustments. Tender to palpation with sacroiliac dysfunctions (subluxations) and sprains. |
| Tip of coccyx | Posterior. Lies at the middle of a line drawn between ischial tuberosities (approximately 2.5 cm postero-superior to anus). | Tender with fractures, sprains, and dysfunctions (subluxation) of the coccyx. |
| Ischial tuberosity | Posterior. Palpated in the inferior part of buttock when hip is flexed. | Commonly used as a contact point for sacroiliac adjustments. Tender to palpation with conditions such as apophyseal injuries, fractures, bursitis, and hamstring tendinopathies |
| ASIS | Anterior. Palpated by tracing iliac crest anterior and inferior; easier to palpate with the person seated when muscles attachments are relaxed. | Serves as the superior attachment site for the inguinal ligament. |
| Iliac tubercle | Anterior. Palpated 5–6 cm posterior to the ASIS. Represents the widest point of iliac crest. | Tenderness along the iliac tubercle and crest may occur with muscle strains of the muscles inserting onto this area and from contusions (“hip pointer”). |
| Pubic symphysis | Anterior. Palpated in midline, approximately a hand’s width inferior to umbilicus. | Tenderness may indicate osteitis pubis or pubic joint dysfunction (subluxation). Sacroiliac dysfunctions may also cause a tender pubic symphysis when palpated. |
| Pubic tubercle | Anterior. Approximately 2.5 cm anterior and lateral to pubic symphysis. | Important landmark when palpating the superficial inguinal ring (superolateral to pubic tubercle) in diagnosing inguinal hernias. Also serves as the inferior attachment site for the inguinal ligament. |
On palpating the paraspinal tissues and myofascial structures of the extremities, areas of focal irritation with discrete palpable thickening or muscle contraction are commonly felt. These taut and tender fibers, or trigger points, can be found in the long paraspinal muscles, shoulder girdle muscles (infraspinatus, supraspinatus, trapezius, rhomboid, and levator scapulae), the pelvis (iliopsoas, piriformis, quadratus, gluteal, and tensor fascia lata), and extremity muscles (extensor carpi radialis, vastus medialis, and soleus).2526 and 27
Myofascial trigger points can be identified by flat or pincer palpation.27 During flat palpation, the palpator’s fingertips move the patient’s subcutaneous tissue and skin across the taut muscle fibers. Pincer palpation is performed by grasping the muscle belly between the thumb and fingers while gently squeezing the tissues with a back-and-forth motion to locate taut bands. Fig. 10-2 demonstrates pincer palpation of the common wrist extensor muscle group.
 |
| Fig. 10-2 Pincer palpation of the patient’s common wrist extensor muscle group. |
Dynamic (Motion) Palpation
A widely held view on the primary effect of the adjustment is that it increases the range of motion of a joint. 13,15,17,28 The location and characteristics of the altered or restricted joint movement (fixation) must therefore be determined before an adjustment/manipulation can be performed. The primary technique for this evaluation is the dynamic (motion) assessment of the various joints of the spine, pelvis, and extremities. Specific techniques for palpating motion in joints can be divided into active, passive, and accessory movements (see Box 10-3).
Normally a joint will move through a certain range of active motion. The patient performs active movements while the examiner guides the patient through a particular motion. The patient’s voluntary muscle contraction causes the joint to move, and the clinician evaluates associated periarticular soft tissues for tension and resiliency. At the end of active motion, the clinician can passively push the bony lever (e.g., spinous process), thereby further assessing the quality of resistance, called end play or end feel. Springing of the joint and the determination of end play are an integral part of the examination preceding adjustment/manipulation (Fig. 10-3).
 |
| Fig. 10-3 Motion (dynamic) palpation assessment for right lateral flexion of the L2 vertebra (L2-L3 motor unit) in the seated position. |
Joint play assessment “is the qualitative evaluation of the joint’s resistance to movement when it is in a neutral position.”13 Joint play exists because the articular surfaces do not perfectly fit. The incongruent articular surfaces also prevent a fixed axis of rotation from occurring during joint motion. The joint capsules and ligaments remain somewhat lax to allow for rolling and gliding of the articular surfaces to accommodate for the changing axis of rotation around these irregular surfaces. The joint demonstrates joint play in the neutral position, when it is under the least amount of stress, with the joint capsule and ligaments in the position of greatest laxity (Fig. 10-4). An active range of motion produced by voluntary muscle contraction follows this joint play near the neutral position. The end point of the active range of motion is called the physiologic barrier7 (see Fig. 10-4).
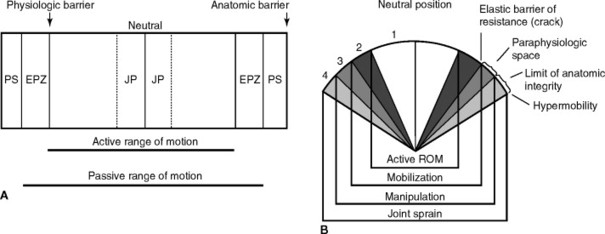 |
| Fig. 10-4 Two graphic representations of joint range of motion. A, Active and passive components of joint motion. PS, Paraphysiologic space; EPZ, end-play zone; JP, joint play. B, Sandoz chart. Four stages of range of movement in diarthrodial joints: 1, Active range of movement (motion produced by muscular action). 2, Passive range of movement (motion produced by traction or springing the joint/joint play, up to the elastic barrier or resistance); characterizes mobilization. 3, Paraphysiologic range of movement (motion beyond the elastic barrier of resistance up to the limit of anatomic integrity produced by adjustment/manipulation and accompanied by an audible release). 4, Pathologic movement (motion beyond the limit of normal anatomic integrity, which damages ligaments and capsule, resulting in joint hypermobility). Adjustment/manipulation that is too forceful may move the joint beyond the limit of anatomic integrity, creating or perpetuating joint instability. (From Gatterman MI: Foundations of chiropractic: subluxation, St Louis, 1995, Mosby.) |
If active range of motion is under the control of the musculature, passive movements are involuntary. Passive range of motion is defined as “movements carried through by the operator (clinician) without the conscious assistance or resistance of the patient.”13 The passive range of motion can be greater than the range of active joint movement (see Fig. 10-4). During active movements, the muscles move the joint to the physiologic barrier. Further movement past this barrier, into the end-play zone, is produced by additional overpressure performed by the examiner (see Figs. 10-3 and 10-4). The end-play zone, or increase in passive resistance, is thought to result from the elastic properties of the joint capsule and periarticular soft tissues. If the examiner were to release the pressure while stressing the tissues in the end-play zone, the joint would spring back to its physiologic barrier. Movement beyond the end-play zone is typically associated with an audible “cracking” noise followed by slight increase in the range of motion and has been referred to by Sandoz29 as the paraphysiologic space. Movement into the paraphysiologic space is within the normal boundaries of the joint and does not cause joint injury. At this point, another barrier is encountered, called the anatomic barrier. Further movement beyond this point will damage anatomic structures associated with the joint (see Fig. 10-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







