Anatomic classification of knee dislocation
KD-I
Single cruciate torn (ACL or PCL)
KD-II
Bicruciate tears (ACL and PCL)
KD-III
Bicruciate tears plus MCL or LCL/PLC
KD-IV
ACL, PCL, MCL, LCL/PLC tears
KD-V
All ligaments with an associated fracture
14.5 Initial Evaluation and Management
Identification of a knee dislocation is relatively easy if the knee remains dislocated at the time of presentation; however, a high index of suspicion is necessary in cases of dislocation followed by spontaneous reduction in the field. The clinician should be highly suspicious for knee dislocation if there is misalignment of the affected lower extremity, deformity of the knee, massive soft tissue swelling, or disproportionate pain (Fig. 14.1a). The absence of a joint effusion may be a misleading and false sense of comfort as high-energy dislocations can result in capsular damage, which will allow the knee effusion to diffuse into the surrounding soft tissue.


Fig. 14.1
(a) Anteroposterior and (b) lateral radiographs demonstrating an anterior knee dislocation. (c) Anteroposterior and (d) lateral radiographs demonstrating an adequate reduction of previous anterior knee dislocation
Patients presenting with knee trauma should be treated like any other traumatized patient, and the first step should always be implementation of the Advanced Trauma Life Support (ATLS) protocol [19]. Following ATLS protocol, and assuming the patient is without more pressing injuries, a dislocated knee should be reduced. In cases of high-energy knee dislocations, a portable “spot shot” radiograph of the knee should be taken prior to reduction to confirm the absence of major fractures. If fractures of the distal femur or proximal tibia are present, the clinician may opt to reduce the knee if the fractures appear relatively stable. In cases of low-energy trauma, such as knee dislocations sustained on the playing field, immediate reduction should be attempted prior to imaging studies. Post-reduction radiographs should always be obtained to confirm a concentric reduction of the tibiofemoral articulation (Fig. 14.1b). The knee should be initially inspected for any evidence of an open injury that would necessitate a formal irrigation and debridement in the operating room.
14.6 Vascular Evaluation and Management
Following confirmed reduction of the knee, a thorough vascular examination should be completed. The incidence of popliteal artery injury associated with knee dislocation has been reported to range from 4.8 to 65 %, with posterior knee dislocations having the highest rate of injury [8, 20, 21]. Vascular injuries are not solely associated with high-energy knee dislocations. Low-energy and spontaneous knee dislocations can cause vascular occlusion or intimal tearing [17, 22]. This examination should begin with inspection of the color, temperature, and capillary refill of the affected leg. Distal arterial flow in the dorsalis pedis, posterior tibial, and peroneal arteries should be interrogated first manually and secondarily with Doppler ultrasound if necessary. The clinician should be cognizant that a normal physical examination and palpable distal pulses do not exclude serious vascular injury, such as an intimal tear to the popliteal artery [23]. The ankle-brachial index (ABI) should be calculated using Doppler ultrasound and a blood pressure cuff if there is any concern for the vascular status. The ratio of systolic blood pressure in the affected ankle is compared to the unaffected upper arm. In a knee dislocation cohort, Mills reported 100 % sensitivity, specificity, and positive predictive value of a significant arterial injury requiring surgical attention if the ABI is below 0.90 [23]. Absent pulses or diminished ABIs are indications for involvement of a vascular surgeon. It is important to involve vascular surgery colleagues in an expeditious fashion, as warm ischemia time of greater than 6–8 h is associated with a higher rate of amputation [17, 24]. Additional studies or interventions that are frequently requested by a vascular surgeon include computed tomography angiogram (CTA) and formal angiography (Fig. 14.2). An abnormal CTA will necessitate a formal angiogram with either endovascular or open vascular intervention. At our institution a formal angiogram with or without intervention is accompanied by external fixation performed by an orthopedic surgeon to stabilize the knee, provide access for additional vascular procedures (the external fixation eliminates the need for a splint), and permit serial examinations of the affected limb postoperatively.
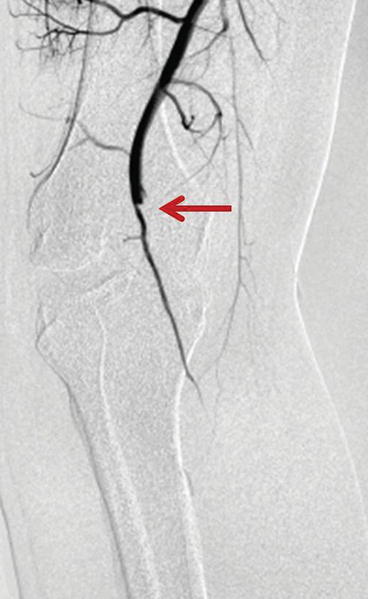
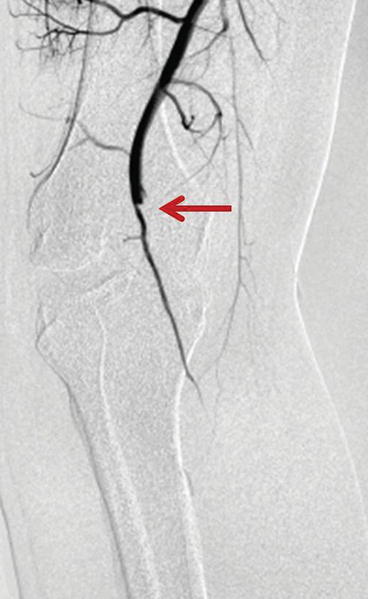
Fig. 14.2
Representative angiogram demonstrating lack of significant distal flow beyond the popliteal hiatus (popliteal artery) secondary to a knee dislocation. Arrow indicates significant obstruction
14.7 Neurologic Evaluation and Management
The incidence of nerve injury with acute knee dislocation is approximately 20 % [12, 25]. The most commonly injured nerve is the common peroneal nerve rather than the tibial nerve. The explanation for the higher incidence of peroneal nerve injury is its anatomic course adjacent to the proximal fibula, the decreased compliance compared to the tibial nerve, and the mechanism of knee dislocation. Lateral and posterolateral dislocations can significantly stretch the peroneal nerve. To identify these injuries, the clinician should perform an initial tactile exam of the patient’s sensation in all nerve distributions of the lower extremity. Graded motor strength with ankle dorsiflexion, ankle plantar flexion, ankle inversion, ankle eversion, and great toe dorsiflexion should be documented. There is no acute treatment for neurologic deficits following knee dislocation, and the overall prognosis for neurologic recovery remains low [26]. Chronic neurologic injuries such as foot drop may be treated with an ankle foot orthosis or a posterior tibial tendon transfer.
14.8 Ligamentous Evaluation
A thorough ligamentous examination should be performed on all patients with a suspected knee dislocation. The initial examination may be limited due to pain, hematoma, or associated injuries; however, gross laxity or instability should be documented to the best of the examiner’s abilities. It is important for the examiner to comment on the integrity of the main ligamentous stabilizers, including the ACL, PCL, MCL, LCL, and PLC. A brief review of the basic ligamentous examination is presented here.
The anterior drawer and Lachman examinations are performed to evaluate for laxity in the ACL, the latter of which is considered the more accurate maneuver [27]. Both examinations grade the magnitude of anterior-posterior (A-P) translation of the tibia in relation to the femur and the presence or absence of a firm endpoint of that motion. The presence of an ACL tear is typically apparent due to increased translation and a lack of a firm endpoint compared to the contralateral knee. A caveat for these maneuvers in the setting of an acute knee dislocation is that it may be difficult or impossible to flex the affected knee to 90° to perform the anterior drawer test secondary to pain, swelling, or fracture. In addition, both examination maneuvers take advantage of the normal anatomic resting position of the tibia in relation to the femur as the “starting point” for the examination of the magnitude of A-P translation. Typically the tibia lies anterior to the femur; however, if the PCL is disrupted, the tibial “starting point” may be translated posteriorly rendering the motion appreciated difficult to associate with ACL laxity rather than PCL laxity.
The third ACL examination maneuver is the pivot-shift test. This is the senior author’s preferred test for grading ACL laxity during an examination under anesthesia; however, it is difficult to perform on the awake patient due to the inability to control hip and leg position. In addition, the pivot-shift test requires an intact iliotibial band (ITB) for accurate results. In the acute knee dislocation, there may be tearing or disruption of the ITB. Lastly, pain, swelling, and fracture are additional reasons this examination maneuver may be difficult to perform in the setting of an acute knee dislocation.
The PCL may be evaluated by assessing the posterior sag and the posterior drawer. The posterior sag test, performed with the knee and hip flexed to 90°, evaluates the position of the proximal tibia in relation to the distal femoral condyles. In the presence of a PCL tear, the proximal tibia will sag (posterior translation) relative to the distal femoral condyles as compared to the contralateral side. The posterior drawer test is performed in 90° of flexion by applying a posteriorly directed force on the proximal tibia with the thumbs on the joint line to quantify the distance of posterior translation. A grade III injury (greater than 10 mm of posterior translation) indicates a combined PCL and PLC injury [28].
Collateral ligament testing is performed with valgus (MCL) and varus (LCL) force on the knee. The testing is performed with the knee in 30° of flexion to isolate the collateral ligaments. The test is then repeated in full knee extension. Laxity at both 30° of flexion and full extension suggests disruption of additional structures. On the lateral side, laxity with varus stress in full extension suggests injury to the cruciate ligaments and the PLC in addition to the LCL [29]. On the medial side, laxity with valgus stress in full extension suggests injury to the cruciate ligaments and medial capsule in addition to the MCL.
The PMC is examined with maneuvers that place external rotation stress with the knee in various degrees of flexion. These tests help define the degree of anteromedial rotatory instability. The most common test is performed with the knee in 30° of flexion. A valgus stress is imposed while the foot is externally rotated [30, 31]. If this test elicits an increase in anteromedial external rotation as compared to the contralateral side, then a PMC injury has been sustained. In addition, if a combined PMC-PCL injury has been sustained, the magnitude of posterior translation of the tibia in the posterior drawer test will be exaggerated or unchanged with internal rotation of the tibia. In a PCL-deficient knee with an intact PMC, the magnitude of posterior tibial translation with the tibia internally rotated during the posterior drawer will be diminished [32, 33].
The PLC can be directly assessed with the dial test. The structures interrogated with this test include the LCL, popliteus tendon, and popliteofibular ligament [34]. With the patient prone, the knees are flexed to 30° and a symmetric, external rotation force is placed on both feet. The thigh-foot angle is measured and the test is again repeated at 90° of knee flexion. A difference in thigh-foot angle of greater than 10° side to side is considered a positive test. An increased thigh-foot angle at 30° of knee flexion but not at 90° is consistent with an isolated PLC injury, while increased thigh-foot angle at both 30 and 90° of knee flexion is consistent with a combined PCL and PLC injury. An isolated increase in thigh-foot angle at 90° of knee flexion suggests an injury to the PCL. The examiner should also be aware that increased thigh-foot angle rotation at 30 and 90° of knee flexion may signify an injury to the anteromedial aspect of the knee rather than the PLC [35].
14.9 Diagnostic Imaging
Radiographs of the knee in two planes (anteroposterior and lateral) should be performed to characterize the direction of dislocation (Fig. 14.1a, b). Initial radiographs are also important to assess for associated fractures, either large osseous injuries to the tibial plateau and distal femur or subtle fractures such as a Segond fracture or PCL avulsion. As mentioned previously, in low-velocity knee dislocations (sports injuries), a reduction should be attempted prior to the initial radiographs and ideally on the field if trained medical personnel are present. This is due to the low likelihood of significant fractures. However, in high-velocity knee dislocations (e.g., automobile accidents), the likelihood of significant fractures is much greater and thus plain radiographs should be performed prior to a reduction attempt. In either scenario, post-reduction radiographs should be obtained to confirm a concentric reduction (Fig. 14.1c, d). If there is concern for a PCL injury, stress radiographs of the bilateral knees may be performed with the knees flexed 80° and weight applied to the anterior tibia [36]. Stress radiographs may be more appropriate in the preoperative planning phase rather than acutely following a knee dislocation.
Once the knee is stabilized and vascular injuries have been ruled out, a computed tomography (CT) scan may be appropriate if fractures are present, and a magnetic resonance image (MRI) should be obtained to assess the extent of the ligamentous injury (Fig. 14.3). The MRI will also assist with preoperative planning in the case of damage to the chondral surfaces, menisci, and capsule. Bone bruising is common following acute knee dislocation and present 75 % of the time [37], while 25 % of knee dislocations have concomitant meniscal injuries [37]. Furthermore, if fractures accompany the knee dislocation, the timing of MRI is crucial. Obtaining an MRI in the early phase of treatment, prior to open reduction and internal fixation of fractures, facilitates evaluation of ligamentous integrity without being obscured by the signal artifact of implanted hardware.
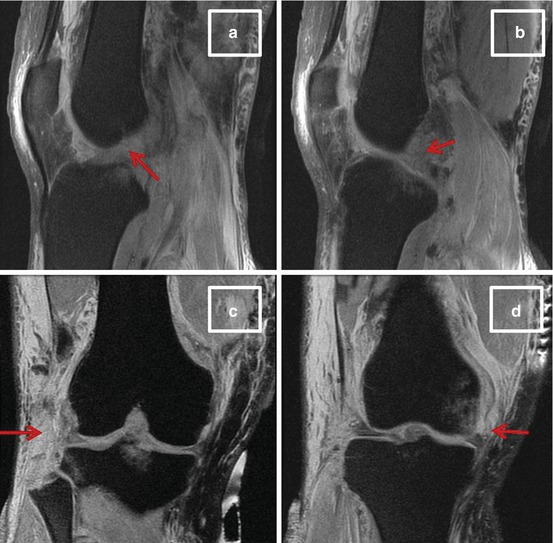
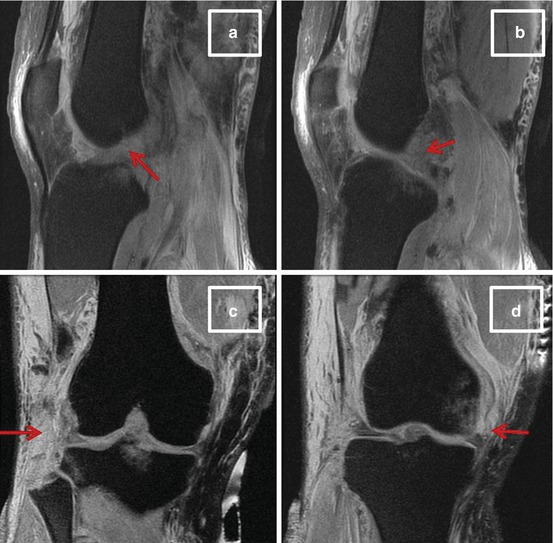
Fig. 14.3
(a) Sagittal magnetic resonance image (MRI) with arrow demonstrating complete disruption of the anterior cruciate ligament. (b) Sagittal MRI with arrow demonstrating complete disruption of the posterior cruciate ligament. (c) Coronal MRI with arrow demonstrating disruption of the lateral collateral ligament and posterolateral corner. (d) Coronal MRI with arrow demonstrating disruption of the medial collateral ligament
14.10 Initial Treatment
The initial care for a knee dislocation is dictated by a number of factors, including the open injury status, neurovascular status, fracture status, and ability to reduce the knee. If the dislocation is reduced, there is no fracture or open injury, and there is no concern for neurovascular compromise, then initial treatment may consist of a long-leg splint in 20° of knee flexion, lower extremity elevation, and serial neurovascular examinations. Twenty degrees of knee flexion is classically taught as the position for long-leg splinting; however, it is our experience that maintaining the knee in flexion for more than 3–5 days may compromise the ability to restore full extension long term. The treating surgeon should be cognizant of this during the initial management. If the knee dislocation is complicated by significant femoral condyle or tibial plateau fractures, an open injury, or a vascular injury or the knee is irreducible, then the complicating factor should be addressed in the operating room. Each of these complicating factors should also prompt the treating surgeon to consider concomitant application of external fixation rather than a splint at the conclusion of the operating room session. Stabilization of the dislocated knee with external fixation should also be considered in cases initially treated in a splint but with post-splinting films that demonstrate persistent tibiofemoral subluxation. Two important considerations when placing an external fixator following knee dislocation are that the hardware should be MRI compatible and the knee-spanning pins should be safely outside the knee joint and sufficiently away from future graft tunnel or fixation hardware sites. This “safe zone” for pin placement is roughly 10 cm proximal and distal to the knee joint line [38]. Lastly, if there is any clinical concern for compartment syndrome preoperatively or intraoperatively, the treating surgeon should have a low threshold for performing fasciotomies.
14.11 Definitive Treatment Considerations
Historically, the mainstay of knee dislocation definitive treatment was immobilization in plaster casts. However, as longitudinal clinical studies emerged, it became clear that patients sustaining knee dislocations and undergoing nonoperative treatment went on to develop persistent knee instability and had poor long-term functionality [39–42]. Recent studies suggest considerable benefit from surgical treatment [12, 21, 39, 41–45]. A recent systematic review comparing operative versus nonoperative treatments for multiligament knee injuries found significantly higher International Knee Documentation Committee (IKDC) scores, improved return-to-work rate, and higher rates of return to sport for patients in the cohort that underwent surgical treatment [44]. Dedmond and Almekinders [39] performed a meta-analysis of differences between operative and nonoperative treatment of acute knee dislocations. They evaluated 74 nonoperatively and 132 operatively treated knee dislocations and found significantly improved Lysholm scores in the surgically managed cohort as compared to the cohort treated nonoperatively [39]. Several other studies have corroborated these findings by comparing return to sport following acute knee dislocation and demonstrated higher success rates in those undergoing surgical reconstruction [45, 46].
14.12 Nonoperative Treatment
Despite the emerging clinical evidence that favors operative rather than nonoperative definitive care, there are some instances in which the treating clinician should opt for nonoperative management. Polytraumatized or significantly injured patients with multiorgan system injuries should not be indicated for surgery until they are able to participate in postoperative rehabilitation. Patients with open injuries and inadequate soft tissue coverage in which there are concerns for wound healing should not be indicated for surgical reconstruction. The low functional demand and morbidly obese patient populations will likely have better outcomes with nonoperative rather than operative treatment. Lastly, patients who wish to pursue nonsurgical treatment should be counseled on the pros and cons of both surgical and nonsurgical care and ultimately have their wishes granted if they choose nonoperative management.
14.13 Surgical Treatment
The objective of definitive surgical management following an acute knee dislocation is to provide a stable joint and ideally return the patient to his or her preoperative activity level. While the objective is clearly defined, there is considerable debate concerning several surgical factors, including timing of surgery, surgical approach, ligamentous repair versus reconstruction, and technique of reconstruction.
14.13.1 Timing of Surgery
The timing of surgery can be broadly classified as early (within the first 2–3 weeks following injury) or delayed (greater than 3 weeks from the time of injury). A third broad classification is a staged approach in which the medial and lateral structures are repaired or reconstructed with or without PCL reconstruction in the early window followed by delayed ACL reconstruction if deemed necessary. Although not universally implemented, the staged approach is still in practice and has been advocated by a number of authors [11, 47]. Currently, most knee surgeons advocate early surgical intervention, and this approach is widely supported by the literature [41, 44, 48, 49]. Harner reported on the subjective and objective outcomes of 31 knee dislocations, 19 of which underwent acute reconstructions [41]. Their cohort of acutely treated patients reported higher subjective scores and had increased stability compared to the delayed cohort. Conversely, authors have also reported favorable outcomes utilizing a delayed approach to ligamentous reconstruction [50–54]. Mook and colleagues performed a systematic review of multiligamentous knee injuries treated with early, late, or staged reconstructions [50]. Their analysis suggested that delayed reconstruction had the advantage of lower rates of postoperative stiffness while performing comparable to early and staged procedures in terms of knee stability. Ultimately, the decision to proceed with acute or delayed reconstruction should be based on patient-specific factors and the surgeon’s comfort level with the various surgical techniques. Lastly, regardless of the decision to operate in the early or delayed postoperative window, the surgeon should be aware that arthroscopic reconstruction in the presence of a disrupted capsule may cause fluid extravasation and result in compartment syndrome. Although this concern is greater in the immediate post-injury phase, all surgeons should be aware of this potential complication and allow 1–2 weeks of post-injury healing prior to any arthroscopic procedure.
14.13.2 Surgical Technique
A wide variety of surgical techniques have been described for the treatment of acute knee dislocations. Successful surgical intervention first requires the treating surgeon to accurately and completely identify all injuries, including those to ligaments, bone, menisci, cartilage, and adjacent soft tissues. Second, regardless of technique, the primary ligamentous restraints must be repaired or reconstructed in an anatomic and isometric fashion. A detailed discussion of all the potential techniques for the surgical care of acute knee dislocations is outside the scope of this chapter; however, a brief description of our preferred ligament reconstruction surgical techniques will follow.
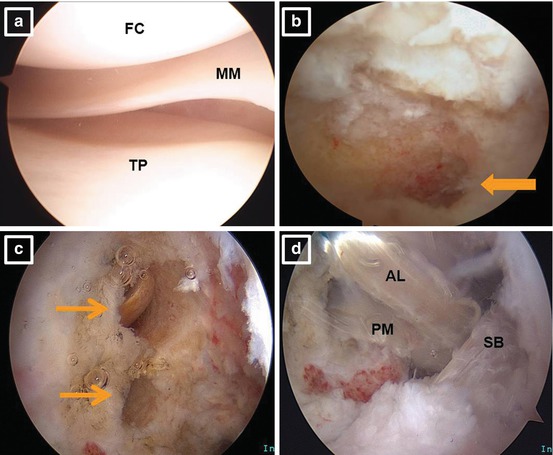
Once the patient is in the operating room, the first step to a successful knee reconstruction is an examination under anesthesia (EUA). A thorough EUA takes advantage of full muscle relaxation and allows the surgeon to completely delineate the extent of the ligamentous injury. The previously described ligamentous examination is repeated, including Lachman, pivot-shift, anterior and posterior drawers, varus and valgus stress testing, and medial and lateral rotational testing. If there is any uncertainty regarding the extent of ligamentous injury after the MRI and EUA, a diagnostic arthroscopy can be performed prior to autologous graft harvest or open surgical treatment of collateral, PLC, or PMC structures. An initial arthroscopy is also beneficial for evaluation of the menisci, chondral surfaces, and joint capsule (Fig. 14.4a).