A 1: Simple (two–fragment) pertrochanteric fractures
A1.1 Fractures following the intertrochanteric line
A1.2 Fractures through the greater trochanter
A1.3 Fractures below the lesser trochanter
A 2: Multifragmentary pertrochanteric fractures
A2.1 With one intermediate fragment
A2.2 With two intermediate fragments
A2.3 With more than two intermediate fragments
A 3: Intertrochanteric fractures
A3.1 Simple, oblique
A3.2 Simple, transverse
A3.3 With a medial fragment
Osteoporosis must be included in the classification scheme because it influences the outcome of fractures near the hip joint, especially in pertrochanteric fractures because the anchorage of specific implants depends on it. The osteoporosis classification of Singh [64], in the context of fractures near the hip joint, is based on the permeability of the trajectories in the femoral neck and femoral head as well as on their quality in conventional X-ray images. It is divided into six grades (I to VI). Grade VI represents a normal-appearing hip joint with trajectories clearly seen on the X-ray, whereas, in grade I, trajectories can only be detected in the caudal areas of the femoral neck and head.
Generally, the failure rate depends on three important factors:
Degree of instability
Degree of osteoporosis
Surgical skills
While an implant failure rate of 1–9 % is to be expected in stable fractures, it increases to 2–26 % in unstable ones [14, 18, 35, 38, 39, 42, 70, 76]. Therefore, an adequate choice of the implant and a high quality of operative care are crucial.
Implants for osteosynthesis fail more often in the lower Singh grades (Singh I, II, III) than in the higher grades (Singh IV, V, VI). Therefore, the probability of osteosynthesis failure is very high in A2 or A3 fractures that are classified by Singh grade I to III. By correct reduction and correct implant positioning, the failure rate can at least be reduced to 3.6 %.
For two reasons the osteoporosis classification according to Singh cannot be recommended without reservations:
A high interobserver variability is evident.
It does not correlate with the qualitative evaluation of osteoporosis using the standard method of dual-energy X-ray (DXA).
20.5 Therapy
Undoubtedly, a lack of anatomical reduction results in a fracture healing in a displaced position. This is and will always be the main reason for persistent functional limitations, which are disturbing for the patient and therefore reduce quality of life [27].
Irrespective of the choice of therapy to treat the fracture itself, a routinely prescribed thrombosis prophylaxis is necessary because of the high incidence of thrombosis, varying from no symptoms at all to severe complications like pulmonary embolism. In cases that include embolism or thrombosis in the anamnesis, a special prophylaxis is indicated [65]. Furthermore, it is advised that patients older than 70 years of age be treated perioperatively, and if necessary also postoperatively, with intravenous (IV) antibiotics to prevent or combat latent or manifest infections [7].
20.5.1 Conservative Therapy
Unstable pertrochanteric fractures can be reduced sufficiently using skeletal traction. However, the necessary 12 weeks of bed rest that follow this therapy are dangerous and inconvenient for the patient and therefore can rarely be recommended. (For traction treatment, see also Chaps. 2 and 4). Stable fractures can be reduced by using a “foam splint.” Premature end of the traction treatment (earlier than 12 weeks for adults) and further treatment with a pelvis-leg cast may lead to a secondary axis deviation in a varus position, despite good callus bridges [9, 36, 55].
20.5.2 Operative Therapy
This is the therapy of choice for trochanteric hip fractures. Basically, three different treatment options can be recommended (Figs. 20.1 and 20.2):
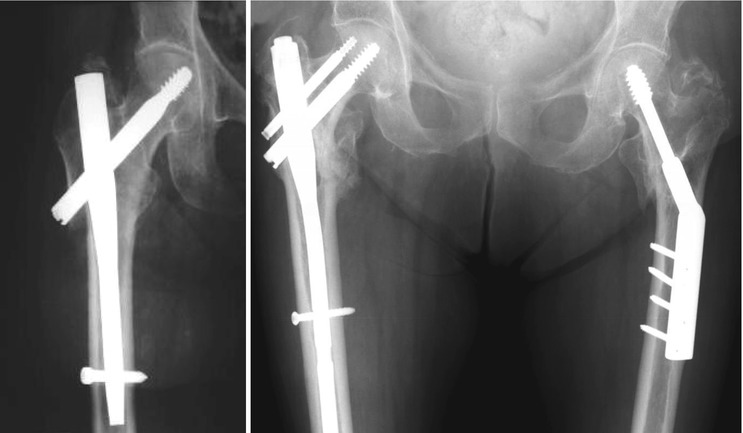
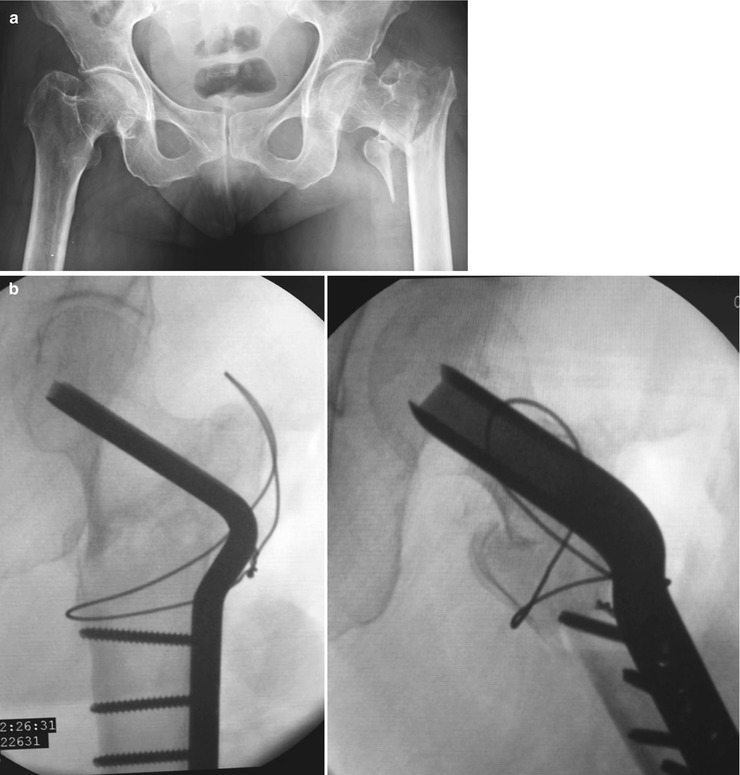
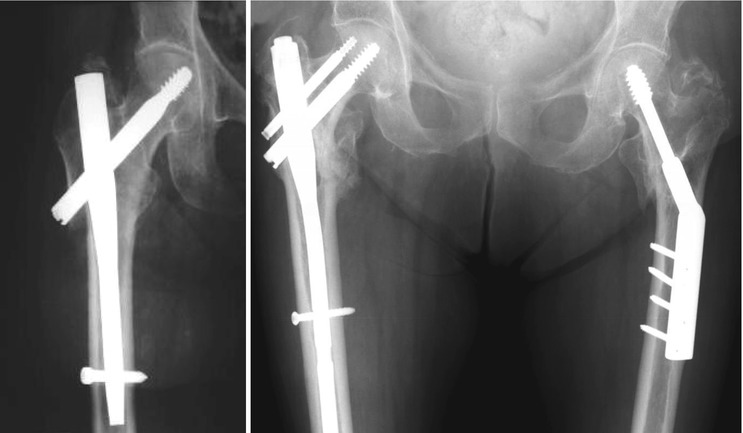
Fig. 20.1
Gamma-nail, PFN, and DHS
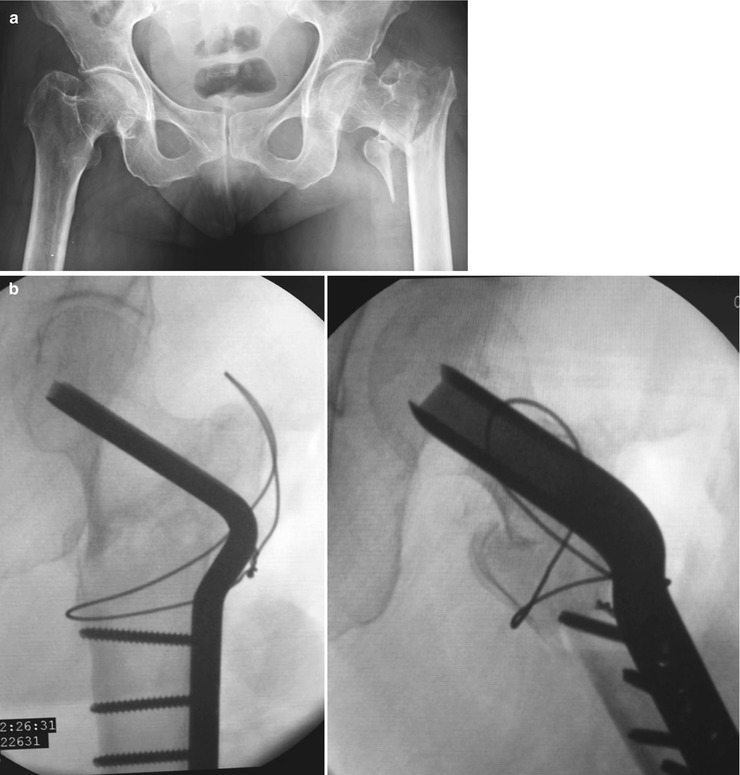
Fig. 20.2
(a) Highly unstable trochanteric fracture. (b) Fixation with double-angled blade plate and tension band wire, valgisation, and medialization
Dynamic sliding systems or compression screw systems such as Dynamic Hip Screw (DHS) [34, 35, 69], with or without adjustable, attachable locking trochanter stabilization plate (LTSP) [14]; the Medoff [45] plate; or an integrated trochanteric reinforcement in the plate, such as the Gotfried [26] trochanter plate
Intramedullary systems on the basis of the Y-nails developed by Küntscher [40], such as trochanter nails, Gamma nails [24], Proximal Femoral Nail – Alpha (PFNA) [21, 23, 62], sliding nails [22], Fi-nails, and many others
Angled and double-angled blade plates are versatile and inexpensive implants that, in experienced hands, can solve many problems in unstable trochanteric fractures as well as in salvage procedures (Fig. 20.3) [77]. However, techniques such as the Dimon-Hughston procedure [16] or valgisation and medialization have to provide an intrinsic stability of the construct (Figs. 20.4 and 20.5).

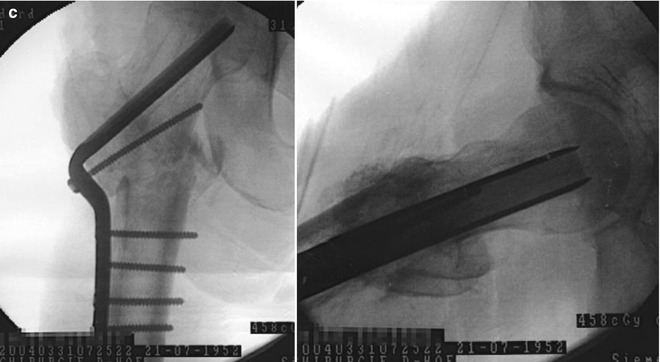
Fig. 20.3
(a) Failed fixation of a trochanteric fracture with DHS. (b) Salvage procedure with PFN failed. (c) Definitive salvage procedure with double-angled blade and intertrochanteric valgisation osteotomy and medialization
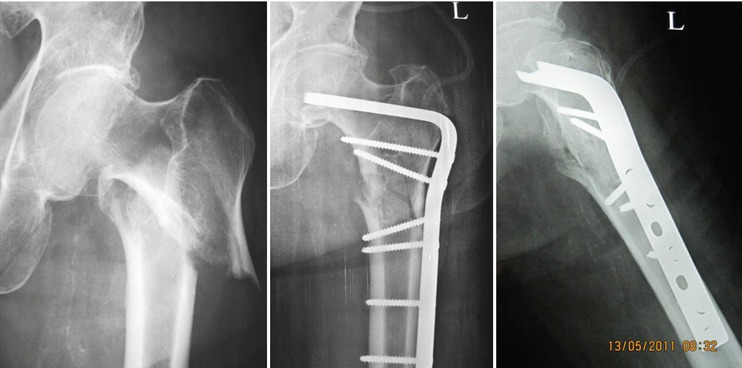
Fig. 20.4
Intertrochanteric fracture with “reversed obliquity,” fixation with a condylar plate

Fig. 20.5
Intertrochanteric fracture with “reversed obliquity,” Dimon-Hughston procedure, fixation with double-angled blade plate
New concepts such as percutaneus locking plates and the use of an external fixator on a routine basis are not approved yet [53, 64, 71, 72]. According to biomechanical examinations, the weight-bearing capacity of intramedullary nail systems is generally higher than those of dynamic slip systems [3, 4, 22, 34, 59]. This fact, as well as the instability of the fracture, should be considered before choosing the implant. Endoprosthetic care is only used in rare, particular cases.
20.5.2.1 Reduction
Fracture reduction is always the first step in the algorithm of operative treatment for pertrochanteric hip fractures.
Closed Reduction
Closed reduction on the traction table (fracture table) is routinely the method of choice to treat this kind of fracture. In order to guarantee sufficient leg manipulation, it is advised to connect the traction table with a high lace-up shoe. After the leg has been positioned in the shoe and connected with the plate of the traction table, reduction is facilitated and optimal manipulation can be achieved. Longitudinal traction and internal rotation are usually needed to reduce the fracture. By locking the hinges of the table, reliable retention can be guaranteed for the duration of the surgery. Whereas extramedullary osteosynthesis allows an abduction of the injured leg, intramedullary fixation should be carried out with the leg in slight adduction.
The use of two image intensifiers (a.p. and axial) should be a routine set-up (if there is enough space in the operating room) because it simultaneously enables sufficient intraoperative control of the fracture fragments and the reduction in two planes.
Open Reduction
Dissecting a pertrochanteric fracture in combination with open reduction is usually performed when closed reduction is not successful and further manipulation of the displaced fracture fragments is necessary. Nevertheless, open reduction causes vast damage to the local tissue structures in a pertrochanteric fracture and can result in extensive blood loss with persistent limited manipulation capacity of the fracture fragments. The combination of open reduction and manipulation on the traction table is a sometimes underestimated tool that can facilitate this difficult surgical step.
20.5.2.2 Stabilization
If the fracture reduction has been successful, the surgical stabilization should be performed next. The choice of the implant generally depends on the required stability and on the fracture configuration. The decision making should include the following points:
Is osteoporosis evident? If yes, to what degree?
Can the fracture be classified as stable? If it is unstable, what kind of instability exists?
What is the patient’s general condition (biological age, general state of health, concomitant illnesses, American Society of Anesthesiologists Score (ASA) score)? [1].
Stabilization has the following aims:
Fixation of the fracture in an anatomical, functionally optimal position
Postoperative full weight bearing that is free of pain should be achieved to prevent further expected complications
Extramedullary, Juxtacortical Osteosynthesis
The key point of the extramedullary plate osteosynthesis is the positioning of the lag screw in the head-neck fragment of the femur: in the anterior-posterior view it should be a little caudal to the femoral head center; in axial view, it should be posterior to the midline and parallel to the femoral neck. After placement of the lag screw, the plate slides onto the bone through the screw and is fixed to the shaft with two to four screws. The system enables the lag screw to glide in the conjunction of the plate. As a consequence, the risk of secondary head perforation of the screw centrally can be reduced [6, 13, 32, 34, 47, 48, 52], which is a common complication in side plates fixed to a head screw or nail system (Jewett plate, three flanged nails with side plates, etc.) [33, 76].
Advantages and Disadvantages
Sliding screws, compression screws, and plate systems are easy to handle after correct application. Apart from the appropriate height of the skin incision and of the soft tissue incision, the positioning of the guide wire is an important key step. The further steps are described in detail in the chapter [19].
Concerning pertrochanteric fractures, the surgeon should be aware that the head-neck fragment might rotate during thread cutting for the lag screw. If this happens, the fragment must be secured with a second K-wire, which is positioned parallel to the guide wire. In all systems in which the head-neck fragment is secured with only one screw, it is possible that the fragment rotates secondarily during aftercare, in the case that the fracture fragments do not interlock. The rotation mechanism can be prevented by using a spiral blade instead of the lag screw. In fracture forms with a shortening tendency it is also possible to medialize the shaft with a lateralization of the head-neck fragment compressed with the trochanter region, seen especially in reversed type fractures [17, 41]. Apart from shortening of the femoral neck length and from a shift of the mechanical axis of the leg, this procedure can cause clinically relevant leg shortening.
To prevent this phenomenon, the locking trochanter stabilization plate (LTSP) [14] was developed as a supplement to the DHS. It can be connected to the regular DHS plate. It offers lateral support. Furthermore, the greater trochanter is stabilized, which secures the function of the m. gluteus medius, reduces the extent of the fracture impaction in the lateral direction, and counteracts the medialization of the shaft as well as a possible secondary varus malposition resulting in leg shortening.
The Gotfried trochanter plate [26, 32] is constructed in a way that the lateral support is permanently included in the side plate and that two dynamic screws are placed in the head-neck fragment.
To prevent a secondary axis deviation and cut-outs, it is recommended to fill the lag screw as well as the metaphysical defects with bone cement. However, using bone cement on a routine basis is contraindicated as it causes local heat necrosis. Furthermore, interposition of bone cement in the fracture surfaces can lead to a delay or prevention of bone healing and it can disable further necessary, corrective procedures [2, 15, 29, 30, 42, 43] (Fig. 20.3a–c).
Complications
Type of complication | % |
|---|---|
Intraoperative femur shaft fracture | 1.0 |
Wound healing problems | 1.0 |
Infection | 1.0 |
Cut out | 5–6 |
Pseudoarthrosis (nonunion) | 12.0 |
Mortality within 12 months | 13.0 |
Intramedullary Osteosynthesis
The load carrier is shifted from juxtacortical lateral to the medullary cavity. The nail has three notches. One notch is situated cranial in a diagonal direction; it runs from lateral distal to proximal medial, corresponding to the CCD angle, and it is used to insert the lag screw, spiral blade, or T-profile anchorage. Two distal notches enable the placement of interlocking screws that secure leg length and guarantee rotational stability of the implant in the femur. The components of the implant are inserted by precisely working target devices only using small stab incisions. While the load carrier of the head-neck fragment is dynamically mounted to the nail in order to allow compression onto the fracture, the nail itself can be locked distally using bicortical screws dynamically (with a sliding path of approximately 10 mm) or statically, with no play of the nail in the medullary cavity at all.
Experimental studies revealed that the load-bearing capacity is higher using intramedullary implants compared with extramedullary osteosynthesis, because the lever arm calculated from the tip of the implant for the head-neck fragment to the nail versus to the plate is shorter in the former. Furthermore, the load transfer to the femur shaft is distributed across a longer distance in a dynamic way. The compressing mechanism can occur in two directions simultaneously [6, 8, 10, 22, 24, 37, 44, 46, 50, 51, 56, 58, 61, 67, 74, 75]. Secondary dynamization, that is, removal of the distal locking screw, is hardly ever necessary and is only indicated if delayed union is suspected after observing a series of follow-up X-rays.
Workflow of the surgery:
Positioning of the anesthetized patient on the traction table. Fixing both legs and bracing the pubic bone on the fracture side on a pillar padded with cotton wool
Reduction of the fracture using longitudinal traction and rotation under image intensifiers control (a.p. and axial) in slight adduction of max.10°
Determining the CCD angle and choosing the appropriate implant (from 120° to 140° in 5° intervals)
Disinfection and sterile draping of the surgical field
Skin incision a few centimeters cranial of the palpable tip of the trochanter. Splitting of the fasciae and musculature on the tip of the trochanter slightly oblique down to the medial side
Opening the medullary cavity with a pointed awl and inserting the guide wire into the medullary cavity
If necessary, enlarging the trochanteric region and medullary cavity by hand using a cannulated drill, which corresponds to the external dimension of the nail: largest diameter for the trochanteric region, smaller ones corresponding to the peripheral nail diameter for the medullary cavity.
Manual insertion of the nail connected to the target device into the medullary cavity, using the inserted guide wire as guidance. It is possible to equip the target device with an aligner unit in order to facilitate the optimal positioning of the guide wire for the head-neck implant and for adjustment of the nail in both planes using image intensifiers.
Second skin incision according to the target device, splitting of the fasciae and pushing away the musculature with a protective sleeve until the target device has contact to the bone
Removal of the guide wire
Opening of the lateral corticalis with the spiral drill. As a consequence, the guide wire for the head implant does not bend under manual pressure when the corticalis is opened, causing a diversion when the notch of the nail is passed. If this is not considered, the reamer in the next step collides with the wall of the nail, which can cause a vulnerable point for nail breakage.
According to the designated length of the head screw, spiral blade, or T-profile anchorage, the implant is inserted according to the instruction manuals and, if necessary, secured by a set screw for the defined glide path [20, 39].
Finally, distal locking is carried out, usually with a screw. The protective sleeve is used to ensure good bone contact without interposition of soft tissue. Drilling through both cortices, the necessary length of the screw is measured and the screw is inserted manually with the help of a screwdriver. The usage of a mallet is strictly forbidden.
For combined fractures such as trochanteric fractures with a femoral shaft fracture, the use of a long Gamma nail is recommended [17].
Advantages and Disadvantages
In all its varieties, the intramedullary osteosynthesis is a closed, minimally invasive method. The alignment of the fracture fragments must be correct in all planes prior to stabilization. If closed reduction combined with percutaneous simple reposition aids is insufficient to achieve an acceptable result, open reduction should be performed to reach this goal as well as to restore length proportions [54].
Although it seems to be a technically simple surgical procedure, the surgeon has to be aware of possible sources of error, which come to be known with experience. The surgical steps are as follows:
Reduction should be performed prior to the actual osteosynthesis.
It is necessary to widen the medullary cavity as needed.
The nail must be inserted manually. If it cannot be inserted without extreme force, it should be removed and the medullary cavity should be widened a little bit more. Under no circumstances should the nail be hammered into the medullary cavity. As a consequence, a fracture of the femoral shaft would occur on a regular basis.
A backlash between the target device and the nail results in a loss of precision during the drilling procedure. This can cause mis-drilling. The connection between the two elements should be checked regularly during the surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








