Elbow
The elbow’s primary role in the upper limb complex is to help an individual position his or her hand in the appropriate location to perform its function. Once the shoulder has positioned the hand in a gross fashion, the elbow allows for adjustments in height and length of the limb, allowing one to position the hand correctly. In addition, the forearm rotates, in part at the elbow, to place the hand in the most effective position to perform its function.
Applied Anatomy
The elbow consists of a complex set of joints that require careful assessment for proper treatment. The treatment must be geared to the pathology of the condition, because the joint responds poorly to trauma, harsh treatment, or incorrect treatment.
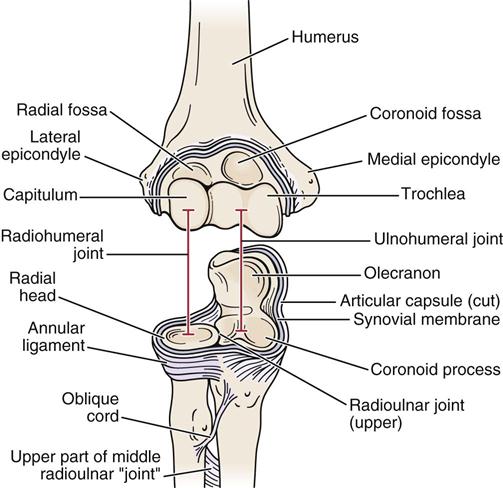
Because they are closely related, the joints of the elbow complex make up a compound synovial joint with injury to any one part affecting the other components as well (Figure 6-1). In addition, the ulnar and humeral articulations “fit” together rather intimately, which does not allow much “give” as compensation when an injury occurs. Thus, this joint often does not respond well to trauma. The elbow articulations are made up of the ulnohumeral joint and the radiohumeral joint. In addition, the complexity and intricate relation of the elbow articulations are further increased by the superior radioulnar joint, which has continuity with the elbow articulations. These three joints make up the cubital articulations. The capsule and joint cavity are continuous for all three joints. The combination of these joints allows 2° of freedom at the elbow. The trochlear joint allows 1° of freedom (flexion-extension), and the radiohumeral and superior radioulnar joints allow the other degree of freedom (rotation).
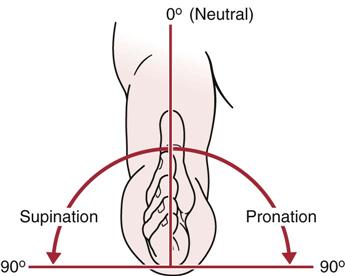
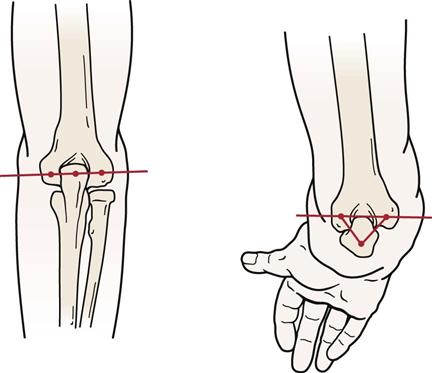
The ulnohumeral or trochlear joint (see Figure 6-1) is found between the trochlea of the humerus and the trochlear notch of the ulna and is classified as a uniaxial hinge joint. The bones of this joint are shaped so that the axis of movement is not horizontal but instead passes downward and medially, going through an arc of movement. This position leads to the carrying angle at the elbow (Figure 6-2). The resting position of this joint is with the elbow flexed to 70° and the forearm supinated 10°. The neutral position (0°) is midway between supination and pronation in the thumb-up position (Figure 6-3). The capsular pattern is flexion more limited than extension, and the close packed position is extension with the forearm in supination. On full extension, the medial part of the olecranon process is not in contact with the trochlea; on full flexion, the lateral part of the olecranon process is not in contact with the trochlea. This change allows the side-to-side joint play movement necessary for supination and pronation. A small amount of rotation occurs at this joint. In early flexion, 5° of medial rotation occurs; in late flexion, 5° of lateral rotation occurs.

The radiohumeral joint is a uniaxial hinge joint between the capitulum of the humerus and the head of the radius (see Figure 6-1). The resting position is with the elbow fully extended and the forearm fully supinated. The close packed position of the joint is with the elbow flexed to 90° and the forearm supinated 5°. As with the trochlear joint, the capsular pattern is flexion more limited than extension.
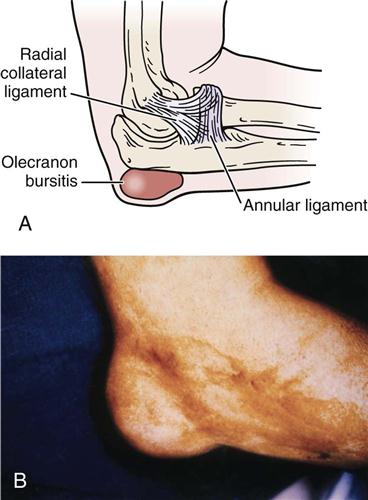
The ulnohumeral and radiohumeral joints are supported medially by the ulnar collateral ligament, a fan-shaped structure, and laterally by the radial collateral ligament, a cordlike structure (Figure 6-4).1 These ligaments, along with the ulnohumeral articulation, are the primary restraints to instability in the elbow.2 The lateral (radial) collateral ligament is the primary restraint to posterolateral instability (most common instability), whereas the medial (ulnar) collateral ligament is the primary restraint to valgus instability.2 The ulnar collateral ligament has three parts, which along with the flexor carpi ulnaris muscle form the cubital tunnel through which passes the ulnar nerve (see Figure 6-4). Any injury or blow to the area or injury that increases the carrying angle puts an abnormal stress on the nerve as it passes through the tunnel. This can lead to problems such as tardy ulnar palsy, the symptoms of which can occur many years after the original injury and may be caused by the “double crush” phenomena of a cubital tunnel problem combined with a cervical spine problem.
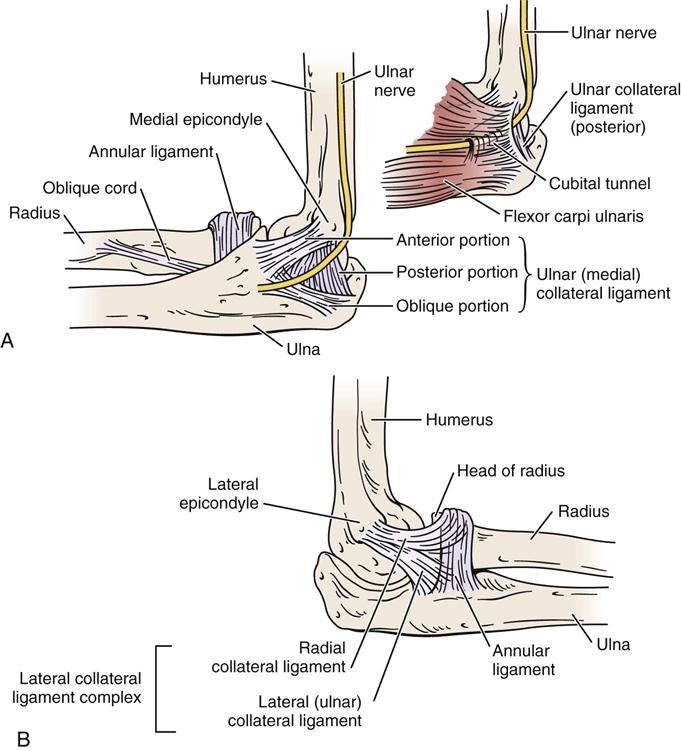
A, Ligaments on medial side of elbow. Note the passage of the ulnar nerve through the cubital tunnel. B, Ligaments on the lateral side of elbow.
The superior radioulnar joint is a uniaxial pivot joint. The head of the radius is held in proper relation to the ulna and humerus by the annular ligament (see Figures 6-1 and 6-4), which makes up four fifths of the joint.3 The resting position of this joint is supination of 35° and elbow flexion of 70°. The close packed position is supination of 5°. The capsular pattern of this joint is equal limitation of supination and pronation.
The three elbow articulations are innervated by branches from the musculocutaneous, median, ulnar, and radial nerves. The middle radioulnar articulation is not a true joint but is made up of the radius and ulna and the interosseous membrane between the two bones. The interosseous membrane is tense only midway between supination and pronation (neutral position). Although this “joint” is not part of the elbow joint complex, it is affected by injury to the elbow joints; conversely, injury to this area can affect the mechanics of the elbow articulations. The interosseous membrane prevents proximal displacement of the radius on the ulna. The displacement is most likely to occur with pushing movements. The oblique cord connects the radius and ulna, running from the lateral side of the ulnar tuberosity to the radius slightly below the radial tuberosity. Its fibers run at right angles to those of the interosseous membrane (see Figure 6-1). The cord assists in preventing displacement of the radius on the ulna, especially during movements involving pulling.
Patient History
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. How old is the patient? What is the patient’s occupation? Tennis elbow (lateral epicondylitis) problems usually occur in persons 35 years of age or older and in those who use a great deal of wrist flexion and extension in their occupations or activities, requiring wrist stabilization in slight extension (functional position). If the patient is a child who complains of pain in the elbow and lacks supination on examination, the examiner could suspect a dislocation of the head of the radius. This type of injury is often seen in young children. A parent may give the child a sharp “come-along” tug on the arm, or the child may trip while the parent is holding the hand, dislocating the head of the radius. Between the ages of 15 and 20, osteochondritis dissecans may be found.4
2. What was the mechanism of injury? Did the patient experience a fall on out-stretched hand (FOOSH) injury or on the tip of the elbow? Catching oneself from falling (Figure 6-5) or repetitive stress in sports (e.g., throwing) can create a severe valgus force to the elbow causing a medial side traction injury (e.g., sprain of the medial collateral ligament) and a lateral side compression injury. This can lead to injury at the radiohumeral joint, abnormal stress at the medial epicondyle (“little leaguer’s elbow”—if from repetitive stress from throwing), and osteochondral damage either on the olecranon process or olecranon fossa. Were any repetitive activities involved? Does the patient’s job involve any repetitive activities? Did the patient perform any unusual activities in the previous week? Did the patient feel a “pop” when throwing or doing other activity? If the pop was followed by pain and swelling on the medial side of the elbow, it may indicate an ulnar collateral ligament sprain.5 A centralized “pop” and weakness of elbow flexion may be the result of a distal biceps rupture. Such questions help determine the structure injured and the degree of injury.
5. Are there any activities that increase or decrease the pain? Does pulling (traction), twisting (torque), or pushing (compression) alter the pain? For example, writing, twisting motions of the arm (e.g., turning key, opening door), ironing, gripping, carrying, and leaning on forearm all stress the elbow.6 Such questions may indicate the tissues being stressed or the tissues injured.
7. Is there any indication of deformity, bruising (Figure 6-6), wasting, or muscle spasm?
11. Does the patient complain of any abnormal nerve distribution pain? The examiner should note the presence and location of any tingling or numbness for reference when checking dermatomes and peripheral nerve distribution later in the examination. Snapping on the medial side may indicate recurrent dislocation of the ulnar nerve or the medial head of the triceps dislocating over the medial epicondyle.4
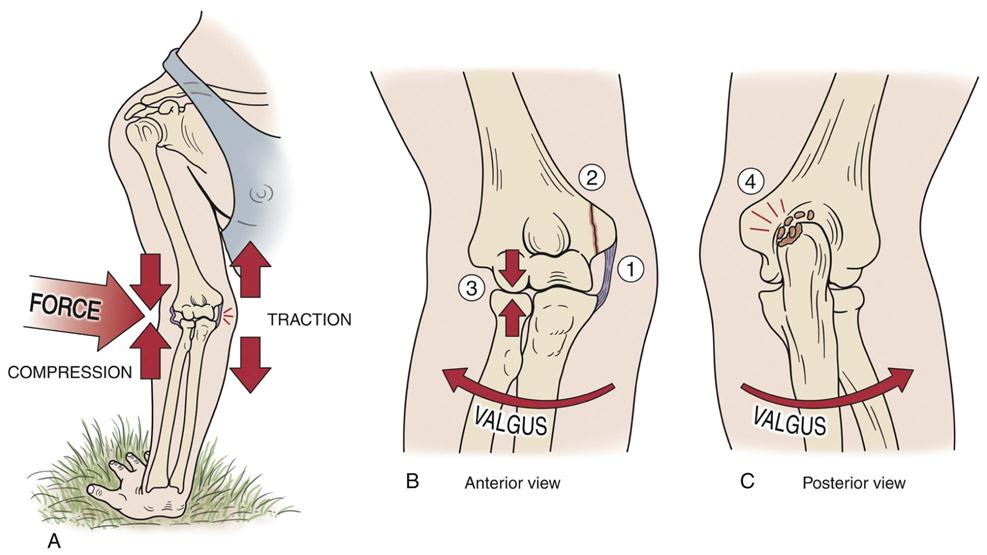
(A) Mechanism of injury. (B) Anterior view. (C) Posterior view. Injury may lead to 1) stretching of medial collateral ligament, 2) stress on epicondylar growth plate (pitcher’s or little leaguer’s elbow), 3) compression at radiohumeral joint, or 4) compression of the olecranon in the fossa, which may lead to osteophyte and loose body formation.
Observation
The patient must be suitably undressed so that both arms are exposed to allow the examiner to compare the two sides. If the history indicates an insidious onset of elbow problems, the examiner should take the time to observe full body posture, especially the neck and shoulder areas, for possible referral of symptoms.
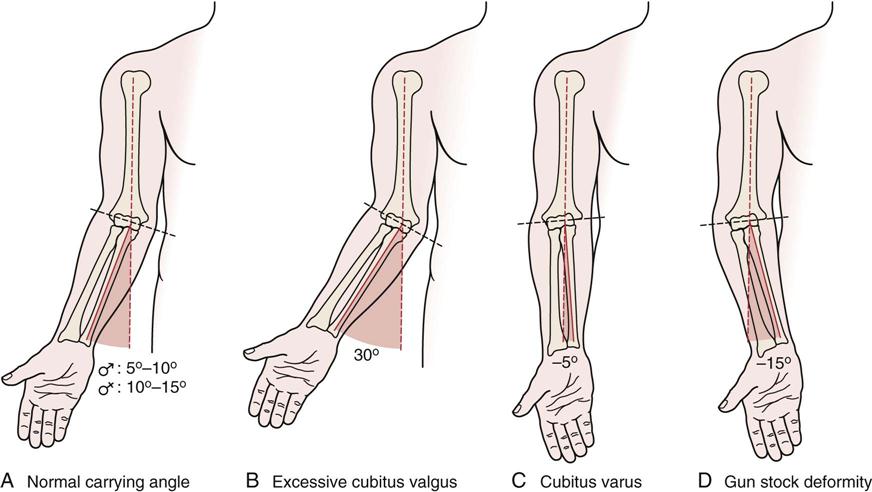
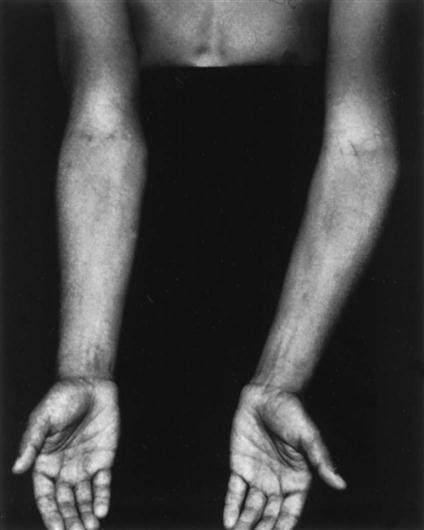
The examiner first places the patient’s arm in the anatomical position to determine whether there is a normal carrying angle7 (see Figure 6-2). It is the angle formed by the long axis of the humerus and the long axis of the ulna and is most evident when the elbow is straight and the forearm is fully supinated (Figure 6-7). In the adult, this would be a slight valgus deviation between the humerus and the ulna when the forearm is supinated and the elbow is extended. In males, the normal carrying angle is 5° to 10°; in females, it is 10° to 15°. If the carrying angle is more than 15°, it is called cubitus valgus; if it is less than 5° to 10°, it is called cubitus varus (Figure 6-8). Because of the shape of the humeral condyles that articulate with the radius and ulna, the carrying angle changes linearly depending on the degree of extension or flexion. Cubitus valgus is greatest in extension. The angle decreases as the elbow flexes, reaching varus in full flexion.8 If there has been a fracture or epiphyseal injury to the distal humerus and a cubitus varus results, a gun stock deformity may occur in full extension (Figure 6-9, see Figure 6-8).

The carrying angle may be determined by noting the angle of intersection between a line connecting midpoints in the distal humerus and a line connecting midpoints in the proximal ulna.
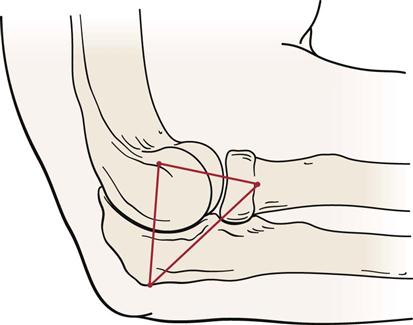
If swelling exists, all three joints of the elbow complex are affected because they have a common capsule. Joint swelling is often most evident in the triangular space between the radial head, tip of olecranon, and lateral epicondyle (Figure 6-10). Swelling resulting from olecranon bursitis (student’s elbow) is more discrete, being more sharply demarcated as a “goose egg” over the olecranon process (Figure 6-11). With swelling, the joint would be held in its resting position, with the elbow held in approximately 70° of flexion, because it is in the resting position that the joint has maximum volume.
The examiner should look for normal bony and soft-tissue contours anteriorly and posteriorly. Often, athletes (such as, pitchers, other throwers, and rodeo riders) have a much larger forearm because of muscle and bone hypertrophy on the dominant side.
The examiner should note whether the patient can assume the normal position of function of the elbow (Figure 6-12). A normal functional position is 90° of flexion with the forearm midway between supination and pronation.9 The forearm may also be considered to be in a functional position when slightly pronated, as in writing. From this position, forward flexion of the shoulder along with slightly more elbow flexion (up to 120°) enables the person to bring food to the mouth; supination of the forearm decreases the amount of shoulder flexion necessary to accomplish this. At 90° of elbow flexion, the olecranon process of the ulna and the medial and lateral epicondyles of the humerus normally form an isosceles triangle (Figure 6-13). When the arm is fully extended, the three points normally form a straight line.10 The isosceles triangle is sometimes called the triangle sign. If there is a fracture, dislocation, or degeneration leading to loss of bone or cartilage, the distance between the apex and the base decreases and the isosceles triangle no longer exists. The triangle can be measured on x-ray films.8

Examination
If the history indicates an insidious onset of elbow symptoms, and if the patient has complained of weakness and pain, the examiner may consider performing an examination of the cervical spine, which includes the upper limb peripheral joint scanning examination and myotome testing. Because of the potential referral of symptoms from the cervical spine and the necessity of differentiating nerve root symptoms from peripheral nerve lesions, the consideration of including cervical assessment is essential.
Active Movements
The examination is performed with the patient in the sitting position. As always, active movements are done first, and it is important to remember that the most painful movements are done last. In addition, structures outside the joint may affect range of motion (ROM). For example, with lateral epicondylitis, the long extensors of the forearm are often found to be tight or shortened, so the position of the wrist and fingers may affect movement.
Active elbow flexion is 140° to 150°. Movement is usually stopped by contact of the forearm with the muscles of the arm.
Active elbow extension is 0°, although up to a 10° hyperextension may be exhibited, especially in women. This hyperextension is considered normal if it is equal on both sides and there is no history of trauma. Normally, the movement is arrested by the locking of the olecranon process of the ulna into the olecranon fossa of the humerus. In some cases, under violent compressive loads (e.g., gymnastics, weight lifting), the olecranon process may act as a pivot, resulting in posterior dislocation of the elbow. This mechanism of injury is more likely to occur in someone with elbows that normally hyperextend (Figure 6-14). Loss of elbow extension is a sensitive indicator of intra-articular pathology. It is the first movement lost after injury to the elbow and the first regained with healing. However, terminal flexion loss is more disabling than the same degree of terminal extension loss because of the need of flexion for many activities of daily living (ADLs). Loss of either motion affects the area of reach of the hand, which in turn affects function.

Active supination should be 90° so that the palm faces up. The examiner should ensure that the shoulder is not adducted further in an attempt to give the appearance of increased supination or to compensate for a lack of sufficient supination (Figure 6-15).11
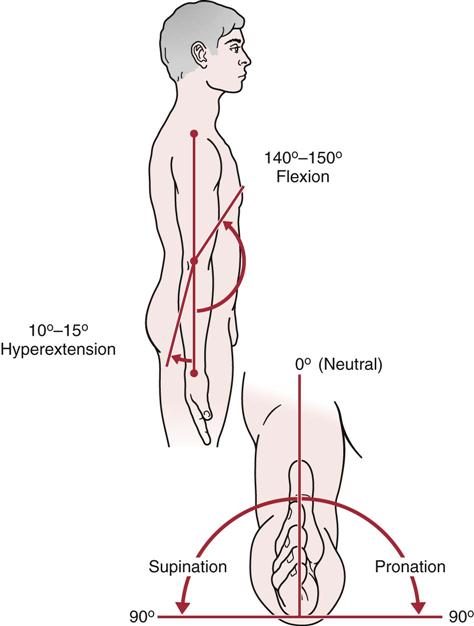
 Figure 6-15 Range of motion (ROM) at the elbow.
Figure 6-15 Range of motion (ROM) at the elbow.For active pronation, the ROM is approximately the same (80° to 90°) so that the palm faces down. The examiner should be sure that the patient does not abduct the shoulder in an attempt to increase the amount of pronation or to compensate for a lack of sufficient pronation.11 However, for both supination and pronation, only about 75° of movement occurs in the forearm articulations. The remaining 15° is the result of wrist action.
If, in the history, the patient has complained that combined movements, repetitive movements, or sustained positions cause pain, these specific movements should be included in the active movement assessment. If the patient has difficulty or cannot complete a movement, but it is pain free, the examiner must consider a severe injury to the contractile tissue (rupture) or a neurological injury, and further testing is necessary.
Passive Movements
If the ROM is full on active movements, overpressure may be gently applied to test the end feel in each direction. If the movement is not full, passive movements should be carried out carefully to test the end feel and to test for a capsular pattern.
It should be pointed out that although tissue approximation is the normal end feel of elbow flexion, in thin patients the end feel may be bone to bone as a result of the coronoid process hitting in the coronoid fossa. Likewise, in thin individuals, pronation may be bone to bone.
In addition to the end feel tests during passive movements, the examiner should note whether a capsular pattern is present. The capsular pattern for the elbow complex as a whole is more limitation of flexion than extension.
In some cases, the examiner may want to determine whether muscles crossing the elbow are tight. If the muscles are tight, the end feel will be a muscle stretch, and ROM at one of the joints that the muscle passes over will be restricted (usually the joint that is the last to be stretched). If the muscle is normal, the end feel will be the normal joint tissue stretch end feel and the ROM will be normal. To test biceps length (Figure 6-16, A), the patient is placed in supine with the shoulder to be tested off the edge of the bed. The shoulder is passively extended to end range and then the elbow is extended.12 Normally, elbow extension should be the same as that seen with active movement.

A, Biceps. B, Triceps. C, Long wrist extensors. D, Long wrist flexors.
To test triceps length (Figure 6-16, B), the patient is placed in sitting. The examiner passively forward flexes the arm to full elevation while the elbow is in extension. The elbow is then passively flexed.9 Normally, elbow flexion should be similar to that seen with active movement.
To test the length of the long wrist extensors (as one would want to do with lateral epicondylitis), the patient is placed in supine lying with the elbow extended (Figure 6-16, C). The examiner passively flexes the fingers and then flexes the wrist.12 Normally, wrist flexion and finger flexion should be the same as found with active movement.
To test the length of the long wrist flexors (Figure 6-16, D), the patient is placed in supine lying with the elbow extended. The examiner passively extends the fingers and then the wrist.12 Normally, wrist extension and finger extension should be the same as that found with active movement.
Resisted Isometric Movements
For proper testing of the muscles of the elbow complex, the movement must be resisted and isometric. Muscle flexion power around the elbow is greatest in the range of 90° to 110° with the forearm supinated. At 45° and 135°, flexion power is only 75% of maximum.9 Isometrically, research shows that men are two times stronger than women at the elbow; extension is 60% of flexion, and pronation is about 85% of supination.13 To perform the resisted isometric tests, the patient is seated (Figure 6-17 ). If the examiner finds that a particular movement or movements cause pain, Table 6-1 can be used to help differentiate the cause. Carrying out wrist extension and flexion is also necessary, because a large number of muscles act over the wrist as well as the elbow.
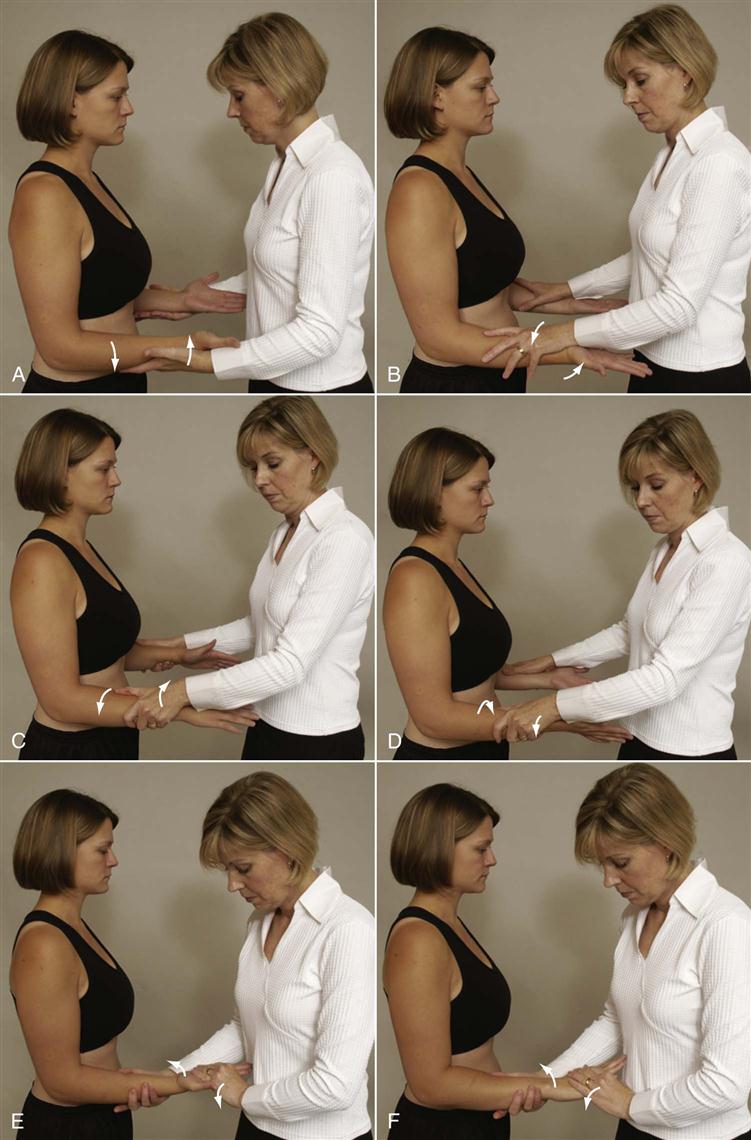
 Figure 6-17 Positioning for resisted isometric movements.
Figure 6-17 Positioning for resisted isometric movements.A, Elbow extension. B, Elbow flexion. C, Forearm supination. D, Forearm pronation. E, Wrist flexion. F, Wrist extension.
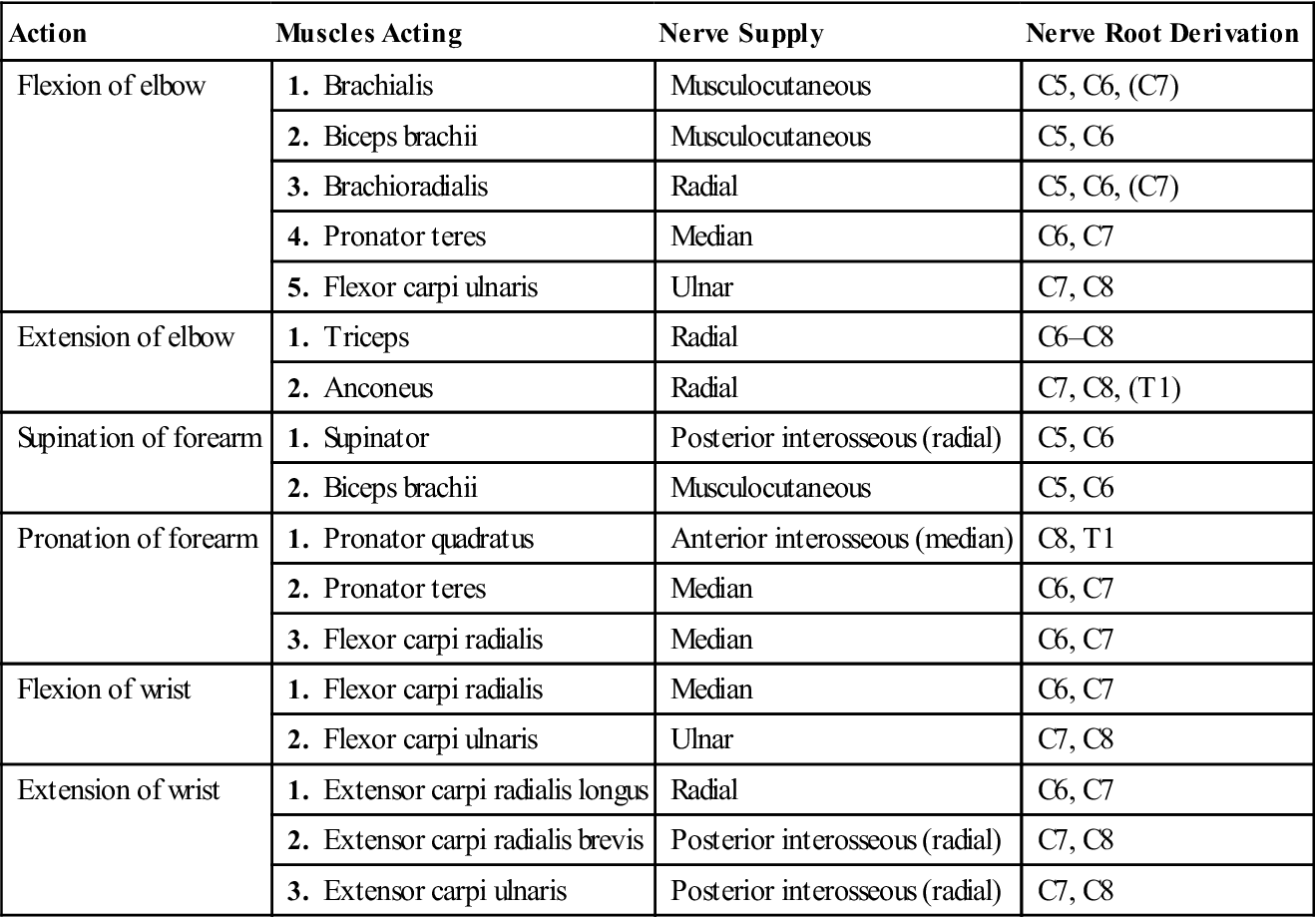
Table 6-1
Muscles about the Elbow: Their Actions, Nerve Supply, and Nerve Root Derivation
| Action | Muscles Acting | Nerve Supply | Nerve Root Derivation |
| Flexion of elbow | 1. Brachialis | Musculocutaneous | C5, C6, (C7) |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| 3. Brachioradialis | Radial | C5, C6, (C7) | |
| 4. Pronator teres | Median | C6, C7 | |
| 5. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Extension of elbow | 1. Triceps | Radial | C6–C8 |
| 2. Anconeus | Radial | C7, C8, (T1) | |
| Supination of forearm | 1. Supinator | Posterior interosseous (radial) | C5, C6 |
| 2. Biceps brachii | Musculocutaneous | C5, C6 | |
| Pronation of forearm | 1. Pronator quadratus | Anterior interosseous (median) | C8, T1 |
| 2. Pronator teres | Median | C6, C7 | |
| 3. Flexor carpi radialis | Median | C6, C7 | |
| Flexion of wrist | 1. Flexor carpi radialis | Median | C6, C7 |
| 2. Flexor carpi ulnaris | Ulnar | C7, C8 | |
| Extension of wrist | 1. Extensor carpi radialis longus | Radial | C6, C7 |
| 2. Extensor carpi radialis brevis | Posterior interosseous (radial) | C7, C8 | |
| 3. Extensor carpi ulnaris | Posterior interosseous (radial) | C7, C8 |
If, in the history, the patient has complained that combined movements under load, repetitive movements under load, or sustained positions under load cause pain, the examiner should carefully examine these resisted isometric movements and positions as well, but only after the basic movements have been tested isometrically. For example, the biceps is a strong supinator and flexor of the elbow, but its ability to generate force depends on the position of the elbow. The biceps play a greater role in elbow flexion when the forearm is supinated than when it is pronated. At 90° of elbow flexion, biceps makes its greatest contribution to supination.14 If the history indicates that concentric, eccentric, or econcentric movements have caused symptoms, these movements should also be tested with load or no load, as required.
If the resisted isometric contraction is weak and pain free, the examiner must consider a major injury to the contractile tissue (third-degree strain) or neurological injury. For example, weakness of elbow flexion and supination may occur with a rupture of the distal biceps tendon, especially if these findings follow a sudden sharp pain in the antecubital fossa when an extension force is applied to the flexing elbow.14 If there is no history of trauma, the most likely cause is neurological, either a nerve root or peripheral nerve lesion. By selectively testing the muscles and sensory distribution (Table 6-2) and by having a knowledge of nerve compression sites (see the “Reflexes and Cutaneous Distribution” section), the examiner should be able to determine the neurological tissue injured and where the injury has occurred.
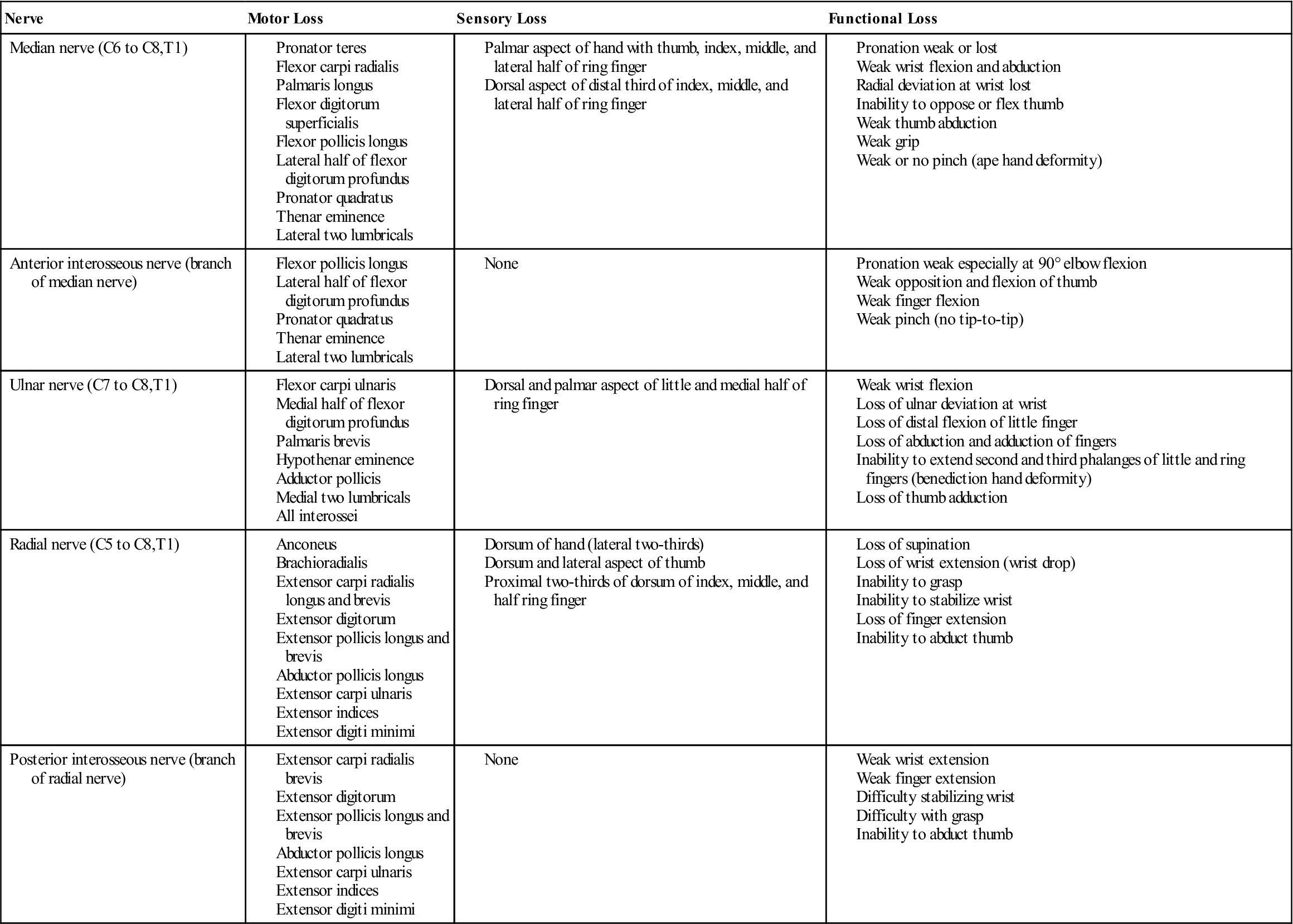
Table 6-2
Nerve Injuries About the Elbow
Functional Assessment
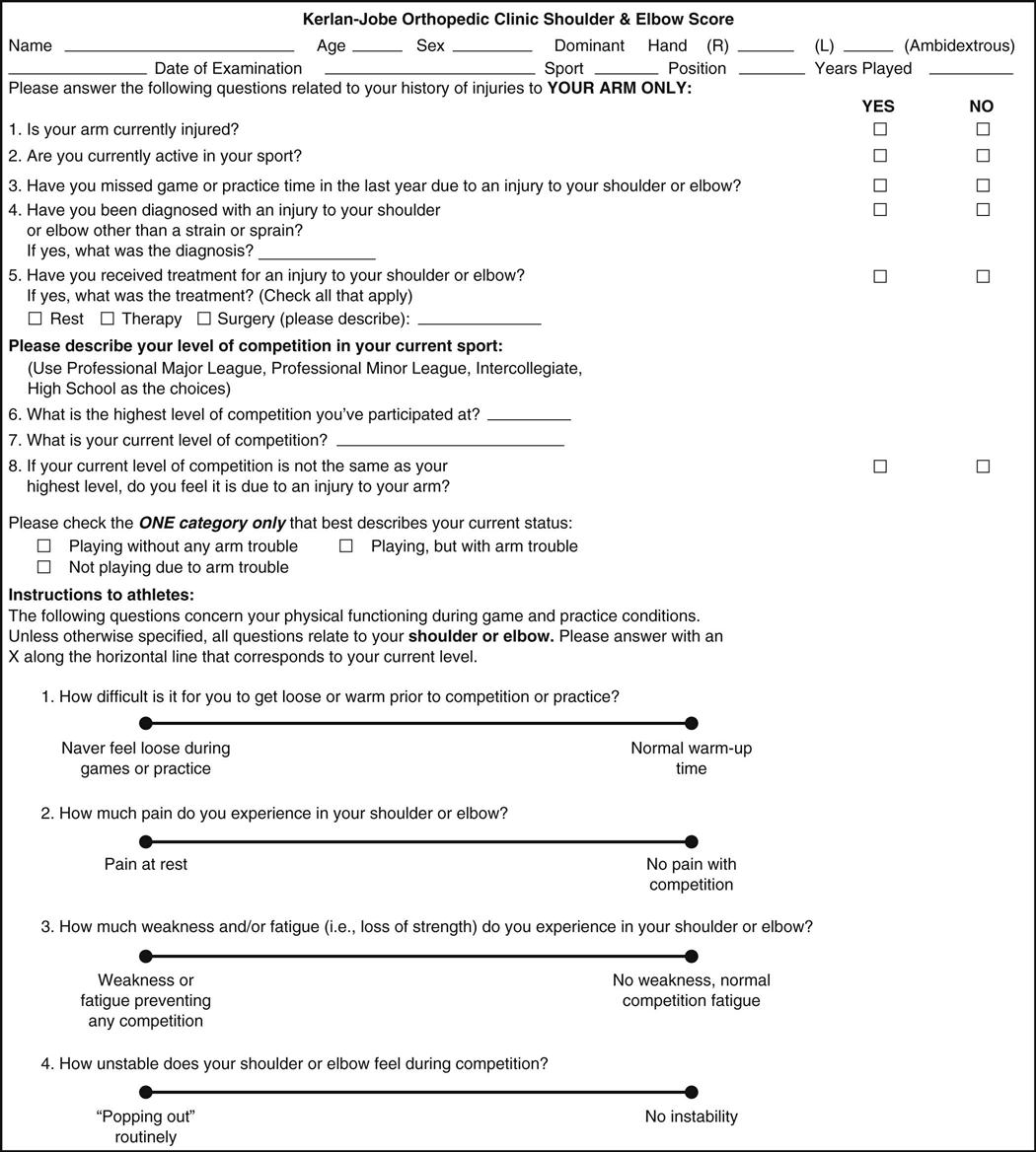
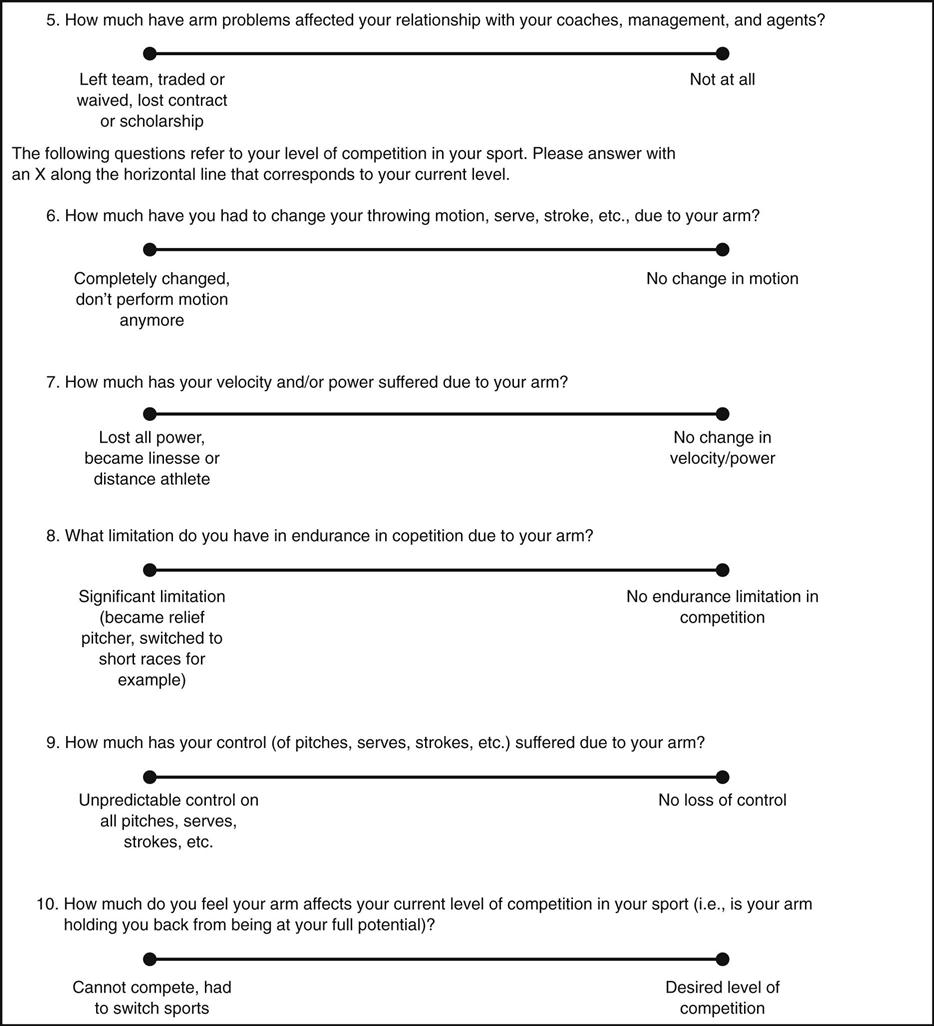
When assessing the elbow, it is important to remember that the elbow is the middle portion of an integral upper limb kinetic chain. It allows the hand to be positioned in space, helps stabilize the upper extremity for power and detailed work activities, and provides power to the arm for lifting activities.15 Motion in the elbow allows the hand to be positioned so that daily functions can be performed easily. Thus, functionally, the elbow is often one part of a functional assessment that may also involve the shoulder and/or hand. This is especially true for athletes who put several joints in the kinetic chain under stress at the same time. For example, the Kerlan-Jobe Orthopaedic Clinic (KJOC) shoulder and elbow score (Figure 6-18 ) is a function score that is designed to look at a functional outcome score involving the shoulder and elbow in overhead athletes.16,17
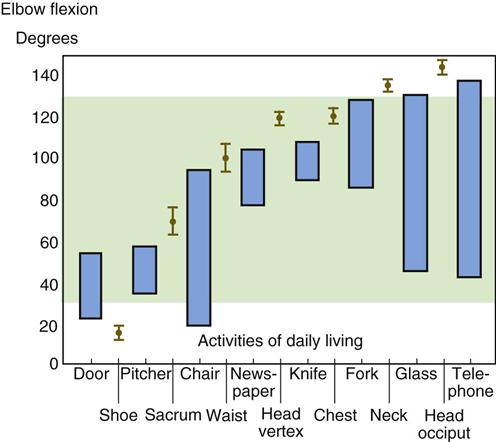
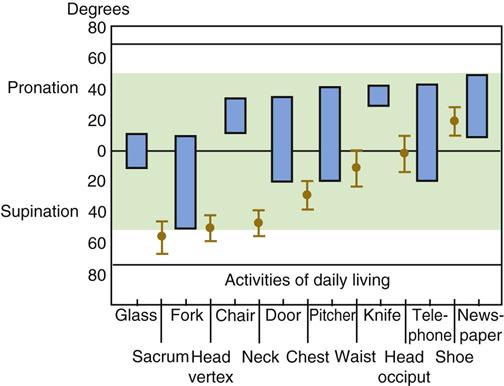
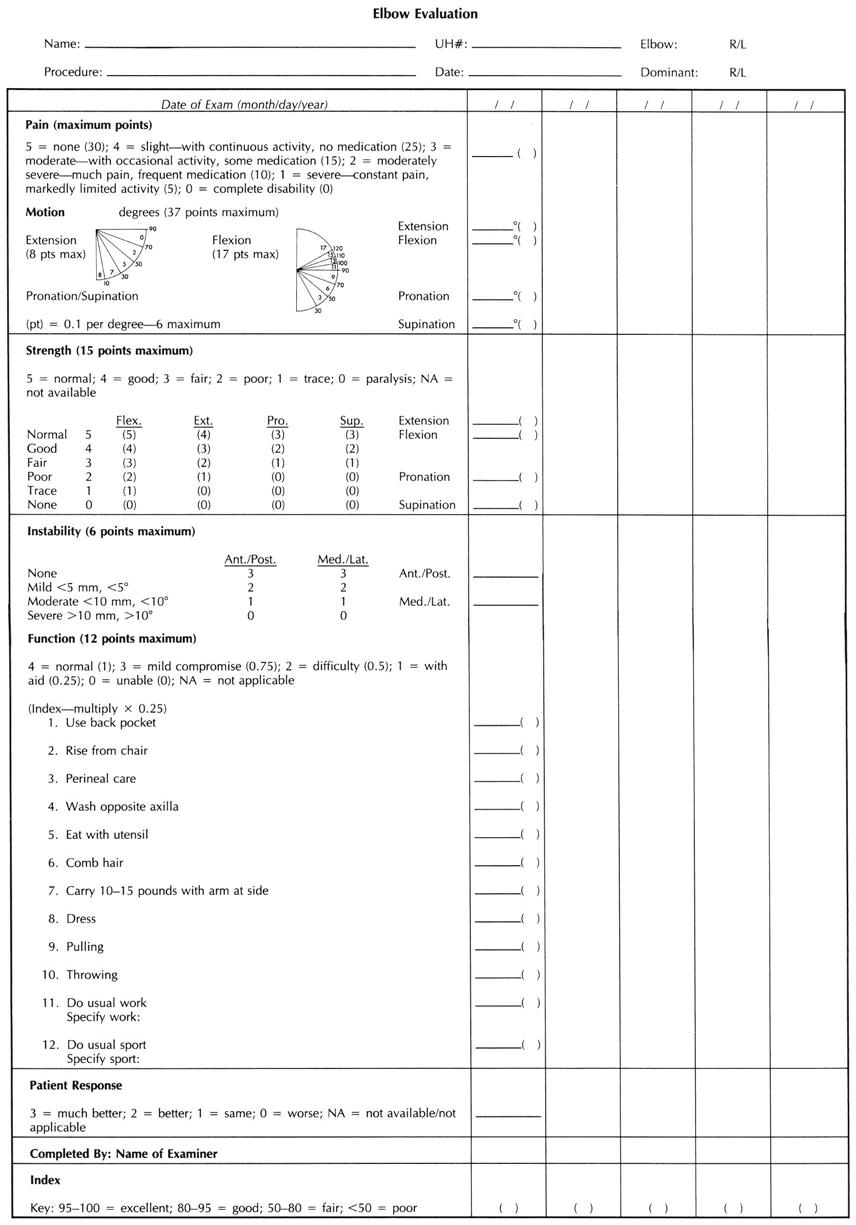
The full range of elbow movements is not necessary to perform these activities; most ADLs are performed at between 30° and 130° of flexion and between 50° of pronation and 50° of supination (Figures 6-19 and 6-20). To reach the head, approximately 140° of flexion is needed. The activities of combing or washing the hair, reaching a back zipper, and walking with crutches require a greater ROM. Activities, such as pouring fluid, drinking from a container, cutting with a knife, reading a newspaper, and using a screwdriver, require an adequate range of supination and pronation. Figures 6-21 and 6-22 show the ROM or arc of movement necessary to do certain activities or the ROM needed to touch parts of the body. Examiners must remember that elbow injuries may preclude lifting objects as light as a cup of coffee, owing to lifting mechanics. Because of the length of the lever arm of the forearm when the elbow is at 90°, loads at the hand are magnified tenfold at the elbow.18 Figure 6-23 is a numerical scoring assessment form that can be used to assess the elbow and includes an important functional component. Table 6-3 demonstrates functional tests of strength for the elbow.
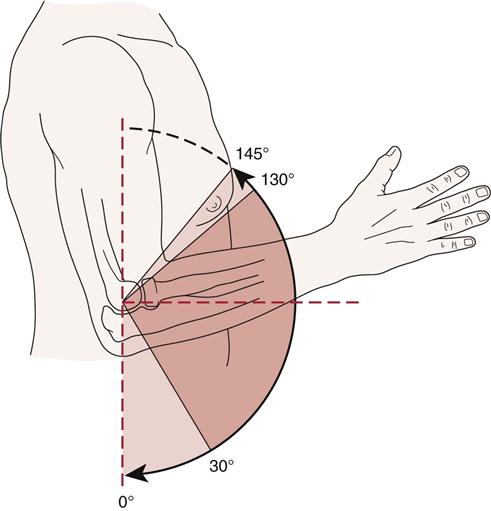
However, the functional arc of motion is somewhat less, and most activities can be performed with flexion of 30° to 130°. (Redrawn from Regan WD, Morrey BF: The physical examination of the elbow. In Morrey BF, editor: The elbow and its disorders, ed 2, Philadelphia, 1993, WB Saunders, p. 81.)
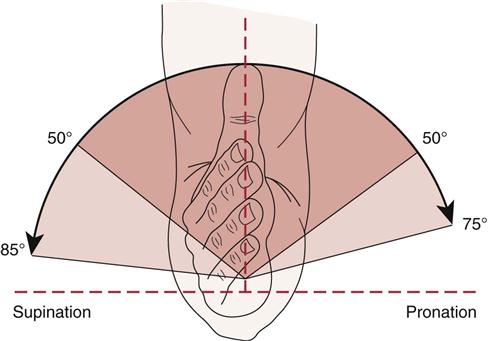
Most activities of daily living (ADLs), however, can be accomplished with 50° of each motion. (Redrawn from Regan WD, Morrey BF: The physical examination of the elbow. In Morrey BF, editor: The elbow and its disorders, ed 2, Philadelphia, 1993, WB Saunders, p. 81.)
Table 6-3
Functional Testing of the Elbow
| Starting Position | Action | Functional Test* |
| Sitting | Bring hand to mouth lifting weight (elbow flexion) | |
| Standing 90 cm from wall, leaning against wall | Push arms straight (elbow extension) | |
| Standing, facing closed door | Open door starting with palm down (supination of arm) | |
| Standing, facing closed door | Open door starting with palm up (pronation of arm) |
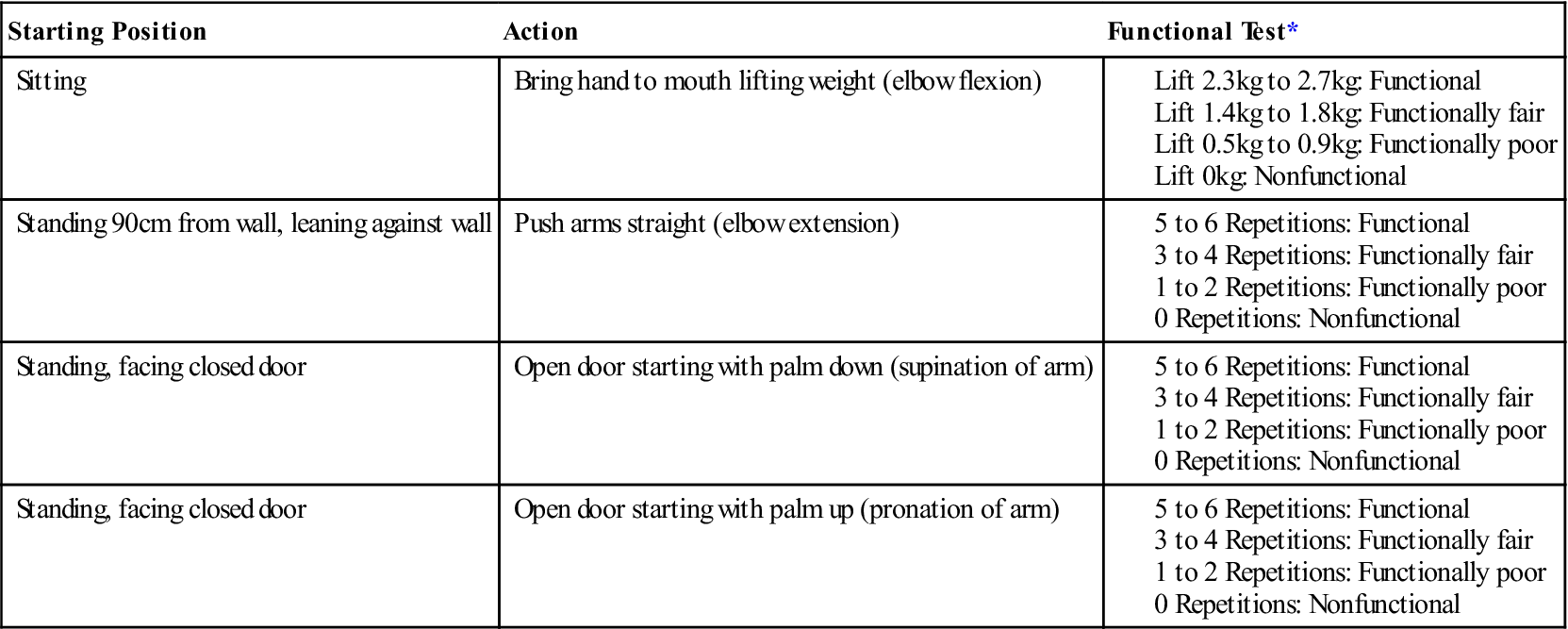
*Younger patients should be able to lift more (2.7 kg to 4.5 kg) more often (6 to 10 repetitions). With age, weight and repetitions decrease.
Data from Palmer ML, Epler M: Clinical assessment procedures in physical therapy, Philadelphia, 1990, JB Lippincott, pp. 109–111.
Special Tests
An examiner should perform only those special tests that have relevance or will help to confirm the diagnosis. If the history has not indicated any trauma or repetitive movement that could be associated with problems, the examiner, depending on the age of the patient, may want to include some of the nerve root compression tests (see Chapter 3) to rule out the possibility of referred symptoms from the cervical spine or the possibility of a “double crush” injury.
For the reader who would like to review them, the reliability, validity, specificity, sensitivity, and odds ratios of some of the special tests used in the elbow joint are available on the Evolve website.
APPENDIX 6-1
Reliability, Validity, Specificity and Sensitivity of Special/Diagnostic Tests Used in the Elbow
| COMBINED PRESSURE AND FLEXION PROVOCATIVE TEST | ||
| Specificity | Sensitivity | |