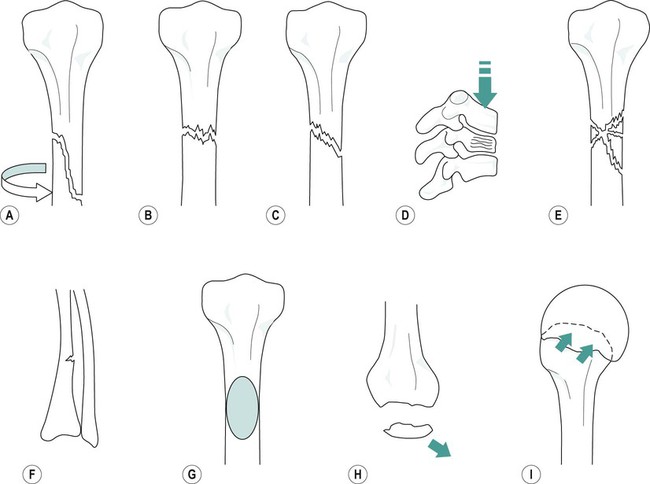
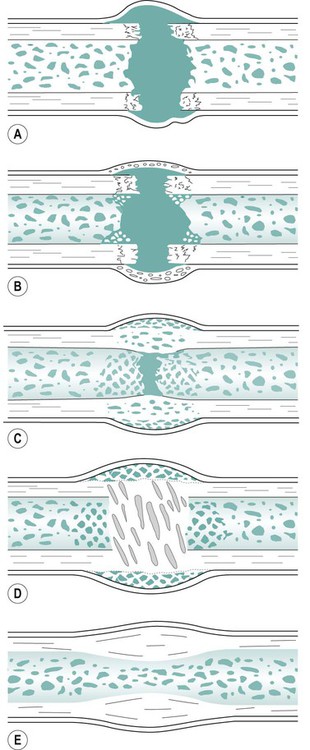
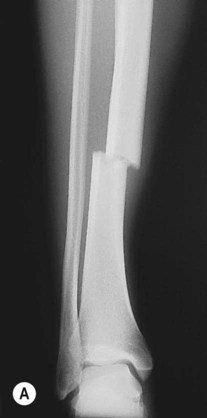
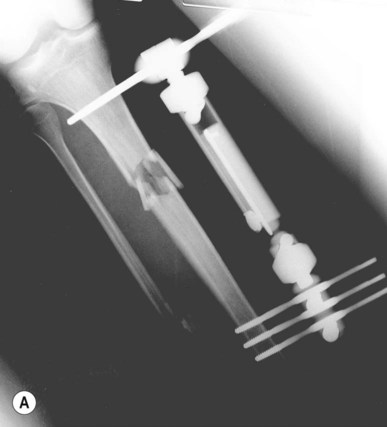
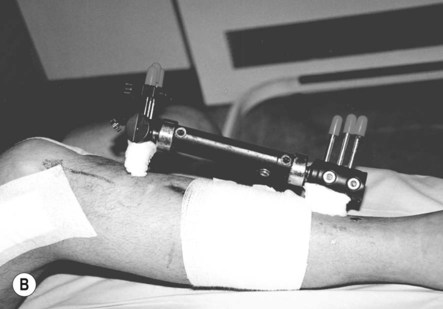
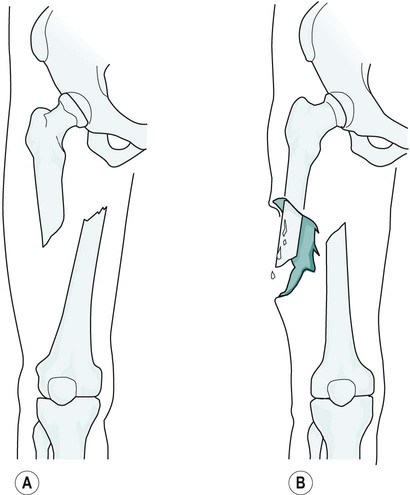
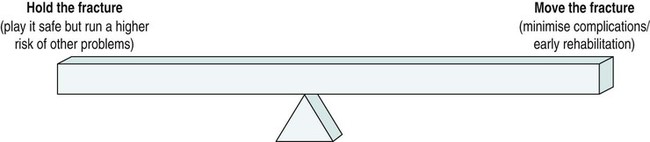
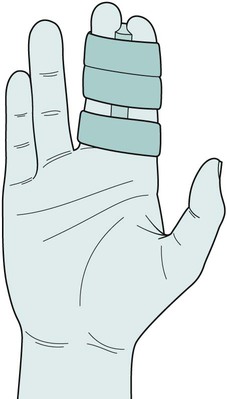
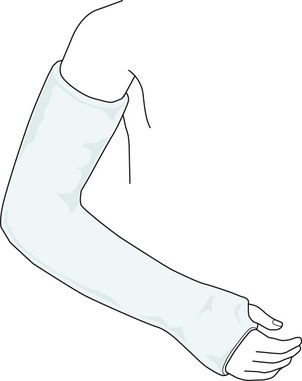
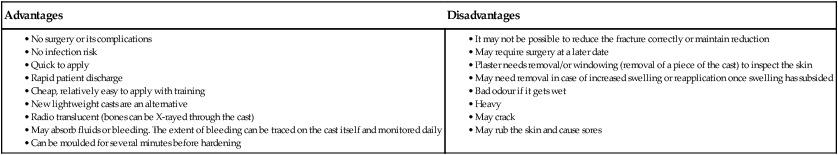
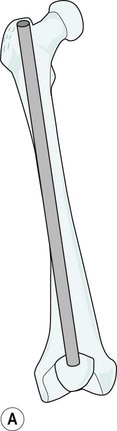
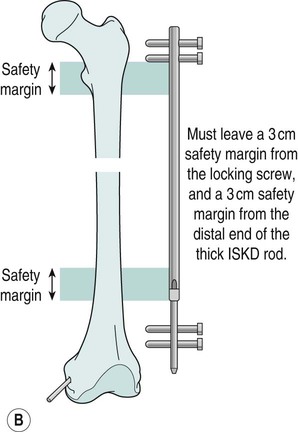
the Executive Committee of the Association of Orthopaedic Chartered Physiotherapists Fractures may be classified as open or closed (Figure 22.1). Open or compound types of fracture occur when the bone-end or some other object has pierced the skin. These fractures are an additional cause for concern because of the possibility of the introduction of microorganisms, leading to bone infection (osteomyelitis). With closed fractures the skin remains intact. Another common classification includes displaced or un-displaced. Figure 22.2 shows some further classifications. Spiral fractures commonly occur from a twisting injury. A direct blow could give a transverse or oblique fracture depending on the angle of the force and whether the limb is fixed or moving at the time of the trauma. Longitudinal forces tend to result in compression or crush fractures. In some cases there are a number of fragments of bone and this is termed a ‘comminuted’ fracture (not to be confused with ‘compound’). Loose fragments of bone are known as ‘butterfly fragments’. Wolff’s law states that bone responds to the stresses that are imposed upon it by rearranging its internal architecture to best withstand the stresses. In other words, bone is laid down where it is needed and absorbed where it is not. It is important to understand this concept when dealing with people who have sustained fractures. Bone is a living tissue, not the brittle, chalky specimens that students may be familiar with. It is continually in a dynamic equilibrium of growth and reabsorption. Figure 22.3 shows the process of fracture healing in compact bone taken through five stages. The time it takes for a fracture to unite depends on a number of factors. • Type of bone. Cancellous bone heals more quickly than compact bone. Healing of long bones depends on their size so that bones of the upper limb unite earlier (3–12 weeks) than do those of the lower limb (12–18 weeks). • Revascularisation of devitalised bone and soft tissues adjacent to the fracture site. • The mechanical environment of the fracture (Marsh and Li 1999). • Classification of the fracture. It is easier to obtain good apposition of bone ends with some fractures than with others. This may depend on the initial position of the fragments before reduction and the effect of muscle pull on the fragments. • Blood supply. Adequate blood supply is essential for normal healing to take place. Certain fractures can be notoriously slow to heal (e.g. fractures of the lower third of tibia). This part of the bone has a poor blood supply owing to the fact that under normal circumstances it does not require one as there is little muscle bulk here, therefore little demand for nutrients and oxygen. • Fixation. Adequate fixation prevents impairment of the blood supply which may be caused by movement of the fragments. It also maintains the reduction thus preventing deformity and consequent loss of function. Interestingly, if a fracture is rigidly immobilised, the stimulus for callus to form is lost, so a small amount of movement at a fracture site actually encourages fracture healing. • Age. Union of a fracture is quicker in children and consolidation may occur at between 4 and 6 weeks. Age makes little difference to union in adults unless there is accompanying pathology. • It has been suggested that certain drugs such as non-steroidal anti-inflammatory drugs may interfere with fracture healing; however, evidence remains inconclusive (Bandolier 2004). • Smoking. There are increased rates of delayed union and non-union in people who smoke who have sustained open tibial fractures (Adams et al. 2001). • Ultrasound. Recent work has suggested that low-intensity ultrasound may accelerate fracture healing (Azuma et al. 2001). Management is difficult. When the lower limb is involved, weight-bearing is encouraged with the help of physiotherapy and pain control aids, such as transcutaneous electrical nerve stimulation (TENS). However, this is minor therapy compared with the use of other treatments such as sympathetic nerve blocks (Viel et al. 1999), vasodilator drugs (e.g. guanethedine) and local analgesia. All of them have variable results. Recovery is slow and may take several months. Oedema may be apparent below the level of the plaster and it is often necessary to elevate the limb, exercise the fingers or toes not encased in plaster, and perform isometric contractions of the muscles within the cast in an attempt to encourage muscle pump activity (Tschakovsky et al. 1996; Sheriff and Van Bibber 1998). Once the plaster has been removed, atrophied muscles may not provide an adequate muscle pump on the veins, in which case swelling may reappear especially after activity or non-elevation. Once a fracture has been diagnosed, the most suitable treatment must be decided upon. This should be the minimum possible intervention that will safely and effectively provide the right environment for healing of the fracture. Interestingly, nature has devised a system by which a slight amount of movement at a fracture site is useful in stimulating callus formation so there is a balance to be made between immobilising a fracture but allowing enough movement to stimulate callus formation and healing (Figure 22.4; Cornell and Lane 1992). Reduction means to realign into the normal position or as near to the normal anatomical position as possible (Figure 22.5). Reduction of a fracture may be either open or closed. Closed reduction means that no surgical intervention is used with the fracture being manipulated by hand under local or general anaesthesia. Open reduction means that the area has been surgically opened and reduced. The objectives of immobilising a fracture are: In some fractures where there is no likelihood of displacement, fixation may not be necessary or minimal fixation will suffice, for example buddy strapping for some finger fractures (Figure 22.6). This is a plaster-impregnated bandage that can be moulded to the part when wet, which sets in time. The standard method of external splinting is still plaster of Paris (Figure 22.7). The advantages and disadvantages of using plaster of Paris are listed in Table 22.1. Table 22.1 The advantages and disadvantages of plaster of Paris It has been found unnecessary to fix some fractures as rigidly as was thought necessary in the past. An example of this is cast (or functional) bracing. Functional braces have hinges to allow movement (see the case study towards the end of the chapter and Figure 22.24). • Surgery inevitably causes additional trauma and potential exposure to microorganisms. • It can convert a closed fracture into an open fracture. • It requires surgery with all its sequelae and potential complications. Ironically, rigid fixation may remove the stimulus for callus formation. The implants are usually left in unless they cause problems e.g. irritation, infection or protrusion. In the young, they will be removed if they will affect growth of the bone. Here, a hollow metal rod is introduced at one end of a long bone, travels down the medullary canal and may be locked with screws distally and proximally (Figure 22.9). The proximal aspect of the nail is threaded and this permits a tool to be threaded onto the nail at a later date for its removal. Figure 22.10 shows fixation of a fractured tibia using an external fixator. Pins or wires are driven into the fragments and held by a piece of apparatus on the outside of the body. Figure 22.11 shows an external fixator for a comminuted intra-articular fracture of the distal radius. Figure 22.12 shows an external fixator for an unstable pelvic fracture.
An introduction to fractures
Definition and classifications
Classification of fractures
Fracture healing
Healing of compact bone
Time for a fracture to unite
Complications of fractures
Growth disturbance
Complex regional pain syndrome I (CRPS I)
Oedema
Principles of fracture management
Reduction
Immobilisation
Common methods of fracture immobilisation
Plaster of Paris
Functional bracing (cast bracing)
Disadvantages of ORIF
Intramedullary nailing
External fixation

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree