
Fig. 22.1
(a) A 47-year-old female was caught between two cars, with crushing injury of the left thigh (IIIb open 33.A3 with bone loss). On day 1, the patient underwent a washout and debridement of the wound with application of a knee-spanning external fixator. (b) On day 3, the patient had further washout and open reduction with internal fixation with lateral bridging locking plate (LISS plate). The medial wound was partially closed, with application of vacuum dressing. Ex-fix was reapplied at the end of the procedure until complete closure of the wound with secondary skin graft. Seven months later, the patient underwent bone grafting with the RIA system (harvesting from contralateral femur) to address the bone defect, combined with an open arthrolysis of quadriceps tendon adhesions. (c) Eighteen-month follow-up X-rays show that the bone defect has bridged and an acceptable clinical function with extension/flexion of 0/0/110°
Screw Fixation
The isolated screw fixation is the ideal treatment for unicondylar fractures (B-fractures). However, in complex fracture patterns in elderly patients with osteoporosis, the screw fixation might not be sufficient because of the increased strength of the osteoporotic bone. In these cases, additional plate fixation methods are necessary to stabilize or buttress the condyle.
Plate Fixation
Plate fixation methods of distal femur fractures can be used in extraarticular as well as intraarticular fractures. The surgical approaches for plate insertion depend on whether an articular fracture requires open reduction. In extraarticular fractures and fractures with simple articular involvement, a lateral approach to the distal femur is used. Reduction is usually performed indirectly. Larger fragments can be reduced with a Kirschner wire. Especially with multifragmentary A3 fractures, the temporary use of an external fixator or distractor to correct axial alignment and to control the rotation may be required. For displaced intraarticular fractures, a parapatellar approach is recommended to ensure an optimal overview of the articulation.
The articular reconstruction is mostly secured with independent 3.5-mm lag screws, or in simple articular fractures occasionally with large cannulated screws. The stabilization of the metaphyseal fractures extension is preferably achieved with angle-stable implants such as condylar blade plate, dynamic condylar screw (DCS), or locking plates. Despite the advantages of internal fixation, all the devices have disadvantages. Blade plates are technically demanding and require an invasive insertion technique, and the implantation of DCS removes a large amount of distal bone stock.
Locking plates are easier to handle and have overcome the disadvantages of the older plates. These more modern plates have multiple fixed-angle screws providing a good stability – especially in more complex fracture patterns or in osteoporotic bone structure. Most of the locking plates can be used with insertion guides to allow minimally invasive surgical technique with closed indirect reduction of metaphyseal fragments.
The advantages of the locking plates compared to the DCS and the blade plate leads to a favorable use of the locking plates for the treatment of distal femur fractures.
Locking Plates (Internal Fixators)
Locking plates are angle-stable systems that differ fundamentally from conventional plates. The advantage of locked plates is the permanent angle stability with a low risk of screw loosening leading to a secondary loss of reduction. The locking mechanism furthermore facilitates a minimally invasive surgical technique and the preservation of cortical perfusion, while not using compression forces under the plate. The angular stability is guaranteed by the precisely fitting threaded connection between screw head and plate hole [17–19].
The stability of the conventional plate fixation is generated by friction under the plate. The friction force depends on the friction coefficient of the plate pressure, caused by the screw force acting in an axial direction. Thus, in conventional plate fixation with axial extension, a cross-loading of the bone and a longitudinal stress on the screws will occur. With locked plating, the longitudinal forces are transferred through the angle screws as shear forces on the bones and a friction fit is no longer necessary. The result is that most of the cortical blood flow remains undisturbed. This concept is a longitudinal stress of the bone [20].
Specially developed locking plate systems for the distal femur are broadly available, combining angular stability and options for percutaneous plating/screw placement. The LISS (Less Invasive Stabilization System), as the first available system, consists of preformed plates according to the anatomy of the distal femur, ranging up to 19 holes in length. Using the insertion handle, the LISS plate can be implanted minimally invasively, while it acts also in combination with a trocar system for percutaneous insertion of the self-drilling and -tapping locking screws.
In preoperative planning, the implant length is determined, and following the biomechanical principles of bridge plating, the implant is chosen to be rather long. The length of metaphyseal screws as well as bicortical screws in the shaft is directly measured.
A meta-analysis of 268 fractures showed an average infection rate of 3.3 %, a rate of delayed fracture healing and nonunion of 2.4 %, and a rate of implant failure of 5.9 % when using locked plates [17, 21, 22] (Fig. 22.2).


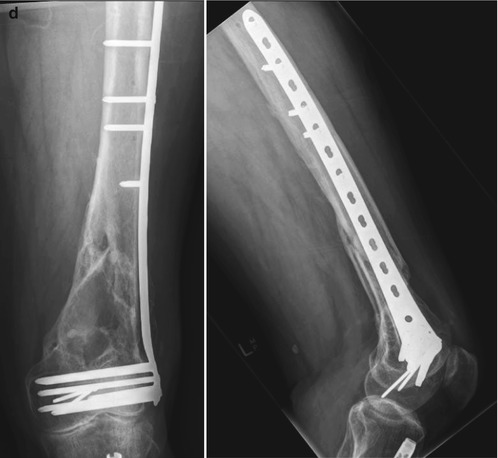


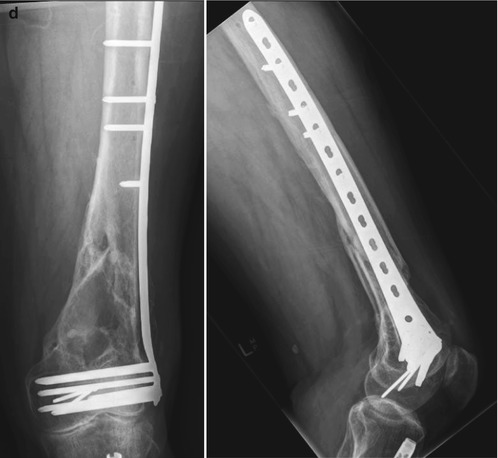
Fig. 22.2
A 72-year-old male had a collision as a pedestrian versus MVA. He sustained a closed 33.C3 distal femur fracture and an ipsilateral midshaft tibia shaft fracture in addition to chest trauma (a). Initial management with an external fixator (b). Intramedullary nailing for the tibia fracture and a minimally invasive stabilization with a locked plate after open reduction of the joint and fixation with 3.5-mm screws. The patient had sustained previously an intertrochanteric femur fracture, and a dynamic hip screw had to be removed to obtain sufficient proximal plate fixation (c). One-year follow-up X-rays demonstrate good callus healing without further intervention (d)
Intramedullary Nailing
Antegrade and retrograde femoral nails can be used for the treatment of distal femoral fractures, depending on the size of the distal fragment. In most cases, retrograde nailing is the first choice for the treatment of distal femur fractures when considering nailing. Advantages of retrograde intramedullary nailing include minimally invasive insertion techniques, decreased blood loss, easier patient positioning for the procedure, and a more reliable locking in the distal fragment than with antegrade nailing. An advantage of nailing distal femur fractures is less frequent irritation of the iliotibial band compared with extramedullary devices.
Despite the benefit that the nail sits central in the axis of the bone, a biomechanical disadvantage is the lower rotational stability of nails compared with extramedullary angular stable implants. Nevertheless, the lower rotational stability appears to be sufficient for postoperative neutralization of torsional forces, considering the good clinical experience with intramedullary stabilization of femoral shaft fractures [23]. Furthermore, intramedullary nails have limited use in C3 multifragmentary articular fractures and in the case of periprosthetic distal femur fractures [24, 25].
Most interlocking nails, by design, achieve rotational stability in the sagittal plane by introducing two distal locking screws, or special locking options like spiral blades in retrograde nails. However, stabilization can be quite challenging in short distal fragments.
Antegrade Technique
Antegrade intramedullary nailing of distal femoral fractures is a rare indication. Standard implants are used, and the indication for extra-articular fractures is limited to those in which the fracture line is at least 4–5 cm proximal to the former growth plate (basically rather distal femoral shaft fractures) [26]. The indication for antegrade nailing was extended by some authors to intraarticular fractures of the distal femur [27, 28]. Intraarticular fractures are reconstructed anatomically according to the articular surface and stabilized with lag screws and a nail placed in a standard antegrade technique. The known general problems of antegrade nailing, such as Trendelenburg limp and heterotopic ossification at the insertion site, join the problematic alignment of the distal fragment. In an analysis of 57 cases of antegrade intramedullary nailing of distal femoral fractures, the infection rate was 0 %, the delayed healing of bone fractures 3.5 %, 0 % nonunion rate, and the rate of implant failure was 3.5 % [27, 28].
Retrograde Technique
Intramedullary nailing of distal femoral fractures is mostly performed in the retrograde nailing technique [29]. For retrograde nailing today, a multitude of different implants are available, differing in material and design (especially regarding the locking options).
The retrograde intramedullary nailing can be performed minimally invasively and allows, in contrast to antegrade nailing, the direct visualization of the articular surface. Indications for retrograde nailing are extraarticular distal femur fractures and simple (C1 or C2) intraarticular fractures of the femur, allowing a double distal locking. A problem is the retaining force of the distal locking screws, which can lead to a loosening in osteoporotic bone. This loosening occurs in about 8 % of cases [23, 30]. The holding force of the distal locking screws could be increased by a modified geometric arrangement of the screws, through the introduction of a spiral blade, and with fixed-angle distal clamping [31]. Other potential problems occurring with the retrograde femoral nailing technique include heterotopic ossification, fractures of the locking pin, adhesion-related limitations of range of motion, swelling of the knee joint, and symptomatic, prominent distal locking bolts [4, 23, 31].
An analysis of 344 distal femur fractures that were treated with retrograde nailing showed an infection rate of 0.3 %, a delayed healing rate of 4.7 %, a nonunion rate of 2 %, and an implant failure rate of 8.4 % [32–36]. Rotational deformities were found in 8.3 % and deformities in the frontal plane in 3.2 % of cases (Figs. 22.3 and 22.4).







Fig. 22.3
A 42-year-old female patient with floating left knee injury (IIIb open C3 distal femur fracture with bone loss and closed 42.B2 tibia fracture). Initial stabilization in a regional hospital with nailing of both fractures on the day of admission (a). Presentation to our output clinic 6 weeks postsurgery with ongoing pain and loosening of the distal locking bolts (b). Removal of nail and restabilization with a locking plate. The bone defect was simultaneously bridged with cortical bone struts harvested from the pelvis (c). After 6 months, regrafting of the proximal (shaft) section. Solid consolidation 1 year postsurgery with good, stable function of the leg; clinical pictures from two different time points (d)

Fig. 22.4
Distal femur fracture after an accident (AO-Classification C 2). X-rays of the day of accicdent (a, b). Reconstruction of articular bone block with a lag screw and distal femoral nail. The x-ray 6 weeks postoperatively show a good reduction with beginning bone healing (c, d)
22.5.2.4 Postoperative Care and Rehabilitation
The follow-up treatment of distal femur fractures needs to be adjusted to the individual fracture situation, the surgical treatment, the implants being used, the concomitant injuries, and the cooperation of the patient. The wounds should be checked regularly and the suture materials should be removed after about 12 days post operation. After every operation, an X-ray examination in two planes should be performed for the purposes of documentation and legal formality. The surgeon should keep records about the maximum range of motion, the degree of weight bearing, and the need for additional support (e.g., ortheses). Special attention should be paid to thrombosis prophylaxis and providing sufficient pain medication to allow post-operative rehabilitation. On the day after the operation, treatment with active and passive physiotherapy (continuous passive motion, CPM) should immediately start, to reduce the risk of adhesions, support the cartilage healing, and to help to reduce the swelling [37]. It is particularly important to gain the full knee extension back early on. The CPM treatment should be performed frequently, until the patient becomes mobile. Depending on the fracture type, patients will partially weight bear for 6–12 weeks. Extraarticular fractures need partial weight bearing for 6–8 weeks, whereas complex intraarticular fractures might need partial weight bearing for up to 12 weeks. Depending on the radiological signs of bone healing, the weight bearing can be increased stepwise. In general, the postoperative management should include individual circumstances and must be well explained to the patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








